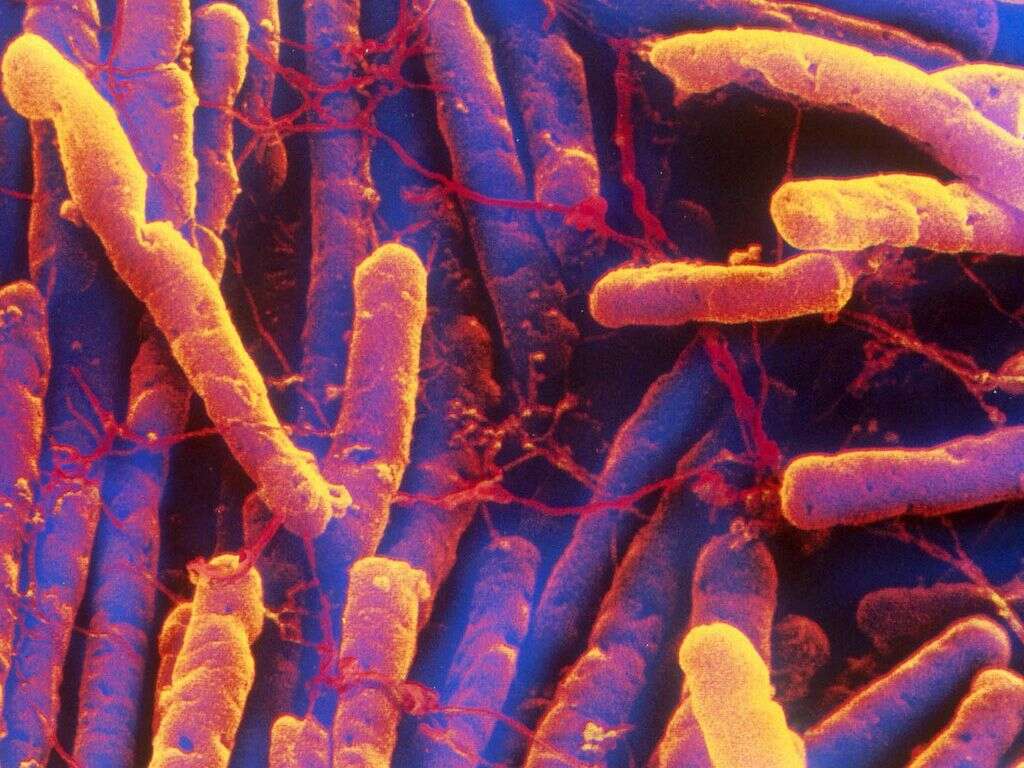
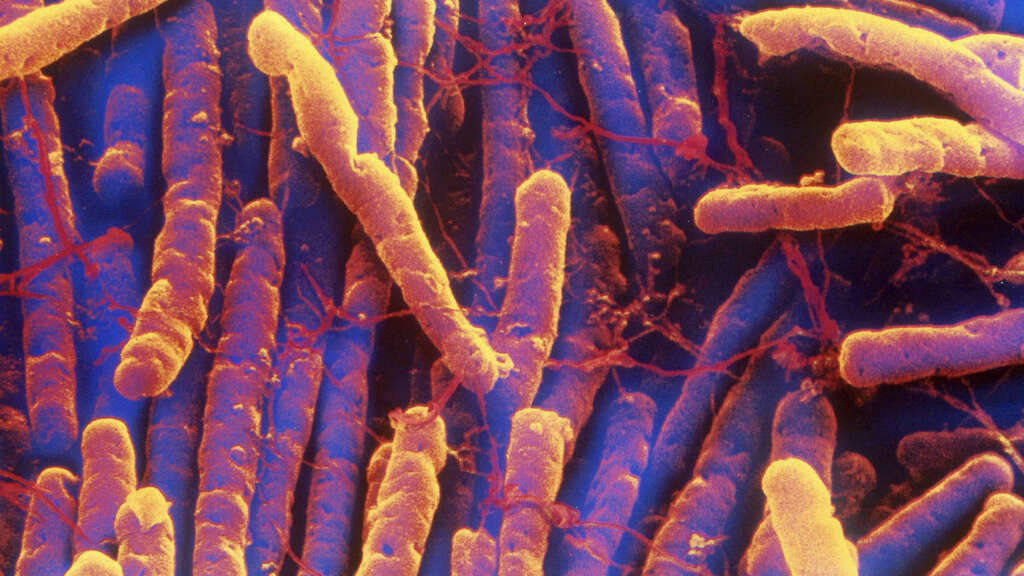
What Is C. Diff?
C. diff infection is an infection caused by the bacterium Clostridioides difficile. This bacteria spreads through bacterial spores that can be found in feces. Transmission occurs when the spores contaminate surfaces or through the hands of other individuals. This infection is responsible for the development of antibiotic-associated colitis and diarrhea.
The C. diff infection often manifests as mild to moderate diarrhea with possible abdominal cramping. It is estimated that 1 in 5 hospitalized patients become colonized with C. diff during their stay with more than 30% developing diarrhea. It is also one of the most common nosocomial infections.

