What Is Claudication?
Dull, aching pain and discomfort in your legs during physical activity may be claudication. The name comes from the Latin “claudicare,” which means limping. Pain from claudication may cause you to limp, but not all limping is due to claudication.
Claudication is not actually a disease but a symptom. It results from oxygen deficiency in your muscles due to decreased blood flow. Treatment of the underlying condition that causes the blood flow to decrease should also improve symptoms of claudication.

1. What Causes Claudication?
Claudication is most often a symptom of peripheral artery disease, particularly atherosclerosis. Materials found in your blood, such as calcium, cholesterol, and fat, build up in your arteries over time. The buildup is known as plaque, which can cause the arteries to become hard. As the plaque builds up, it reduces the amount of space inside the vessel for blood to flow.
When the muscles are at rest, they may get enough oxygen to meet their needs even with reduced blood flow. However, the muscles’ oxygen demands increase during physical activity when they are in use. When muscles do not get enough oxygen, the pain that results is claudication.

2. What Does Claudication Feel Like?
Most people experience claudication in their legs. Occasionally, it may also occur in the arms. This is less common and usually affects athletes who perform repetitive motions of their arms or people who perform heavy physical labor for a job or a hobby.
If claudication affects both legs, one tends to exhibit worse symptoms than the other. It usually affects only one leg at a time. Claudication is often described as a dull ache in the limbs. It can also involve weakness or fatigue of the muscles. Some people report numbness or heaviness.

3. How Does Claudication Progress?
At first, claudication occurs only during exercise or physical activity and usually occurs after a specific period of time, often in a predictable pattern. For example, if you take walks regularly, you may notice that the pain starts after you travel two blocks. The pain usually gets better if you stop the activity. For this reason, claudication is often described as intermittent.
Over time, as the plaque buildup in your arteries gets worse, the blood flow can decrease even further. As a result, the muscles in the affected limb may not get enough oxygen at baseline, and the pain of claudication may persist even at rest.

4. Who Is Most at Risk?
Claudication affects people over the age of 50 more often than any other age group. Males experience it more often than females. Medical conditions that have a negative effect on circulation, such as diabetes, can increase your risk.
Smoking tobacco also affects your circulation and increases your likelihood of developing claudication. Because claudication is most often a symptom of peripheral artery disease, the risk factors for PAD are also risk factors for claudication. These include obesity, high cholesterol, and high blood pressure.

5. What Are Possible Complications?
Peripheral artery disease, the most common cause of claudication, can cause complications. Decreased circulation can cause coldness and decreased sensation of the affected limbs. Skin that does not receive sufficient blood flow can develop nonhealing sores or serious infections, such as gangrene. Men with PAD can become impotent.
Bear in mind that the buildup in plaque that can damage the peripheral arteries can also affect those supplying blood to the vital organs of the heart and brain. Therefore, arterial disease can also increase your risk of heart attack or stroke. Claudication may be an early sign that you may someday experience cardiovascular events of this nature, so you should take it seriously.

