What Is Urticaria?
Urticaria, or hives, are bumps that appear and disappear on the skin, and they are often red or skin-colored. While many people mistake hives for bug bites, these vanish too quickly. Also, this condition is more rash-like.
Many people feel shame or embarrassment from the appearance of urticaria, but nearly 20% of people will experience hives in their lives. Therefore, it is a common condition, and you would have no reason to be embarrassed if your skin breaks out in such a rash.
To better help you and other sufferers understand the condition, it is necessary to talk about the specifics of the disorder. Here are 10 of the most frequently asked questions about urticaria.

1. What Causes Urticaria?
The causes of urticaria are vast and not always readily apparent. While some forms of hives can appear because of a bacterial infection, the common cause is an allergic reaction to a trigger substance. Unfortunately, the triggers are different and specific to each patient. Therefore, it is necessary for you to see an allergist if you believe you are experiencing urticaria symptoms. Also, you might want to consider any substances, foods or objects you have been in contact with or ingested. There are many common triggers for this condition: medication, insect stings or bites, some foods, latex, bacterial infections, viral infections, pollen, pet dander, plants, blood transfusions or physical stimuli.
Unfortunately, the best way to weed out your trigger and the cause of your hives is through the process of elimination. It can be a time-consuming process, but an allergist can help speed up the process.

2. What Are Common Symptoms?
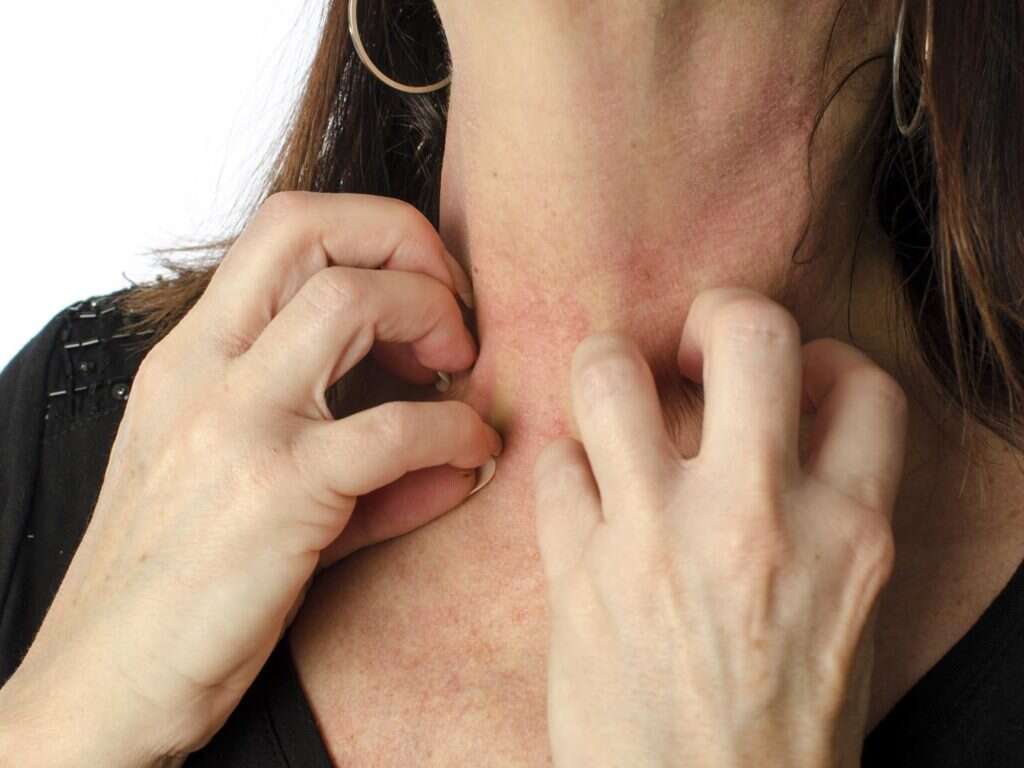
The symptoms of urticaria can either be acute or chronic, meaning hives may last minutes, months or years. They can appear anywhere on your body and are not reserved to recurrence in the same area. It is common for patients with hives to experience itchiness.
Beyond the standard appearance of a rash and raised skin, urticaria can lead to swelling. While not common, the swelling can affect the throat, leading to restricted airways and breathing. However, most of the common symptoms of hives are non-life-threatening. Although, if you have hives that last for over a month, you should see an allergist who can perform a thorough physical to ensure that your urticaria diagnosis is correct.

