What Is Lymphoma?
Lymphoma is a term used to describe the malignant proliferation of lymphoid cells (i.e. B and T lymphocytes). These are the cells that are part of your lymphatic system, the part of the body that aids in the fight against pathogens. The lymphatic system includes the lymph nodes, which are frequently affected in some types of lymphomas. However, extra nodal lymphomas can also occur.
Lymphomas can be categorized into two main subtypes: Hodgkin’s lymphoma (HL) and non-Hodgkin lymphoma (NHL). It is estimated that about 60% of lymphoma cases are NHL. It is important to recognize that different types of lymphomas have differences in terms of risk factors, treatment, and prognosis.

1. Hodgkin Lymphoma
Hodgkin lymphoma (HL) is potentially curable. It is rarely extranodal and can spread to contiguous structures. It can be further classified into several types: nodular sclerosis, mixed cellularity, lymphocyte depleted, lymphocyte rich, and lymphocyte predominant. Nodular sclerosis constitutes approximately 70 percent of Hodgkin lymphomas. In HL, staging is important because it guides therapy. The Ann Arbor classification is often used for staging of the disease.
In stage I, it affects a single lymph node area or a single extranodal site. At stage 2, there is involvement of 2 or more lymph nodes on the same side of the diaphragm. By stage 3, there is involvement of lymph nodes on both sides of the diaphragm. At stage 4, there is multiple involvement or dissemination of lymphoma to extranodal organs.

2. Non-Hodgkin Lymphoma
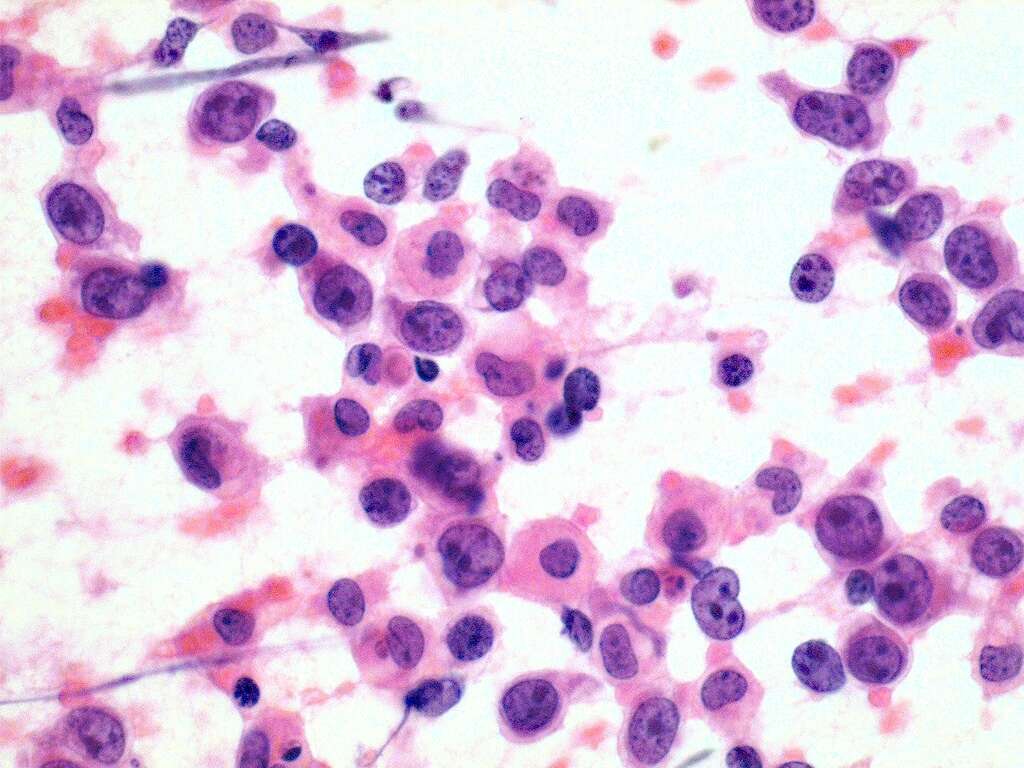
Non-Hodgkin lymphoma (NHL) is the most common type of lymphoma. Like Hodgkin lymphoma, it can also be further divided into several subtypes where each subtype has different features. NHL can be divided according to the type of lymphocyte the lymphoma starts in, how it looks under a microscope, the chromosome features of the cells or the presence of specific proteins on the surface of malignant cells.
Some examples of subtypes are follicular lymphoma, diffuse large cell lymphoma, mantle cell lymphoma, marginal zone lymphoma, and Burkitt lymphoma. Prognosis-wise, NHL can be divided into indolent and aggressive. The various subtypes of NHL help oncologists to predict prognosis and decide which treatment option may be best.