6. What Is Involved in Diagnosis?
Since claudication can be a symptom of a serious underlying medical condition, it is important to discuss it with your doctor. Be prepared to answer questions during physical examination about what activities make your pain worse and what factors make it better.
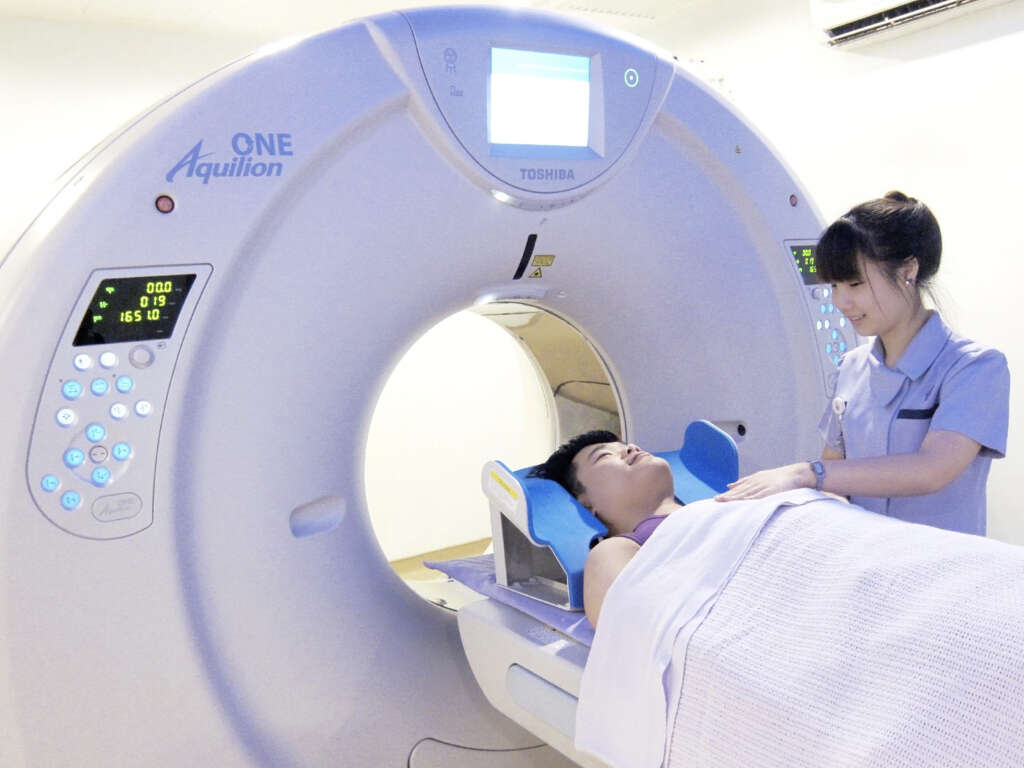
There are a number of tests available to diagnose the underlying cause of claudication. Some are relatively simple, such as gauging your blood flow by checking your blood pressure and pulse at multiple points on your body. Imaging studies, such as MRI or Doppler ultrasound, allow the doctor to visualize the blood flow. Lab tests can measure the levels of harmful materials circulating in the blood.

7. What Medical Treatments Are Available?
Short-term treatment goals for claudication involve reducing the pain. In the long-term, the goal is to manage the underlying condition. Your doctor may prescribe medications to decrease blood pressure, lower cholesterol, or prevent blood clots. A drug called cilostazol can help improve your blood flow and thus relieve your pain.
If other treatments are effective, surgery may not be necessary. However, in the absence of improvement otherwise, your doctor may perform a bypass procedure, which involves grafting a healthy vessel around a diseased one so that the blood can flow more easily. Another surgical option is opening the blocked artery with angioplasty.

8. How Does Exercise Help Improve Claudication?
Claudication can contribute to a vicious cycle. If you experience pain when you exercise, you may decrease physical activity to relieve your discomfort. Less physical activity may worsen the conditions that are causing your claudication, which can become worse as a result.
Exercise has many benefits for dealing with claudication. It helps to improve vascular health and reduce the factors that cause the pain. Doctors typically recommend regular, moderate exercise that incorporates frequent breaks for rest and recovery when pain is present.

9. What Else Can You Do to Prevent Claudication?
Because claudication is a symptom of an underlying medical condition, managing these risk factors may help you avoid claudication. Therefore, you should try to maintain a healthy weight and manage your cholesterol by eating low-fat dairy products, fruits, vegetables, whole grains, and unsaturated fats. You shouldn’t start smoking, and if you already smoke, you should quit.
Compression stockings help to improve the flow of blood in your legs. A clinical study in 2015 proved them helpful for relieving claudication at rest and increasing the amount of time patients could walk without pain when worn over 16 weeks for two hours a day.

10. What Are Strategies for Coping?
There are good ways and bad ways to cope with claudication. You may think that such discomfort just a normal sign of aging, but chances are that it is not. You should discuss the symptoms with your doctor and, in the meantime, don’t abandon activities completely.
A diagnosis of claudication due to peripheral artery disease can affect you mentally and emotionally. You may be able to find a support group in which you can talk to people who are going through the same thing. Protect yourself from misinformation by seeking out as much data as you can from your doctor and other reliable sources.