What Is Antiphospholipid Syndrome?
Our blood vessels transport blood all around our bodies and they carry essential nutrients and oxygen. Our heart is constantly beating, and it needs to be because our cells need constant nourishment and energy. If the flow was to stop then all or part of our body could be in a lot of trouble.
One thing that can cause the blood flow through any vessel to be interrupted is a blood clot. There are numerous reasons why these clots might form, and one of these is a medical condition known as antiphospholipid syndrome.
1. Blood Coagulation
In order to maintain the integrity of the body’s blood vessels, any damage to their wall must be immediately repaired. This process is known as hemostasis, which involves the formation of blood clots (thrombus) at the site of the injury. First, a weak platelet plug forms due to the interaction between platelets and the wall of the vessel. Secondly, since this plug needs to be stabilized, coagulation cascades are activated. These cascades are merely pathways mediated by different clotting factors, that lead to the generation of a substance known as thrombin, which converts the fibrinogen present in the platelet plug to fibrin. Fibrin (once cross-linked) is the key to the formation of a stable thrombus.
Note that hemostasis is a complex process that is necessary to ensure that our tissues receive oxygenated blood. Thus, it is a highly regulated process. When the mechanisms that regulate blood coagulation are altered, a condition (among many others) known as antiphospholipid syndrome can occur.

2. Antiphospholipid Syndrome
Antiphospholipid syndrome is an autoimmune condition that can be acquired during a person’s lifetime. This means that your immune system attacks its own healthy tissue by mistake, as a result of a mix of genetic, hormonal, and environmental factors. It does this by producing auto-antibodies, known as antiphospholipid antibodies, that target protein that attaches to fat molecules on the outer layer of cells. By poorly understood mechanisms, this causes a dysregulation of blood coagulation that makes the formation of blood clots (thrombosis) much more likely to occur.
These alterations can lead to dangerous clotting in arteries and veins, which can result in the formation of blood clots in the arms, legs, lungs, brain, or kidneys. Antiphospholipid syndrome, when present in pregnant women, can cause miscarriage and stillbirth.

3. Risk Factors
Antiphospholipid syndrome is a disease of unknown cause. However, possible triggers and risk factors have been suggested. Many of the risk factors that have been proposed are associated with the clinical syndrome itself and/or the presence of antiphospholipid antibodies.
Possible risk factors for antiphospholipid syndrome include infections, medications, family history, and immune system disorders. Infections associated with the antiphospholipid syndrome include hepatitis C, syphilis, HIV/AIDS, and malaria. Moreover, drugs that have been associated with this condition include certain medications for the cardiovascular system (i.e. hydralazine, procainamide, quinidine, propranolol), psychiatric drugs (i.e. phenytoin, chlorpromazine), among others. Finally, genetic predisposition may also play an important role, since a strong association has been established between the presence of abnormal antibodies and the presence of specific genes (HLA genes DRw53, DR7, and DR4). Also, this condition can run in families, seen as relatives of a person with the disease are more likely to have antiphospholipid antibodies.
Note that it’s possible for a person to have antiphospholipid antibodies in their body without developing signs or symptoms of the disease. However, these people are at a higher risk of developing thrombosis, especially if they become pregnant, are tobacco smokers, take oral contraceptives or estrogen therapy, have high levels of cholesterol and triglycerides, or remain immobile for long periods of time.

