What Is C. diff?
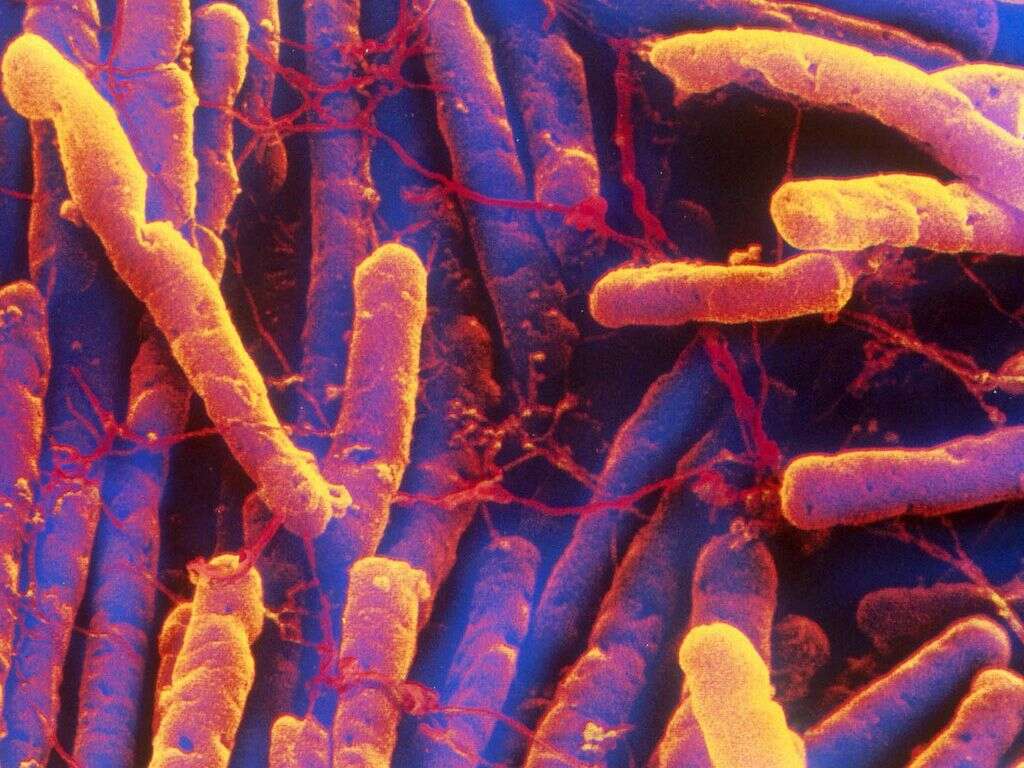
C. diff (Clostridium difficile) is a Gram-positive bacterium that forms spores. It is an anaerobic (does not require oxygen) bacteria that is motile and commonly found anywhere, particularly in soil. The cells that are vegetative are rod-shaped, have the ability to alter their shape to adapt to the environment (pleomorphic), and usually occur in short chains or pairs. When viewed under a microscope, this organism appears to have a drumstick shape cell where there is a bulge at the ends (to form spores).
C. diff shows optimal growth in blood agar in the absence of oxygen at human body temperatures. It produces cytotoxin B and enterotoxin A, resulting in disruption of signal transduction in the host. When in hostile conditions, C. diff produces spores that are able to tolerate conditions that the active bacteria are not able to. It can become established in the colon and can be found in 2% to 5% of the adult population.
1. Pathogenicity
C. diff can produce enterotoxin A and cytotoxin B, which can cause inflammation and diarrhea in individuals who are affected. The diarrhea in patients can be loss of fluid from the intestines or it can also become life-threatening pseudomembranous colitis where there are formation of pseudomembranes and intense inflammation of the colon. There is also an adhesin factor that increases the binding to the colonic cells. Paracresol produced by the bacterium also inhibits other microbial growth to prevent competition for resources. Treatment of C. diff can be difficult due to the physiological abilities of the bacterium (such as protection from pseudomembrane and formation of spores) and increasing antibiotic resistance.
2. Transmission
C. diff can be transmitted from person to person via the fecal-oral route. This means that the disease can be transmitted as the pathogens in the feces pass to another person due to lack of sanitation and poor hygiene practices (such as hand washing). Any surface that becomes contaminated with feces becomes a potential reservoir for C. diff spores. This organism can live on surfaces for long durations.
The spores are heat resistant and cannot be killed by routine surface cleaning or hand sanitizers that are alcohol based. When ingested, the spores are also resistant to stomach acid allowing them to pass into the human system unscathed to multiply in the colon. The World Health Organization (WHO) recommends using soap and alcohol solutions to help limit the spread of spores.
3. Range of Hosts
C. diff is an organism that can affect not only humans but also calves and pigs. This bacterium can inhabit in feces of domestic animals, humans, and can be found in retail meat, sewage, human intestinal tract, and in soil. Based on a study by the Center of Disease Control (CDC) in 2015, it is estimated that in 2011, C. diff affected about 500,000 Americans, which resulted in 29,000 deaths.