3. Risk Factors
The risk factors for Hodgkin lymphoma are a positive family history (i.e. siblings) and infection with the Epstein Barr virus (one cause of infectious mononucleosis).
HL is most common in young adults and in late adulthood (i.e. after 55 years). Other risk factors include autoimmune diseases (i.e. systemic lupus erythematosus), and a weakened immune system (i.e. patients with AIDS or using immunosuppressant medications).

4. Epidemiology for Hodgkin Lymphoma
In the United States, the National Cancer Institute has reported that the rates of Hodgkin lymphoma (HL) have decreased over the last 10 years. As of 2010-2014, the adjusted incidence has been reported to be 2.6 cases per 100,000 individuals. In Europe, the incidence mirrors the US. In the United Kingdom, estimates show a crude incidence rate of 3.3 cases per 100,000 individuals. Generally, it has been observed that the incidence of HL is higher among males compared to females.
This is most apparent in the pediatric population where 85% of HL cases affect boys. The lowest incidence of HL is found to be among Pacific Islanders and Asians. Age-wise, there seems to be a clear bimodal distribution with the incidences of HL peaking in the ages of 15 to 34 years old and those above the age of 55 years old.

5. Epidemiology of Non-Hodgkin Lymphoma
The American Cancer Society estimated that in 2019, there were about 74,200 new cases of non-Hodgkin lymphoma (NHL). Since the early 1970s, it has been observed that the incidence rates of NHL have almost doubled. However, some of these increased rates can be attributed to improved diagnostic techniques and better medical care.
NHL is the most common hematopoietic neoplasm where it represents about 4.2% out of all cancer diagnoses and is 7th in ranking in terms of frequency among all cancers. Generally, NHL is diagnosed around ages 65 to 74, except small noncleaved lymphomas and high-grade lymphoblastic lymphomas, which are more often observed in young adults and children.

6. Signs and Symptoms
Lymphoma can be present with vague and nonspecific symptoms. The most characteristic presentation of patients with lymphoma is generalized painless lymphadenopathy. This means that the lymph nodes are swollen or abnormal in consistency. Lymphadenopathy is mostly seen in Non-Hodgkin lymphomas, but can also be see in HL. However, it is a nonspecific sign that can also be seen in various other conditions.
Furthermore, some lymphomas express as a nodal mass or extra nodal masses (i.e. cutaneous masses). Other symptoms include B symptoms (systemic symptoms) such as fever and chills, weight loss (unintentional loss of more than 10% of the total body weight over a duration of 6 months or less), and night sweats (drenching sweats at night). B symptoms are more common in Hodgkin lymphoma, which affects mostly young adults. Other symptoms of lymphoma include fatigue, loss of appetite, and shortness of breath.

7. Tests
In lymphoma, the history and physical examination is important but the best treatment option is determined through staging. This means that imaging, biopsy, and the assessment of prognostic factors are required. Tests that can be useful include a complete blood cell (CBC), and blood chemistry studies. Tests for an erythrocyte sedimentation rate, lactate dehydrogenase levels, serum creatinine, alkaline phosphatase, human immunodeficiency virus, and serum levels of cytokines can also help determine prognosis and treatment of choice.
A lymph node biopsy will also help with the diagnosis of lymphoma. This means partial or total excision of the lymph node will be required. It will then be examined under the microscope to reveal histopathological features.

8. Imaging
While staging laparotomy and laparoscopy were once the standard of care in some cases of lymphoma, the use of modern imaging has meant that these procedures are no longer needed.
Imaging studies help to accurately stage lymphoma. This includes those such as X-rays, computed tomography (CT) scans, positron emission tomography (PET) scans, and more. Imaging studies help determine the bulk of the disease that impact prognosis. Although the definition of bulky disease varies, it generally can be defined as a nodal mass more than 10 cm or a mediastinal mass that is 33% or more than the thoracic diameter when measured at the level of the T5/6 vertebrae. Other potentially beneficial scans include a bone scan, ultrasonography, a magnetic resonance imaging (MRI) scan, and a Gallium scan.

9. Hodgkin Lymphoma Treatment
The treatment for HL is specific depending on the type, stage, and assessment of possibility of resistant disease. Although curable, the therapies can lead to significant long-term toxicity. Treatment options include radiation therapy, salvage chemotherapy, induction chemotherapy, and hematopoietic stem cell transplantation.
Follow-up of the patient after complete remission is also recommended for 5 years. It should include lab tests and imaging. Even after 5 years, annual surveillance is recommended.

10. Non-Hodgkin Lymphoma Treatment
The treatment for NHL varies depending on the phenotype, histology, tumor stage, symptoms, age of the patient, comorbidities, and symptoms. Chemotherapy can be usually administered outpatient along with growth factor support. High doses of chemotherapy, bone, or stem cell transplant is done inpatient.
Patients with complications such as infection, dehydration, and side effects of chemotherapy should be admitted for further care. Regular diet and activity continues. However, exposure to other patients with infectious or communicable diseases should be avoided.