4. Associated conditions
Some people with antiphospholipid syndrome have no evidence of associated conditions, while others can present with associated autoimmune or rheumatic diseases. The most frequent associated disease is systemic lupus erythematosus (commonly known as lupus or SLE).
Other conditions that can be associated with the antiphospholipid syndrome include Sjögren syndrome, rheumatoid arthritis, autoimmune thrombocytopenic purpura, and systemic sclerosis. Furthermore, some studies suggest that having any of these conditions can also be a risk factor for developing the antiphospholipid syndrome.
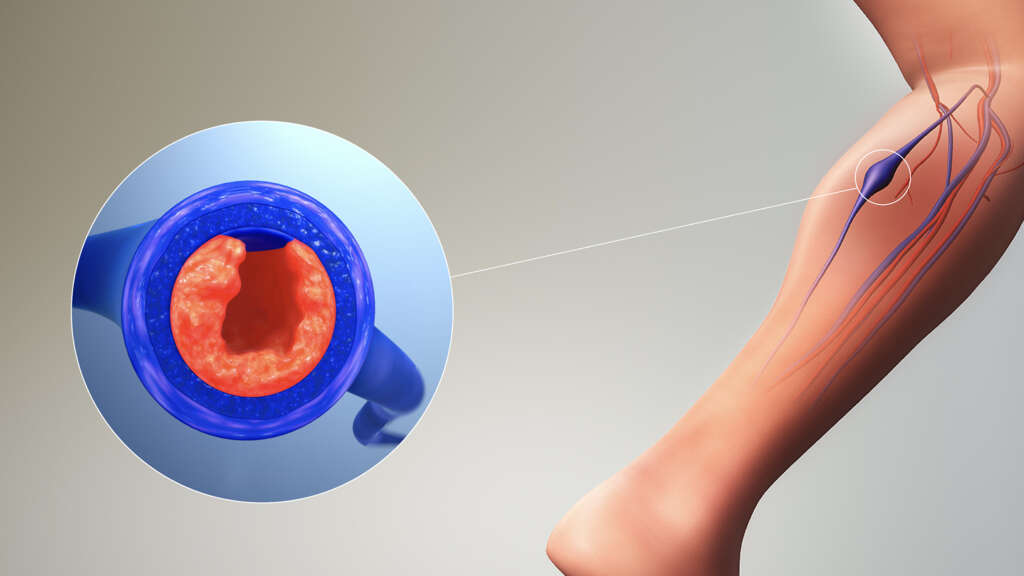
5. Deep Vein Thrombosis
As you may already know, thrombosis is the formation of a blood clot or a thrombus, within a blood vessel. A thrombus prevents blood from flowing normally through the circulatory system. As explained above, people with antiphospholipid syndrome have a higher risk of thrombotic events (i.e. DVT).
Deep vein thrombosis (DVT) is simply when a thrombus forms in one or more of the deep veins in your body, usually in the veins located in your legs. Signs and symptoms of deep vein thrombosis are usually localized (on the affected leg) and include pain, swelling, redness, and warmness. Dangerously, these clots can break loose and travel through your bloodstream to your lungs, blocking blood flow (pulmonary embolism). Symptoms of pulmonary embolism include chest pain, sudden shortness of breath (sudden dyspnea), and coughing up blood-streaked mucus.
6. Arterial Thrombosis
Our arteries carry oxygenated blood away from our heart to the rest of the body. Some people can develop a clot in one of their arteries, and this is known as arterial thrombosis.
Arterial thrombosis can lead to serious conditions like a heart attack (coronary arteries), ischemic stroke (cerebral vascular system), transient ischemic attacks (similar to a stroke but last only minutes and cause no permanent damage), digital ulcers (sores in the tips of fingers), and gangrene of extremities.
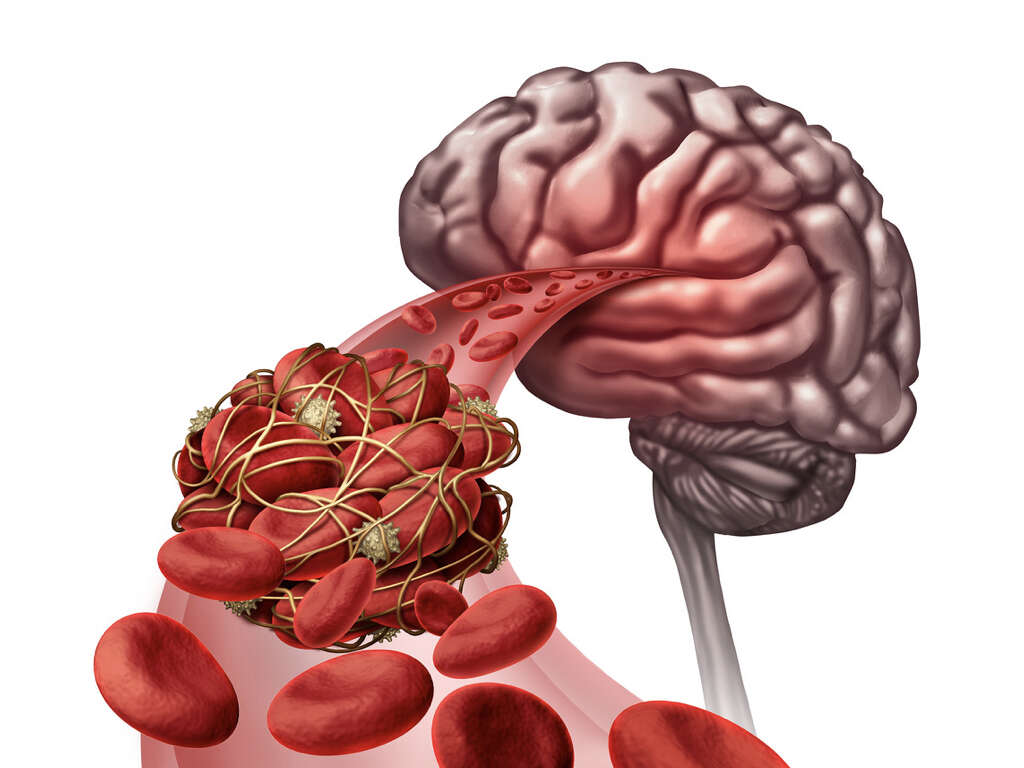
7. Clots in Brain
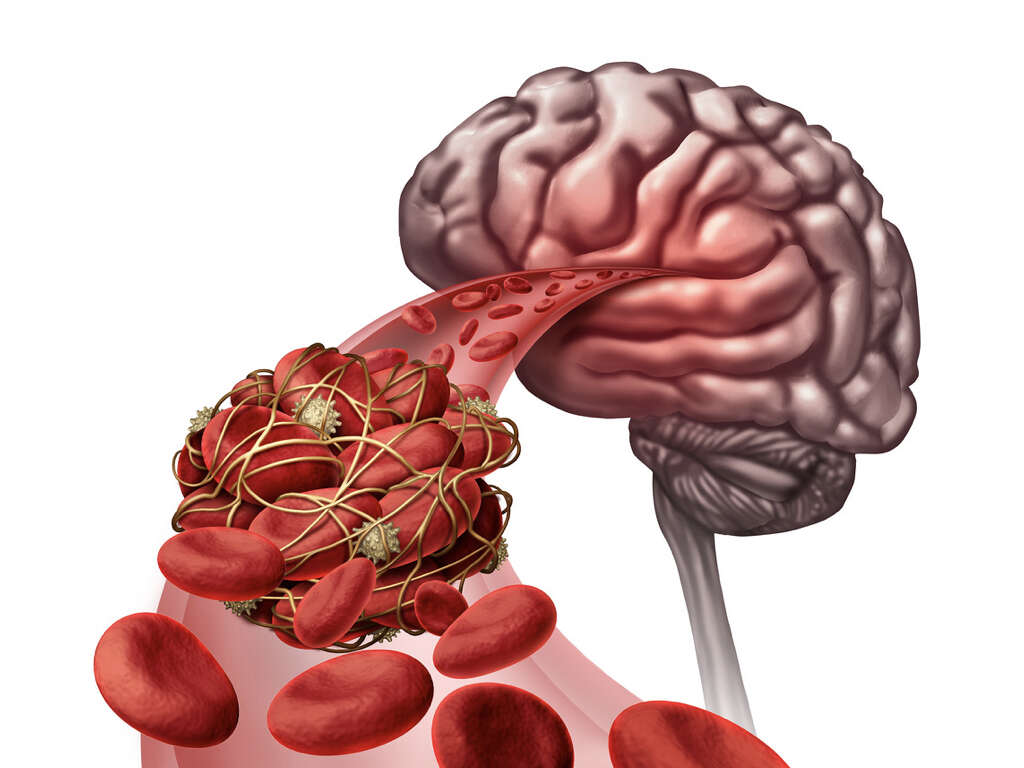
Our brain needs a lot of oxygen to work properly, and its supply has to be constant. If the flow is interrupted, even for a short while, then the patient can be in some serious trouble. Patients with antiphospholipid syndrome are at risk for developing thrombosis in the cerebral vascular system (i.e. stroke, TIA).