This study also found that 40% of cases originated from community healthcare settings such as nursing homes while an additional 24% began in hospitals. C. diff can be commonly be found in the human digestive system but is often outcompeted by other bacteria. When an antibiotic is used, it disrupts the balance of bacteria in the gut and allows the proliferation of C. diff.
4. Risk Factors
Although C. diff infection can occur in any individual regardless of gender or age, most patients who are affected are those who live in long-term care facilities and hospitals. Not only that, they also tend to have received antibiotics. Almost any antibiotic increases the possibility of the colonization of C. diff. However, the most common offenders are the medications that alter the balance of gastrointestinal bacteria.
These include broad spectrum penicillins, fluoroquinolones, clindamycin, and cephalosporins. C. diff infections are also more likely among populations who have a serious illness or are above 65 years of age. Powerful anti-ulcer medications such as proton-pump inhibitors can also increase the risk as it decreases the stomach acidity thereby reducing the ability to fight off the pathogen.
5. Signs and Symptoms
In a C. diff infection, patients can experience symptoms ranging from a mild case of diarrhea to severe life-threatening inflammation in the colon. Diarrhea can be defined as having 3 or more loose stools per 24 hours. A clinical prediction rule used in adults for suspecting a C. diff infection is to establish if there is recent antibiotic use, significant diarrhea, fever, abdominal pain, and a distinctive odor to the stool that has been said to resemble horse manure.
In the pediatric population, the most common symptom is watery diarrhea, appetite loss, fever, abdominal pain, and nausea. In severe cases, the inflammation of the colon can result in having no bowel movements. Some patients may exhibit symptoms of shock (low blood pressure, tachycardia) and dehydration.
6. Diagnosis
The first line diagnostic approach is to perform stool testing for the C. diff toxins (toxin A and toxin B). However, this test is not 100% accurate. Toxigenic culture is a test where the organism is cultured on a media to test for the production of toxins. Although the gold standard, it is a labor-intensive and time-consuming test. An enzyme-linked immunosorbent assay (ELISA) test for toxin A and B can also be performed.
Other tests include a polymerase chain reaction and glutamate dehydrogenase test (in combination with the enzyme immunoassay test). Testing can become difficult if the stools are not watery or loose. An examination of the colon (colonoscopy or flexible sigmoidoscopy) can also be performed. Imaging such as a computed tomography (CT) scan and abdominal x-ray can also be beneficial.
7. Treatment and Management
Patients who are already on antibiotics should stop taking their medication once possible. Treatment generally involves the use of antibiotics that are specific for C. diff so it stops it from growing. Examples of antibiotics that may be prescribed are fidaxomicin and vancomycin. Patients with complications such as toxic megacolon or organ failure may require surgery to remove the diseased part.
Patients should be monitored for relapse especially if they are above 65 years old, have underlying medical issues, or are currently taking another type of antibiotic for a different infection. Other treatment options include fecal microbiota transplant to help restore healthy intestinal bacteria through the placement of another individual’s stool via a colonoscope and supplementation of probiotics.
8. Complications of C. Diff Infections
In C. diff infections, some of the complications that may occur include renal failure, dehydration (die to diarrhea), shock (due to severe dehydration), bowel perforation (because of severe damage to the intestinal lining), peritonitis (from bowel perforation), toxic megacolon (where the individual is unable to expel stool and gas causing it to distend and increase the possibility of rupture), and death (due to various complications).
It is also estimated that about 20% of patients experience recurrent infection. There is also the issue of resistance to antibiotics. Healthcare providers should avoid prescribing antibiotics and, when necessary, choose the simplest and most narrowly focused drug. Patients can also contribute by not demanding to have an antibiotic prescription for every possible infection.
9. Fighting Relapse
Most patients experience improvement of symptoms within 10 to 14 days of treatment with vancomycin or fidaxomicin. However, about 20% of patients experience a relapse after finishing their treatment. Vancomycin and fidaxomicin helps to kill the active form of C. diff, which stops the production of toxins and resolves diarrhea. However, the spores of C. diff survive and resume toxin production once the therapy stops.
Patients who remain well after treatment do not require further investigations. Patients who experience further diarrhea will require testing. When a relapse occurs, another 10 to 14 days of further treatment is recommended. When relapse occurs the second time, vancomycin is recommended. When three or more relapses occur, transplantation of fecal microbiota may be performed.
10. Prevention
C. diff can be prevented by stopping the spread from healthcare facilities such as nursing homes and hospitals. Strict infection control guidelines should be followed. This includes avoiding the unnecessary use of antibiotics. Since most illnesses are caused by viruses, it is best to observe before taking antibiotics. Those who must take antibiotics should be given one that has a narrow range so it does not interfere as much with the balance of bacteria in the gut.
Handwashing is the cornerstone of prevention. Good hand hygiene before and after providing patient care is crucial. Soap and warm water is required during a C. diff outbreak as alcohol-based hand sanitizers do not destroy C. diff spores. Patients who have a C. diff infection should have their own room or share a room with another patient who also has the infection. Disposable gloves and gowns should be worn when caring for these patients. All surfaces should be disinfected using bleach.