3. What Do Hives Look Like?
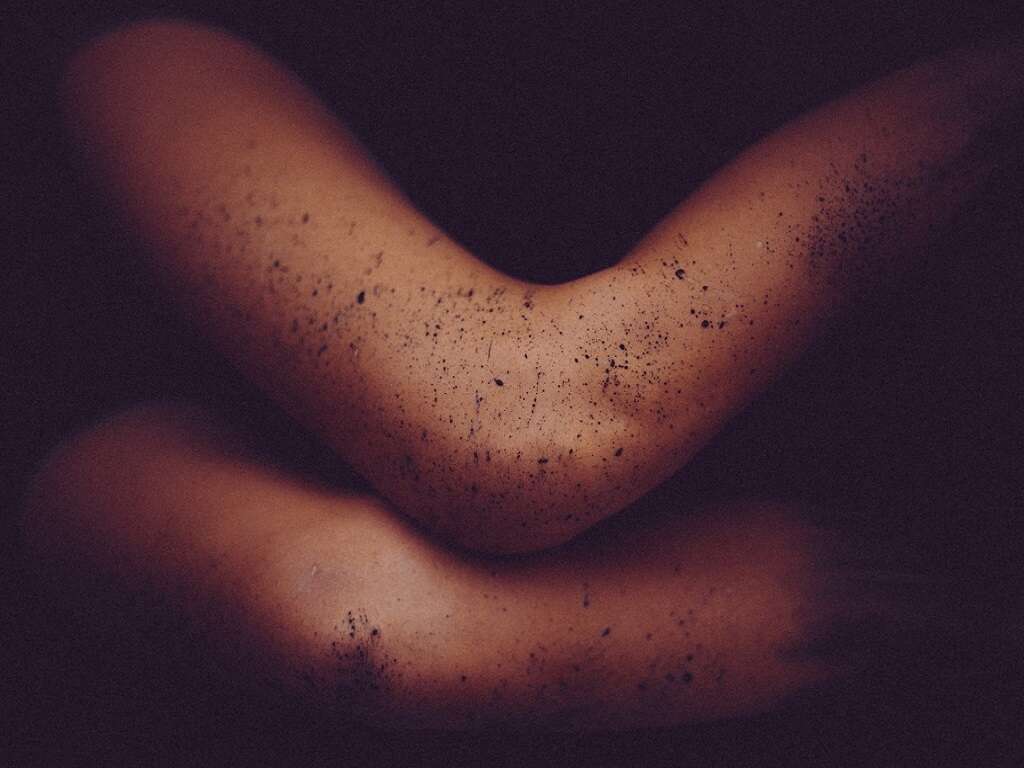
Hives appear as swollen bumps on the skin with surrounding skin appearing red. When pressed, the center of the hive turns white in a process known as blanching. The bumps or plaques show up suddenly and are usually caused by external stimuli or triggers. The body reacts to these stimuli by producing histamine, and in response to this chemical, blood plasma is released, forming hives.
In addition to their appearance, hives cause itching, burning or stinging. It is not uncommon for several small patches of urticaria to spread and connect into larger sections of hives with persistent scratching. Therefore, it is best to avoid itching and scratching. Instead, work with an allergist to determine known triggers, so you can avoid them in the future, reducing the risk of another outbreak.

4. How Is Urticaria Diagnosed?
Diagnosing hives is not too challenging. The appearance of urticaria is discernible from other conditions. However, discovering the trigger is often tricky. While there are cases when the trigger is apparent—a patient eats peanuts and breaks—there are other instances when testing is needed.
While a single episode of hives may not call for testing, recurrent episodes or a single event that has lasted a long time often requires some detective work. An allergist is often your best bet for identifying the underlying triggers. They will use a series of skin tests, blood tests, skin prick tests and oral challenges to determine the cause of your hives. Although, you should prepare yourself for a less than a definitive diagnosis. Sometimes, despite rigorous testing, no trigger is identified.