If there is a blood clot that interrupts blood flow completely in a major blood vessel of the brain, the tissue that it supplies can suffer permanent damage (acute infarction). This process is known as an ischemic stroke. The signs and symptoms of a stroke include visual disturbances, difficulty speaking or understanding speech, and sudden numbness, weakness, or paralysis of the face, arm, or leg. However, when the interruption of blood flow (ischemia) to the brain is brief and tissue infarction does not occur, it is referred to as a transient ischemic attack (TIA).
Importantly, a stroke can occur in young people with the antiphospholipid syndrome that have no risk factors for cardiovascular disease. When this occurs, it should alert the physician on the possibility of antiphospholipid syndrome.
8. Pregnancy complications
Women with antiphospholipid syndrome are at a high risk of recurrent miscarriages and stillbirths. In fact, of women with recurrent miscarriages, roughly ten to fifteen percent are diagnosed with this condition. In general, almost half of pregnancy losses associated with antiphospholipid syndrome occur in the first trimester.
The antiphospholipid syndrome has also been associated with other pregnancy complications such as preeclampsia (high blood pressure), placental insufficiency, premature delivery, and neonatal complications.

9. Who Is Affected?
Antiphospholipid syndrome can affect people of all ages, from the elderly down to infants. However, it is more likely to be found in women, and it is also more likely to be found in middle-aged adults.
The extent of the symptoms will vary from person to person, and many people with the condition will be able to continue with little to no effect on their quality of life.

10. Treatment and Management
Antiphospholipid syndrome cannot be cured; however, actions can be taken to prevent clinical events (thrombosis). The first step in prevention is the elimination/ treatment of risk factors like oral contraceptives, tobacco use, high blood pressure, and hyperlipidemia (high cholesterol/ triglycerides). Also, when a person with this disease requires surgery or hospitalization, preventive measures in the form of antiplatelet medication can also be used. Patients with other associated diseases (i.e. Systemic lupus erythematosus) might require other medications.
When a person with antiphospholipid syndrome develops a thrombotic episode, standard initial treatment involves a combination of blood-thinning medications (heparin and warfarin). These drugs increase the risk of bleeding episodes; thus, doctors must monitor the dosage closely (with blood tests).