1. Mechanism
A C. diff infection results in the disturbance of the bacterial balance in the colon due to the colonization of the bacterium. The release of toxins also damages the mucosa causing inflammation. There are two types of toxins with toxin A being an enterotoxin while toxin B is a cytotoxin. Both these toxins are able to bind to receptors on the intestinal cells and cause various issues.
In animal model studies, researchers have hypothesized that some intestinal cells that survive toxin B may contribute to the development of inflammatory bowel disease and irritable bowel syndrome due to persistent inflammation and stimulation of preneoplastic (pre-cancerous) cells. The NAP1 strain of C. diff has been associated with the most severe C. diff infections as it results in full blown colitis that is characterized by renal failure, leukocytosis, and toxic megacolon.
2. Risk Factors
One of the risk factors that increases the likelihood of a C. diff infection is exposure to antibiotics. The most commonly implicated antibiotics are the cephalosporins, ampicillin/amoxicillin, fluoroquinolones, and clindamycin. Brief exposure to any single antibiotic can increase the likelihood of C. diff colitis. This risk further increases with the use of two or more antibiotics.
Other medications that have been implicated include proton pump inhibitors and antidepressants. Other risk factors include those with advanced age (more than 60 years), are immunocompromised, severe illness, gastric acid suppression, and hospitalization.

3. Statistics
In the United States, a C. diff infection is commonest among hospitalized patients resulting in about 3 million cases annually. Cancer patients are those who are mainly affected by C. diff infections. There are about 14,000 deaths due to diarrhea caused by C. diff. From 2000 to 2009, the number of patients hospitalized who developed C. diff infections doubled or tripled.
Globally, the incidence and deaths have also rise in Canada and Europe. The global increase is thought to be due to the rising elderly population, resistance to treatment, and more virulent strains of C. diff. These rates are also increasing among hospitalized children, especially those with immunosuppression.

4. Symptoms
A C. diff infection can cause a variety of symptoms. There are some individuals who are asymptomatic while mild cases may experience some diarrhea. Most patients only develop diarrhea during or shortly after they have started antibiotics; 25% to 40% may not even experience symptoms for as long as 10 weeks after the completion of their antibiotic therapy.
Symptoms of a C. diff infection often includes loss of appetite, a general feeling of being unwell, mild to moderate watery diarrhea, fever (in more severe cases), cramping abdominal pain, and rarely diarrhea that is bloody. Due to the diarrhea, the patient may also have symptoms of dehydration, dizziness, fatigue, severe thirst, headaches, confusion, and more.

5. Stool Testing
Testing for a C. diff infection can be done through stool testing only on diarrhea samples. However, testing is not recommended for those without symptoms unless it is done for study purposes. Blood may be present in the stool samples but not to the naked eye. White blood cells are present in approximately 50% of stool samples. To detect C. diff and its toxins, the most sensitive test is a stool culture.
Although a stool culture is the gold standard to test for C. diff infection, it takes a long time to obtain results. This is why the enzyme immunoassay (EIA) is more often used. It is a rapid test but not ideal as it has a lesser sensitivity (will not be able to detect all cases) compared to the stool cytotoxin test.

6. Other Lab Investigations
The white blood cell levels are usually elevated in a C. diff infection. This finding also means that the patient has a poorer prognosis. Since C. diff patients are prone to acute kidney injury, serum creatinine levels should also be measured in those with a C. diff infection. Both an elevated white blood cell count and higher serum creatinine levels means that the infection is severe and oral antibiotics should be prescribed.
Severe cases of C. diff infection can cause dehydration, electrolyte imbalance, and hypoalbuminemia (low albumin level). In these cases, electrolyte levels and albumin levels should be monitored. Serum lactate levels should be tested for patients requiring surgical intervention. Measuring biomarker levels can also be useful to distinguish colonization and disease.

7. Medical Imaging
Endoscopy is not usually recommended for a C. diff infection. However, this may help demonstrate the presence of yellowish white plaques that are raised on a red and swollen mucosa. These plaques are known as pseudomembranes and can be seen in 14% to 25% of those with mild disease while it can be observed in 87% of patients who have a full-blown disease.
In some cases, endoscopy is contraindicated as it increases the risk of perforation. An abdominal computed tomography (CT) scan is recommended by the American College of Radiology as the imaging of choice for a C. diff infection involving the colon. It can help identify irregularity of the bowel wall, ascites, megacolon, and more.

8. Treatment and Management
This organism is present in 2% to 3% of healthy adults and 70% of healthy infants. Asymptomatic individuals do not require treatment. Severe cases will require oral vancomycin as it helps resolve symptoms faster and results in less treatment failures. Oral metronidazole is recommended for mild to moderate cases as the initial treatment.
For patients with multiple recurrent cases of C. diff infection, fecal transplantation can be recommended. Surgery may be recommended for patients who develop complications such as colonic perforation or deterioration of condition despite treatment. Other supportive measures include adequate fluid and electrolyte replacement and reviewing the use of medications.

9. Complications
Some complications that may occur in C. diff infections include fulminant colitis, toxic megacolon, and colon perforation. Fulminant colitis is rare and occurs in 3% of patients. Patients who develop fulminant colitis will require surgery. A study reported a 34.7% death rate among those with fulminant colitis. These patients often require admission into the intensive care unit or require a colectomy (removal of the colon via surgery).
Risk factors for death from fulminant colitis are 70 years of age or more, cardiorespiratory failure, and severe leukopenia or leukocytosis. Toxic megacolon is a complication that occurs when there is acute inflammation and dilation of the colon. The dilation can usually be seen on a plain abdominal X-ray. Patients with colon perforation usually experience tenderness and pain in the abdomen, rigid abdomen, and more. Suspicion of perforation should lead to a prompt surgical consult.

10. Prognosis
There are some individuals with mild disease that can recover without advance therapy. However, they may experience persistent diarrhea that can significantly affect their quality of life. This is the only reason why treatment is recommended for even mild cases of C. diff. Proper antibiotic prescription has been shown to improve symptoms in more than 95% of mild to moderate cases in as little as 3 to 4 days with resolution in 7 to 10 days.
About 20% to 27% relapse after completing therapy (3 days to 3 weeks). Once there is a relapse, there is a higher risk for more relapse. Individuals with two or more relapses have a relapse rate of 65%. Severe strains of C. diff have been reported to be in United States and several European countries.