5. Are There Any Treatments for Urticaria?
If an allergist cannot determine the cause of urticaria, then they may suggest medications to counteract the symptoms. For example, antihistamines are often prescribed or recommended. These medications work by blocking the effect of histamine in the skin, which can reduce the appearance of hives.
Also, for more severe episodes, other more potent medicines can be prescribed. Corticosteroids or immune system modulators, such as prednisone, might help reduce symptoms. These medications work by adjusting the immune system response in your body, hopefully eliminating your hives or reducing inflammation.
For patients with severe urticaria reactions, like swollen lips, tongue or throat, an allergist may prescribe an epinephrine auto-injector. Injectors are typically reserved for cases where anaphylaxis, a potentially fatal allergic reaction, is a concern.

6. How Long Will Urticaria Last?
When patients are given a diagnosis of urticaria, one of the first things they want to know is when the rash will disappear. Unfortunately, the answer varies. For some patients, hives only last a few days or a few weeks. Other people may suffer outbreaks for months or even years. The primary determiner of the timeline is the specific form of urticaria and whether a trigger can be identified.
If you and your allergist have figured out the cause of your symptoms, then avoiding those triggers should eliminate the body’s reaction. However, if you experience chronic hives or chronic idiopathic urticaria, then your symptoms will need to be managed with medications. Also, further testing may indicate another underlying condition, such as thyroid disease, which may be making hives worse.

7. Are Hives Contagious?
In rare circumstances, hives can be contagious, but this is only when the cause is a viral infection, which is why a doctor’s visit is always recommended when you experience sustained urticaria. Otherwise, hives are almost always an allergic or physiological reaction to some external stimuli. For example, some urticaria patients break out in hives because of certain foods or medications, but others have a skin reaction when they are exerting themselves and sweating.
The causes of urticaria vary a great deal, but most are not contagious. However, due to the minor risk of infection or virus, it is beneficial to see a physician so they can perform a skin test and blood test to determine if such factors are a concern.

8. Are Hives Related to Seasonal Allergies?
While hives are typically an allergic reaction to some external substance, seasonal allergies do not often make the condition worse. Only in rare instances have pollen allergies or other seasonal factors been identified as the triggers. You need to remember that for chronic urticaria sufferers, the condition is year-round, which means it is multi-seasonal.
Therefore, seasonal shifts or changes cannot be the main trigger or influence. Instead, urticaria is an immune system response to some outside factor that is present throughout the year, which is why it is often related to food or medication. The best way to determine your trigger is to speak with an allergist who can perform multiple tests to try and identify your triggers.

9. Are Hives Also Known as Angioedema?
Urticaria is not angioedema, but it can be related. While hives are on the skin’s surface, angioedema is swelling of tissue beneath the skin. However, this condition can still be caused by medications or an allergic reaction. Also, it is possible that an enzyme deficiency, which can have a hereditary component, is the cause of angioedema.
While the appearance and symptoms of angioedema are similar to urticaria, there are a few differences that may help identify it. For example, this condition frequently presents with swelling of the eyes, mouth, hands, feet or throat. Also, symptoms are typically accompanied by stomach cramps and difficulty breathing.
Despite the differences in the conditions, angioedema and urticaria are visually incredibly similar. Therefore, it is best to seek out treatment and diagnosis from an allergist, who can also help identify your specific condition.

10. Is There a Cure?
Some people outgrow allergies, but others have those allergies for life. If urticaria is a result of an allergic reaction, then a cure is hard to define. For those who outgrow their allergies, then yes, there is a definitive cure. For those who suffer lifelong allergies, then the only cure is the avoidance of those trigger substances, which may not be possible in every situation.
However, allergies are not the only cause of urticaria. Some forms of the condition are related to a virus or bacterial infection. In these cases, urticaria is likely curable with the appropriate medications and treatment.
Urticaria, also known as hives, is often an allergic reaction, but it can occur because of virus or infection. However, regardless of the cause, hives are a treatable and manageable condition. While not all forms of the condition have a definitive cure, the symptoms can be curbed, making living with the urticaria bearable. Although, for the best possible outcome, you should seek the advice of an allergist or physician. They will be able to perform the necessary tests to help identify your specific triggers, or at the very least, come up with a treatment plan to help relieve your unique symptoms.