Rectal Prolapse Symptoms, Causes and More
 Article Sources
Article Sources
- 1. ‘Rectal Prolapse Expanded Version.’ ASCRS, fascrs.org/patients/diseases-and-conditions/a-z/rectal-prolapse-expanded-version
- 2. ‘Rectal Prolapse: Treatment, Diagnosis, Causes & Symptoms.’ Cleveland Clinic, my.clevelandclinic.org/health/diseases/14615-rectal-prolapse#:~:text=Is rectal prolapse just another, the anus and lower rectum
- 3. Jan Rakinic, MD. ‘Rectal Prolapse Treatment & Management: Approach Considerations, Nonoperative Management, Surgical Options.’ Medscape, 24 July 2020, emedicine.medscape.com/article/2026460-treatment
- 4. Trompetto, Mario, et al. ‘Altemeier’s Procedure for Complete Rectal Prolapse; Outcome and Function in 43 Consecutive Female Patients.’ BMC Surgery, BioMed Central, 3 Jan. 2019, bmcsurg.biomedcentral.com/articles/10.1186/s12893-018-0463-7#:~:text=Altemeier’s procedure is one of the pouch of Douglas
Rectal prolapse refers to a condition where the rectum pushes out through the anus. The rectum is the terminating point of the colon or large intestine, and the anus is the opening the body uses to evacuate solid waste.
About 2.5 out of 100,000 people may experience rectal prolapse, and women over 50 may be over six times more likely than men to have it. This condition is commonly mistaken for severe hemorrhoids. The degree of rectal prolapse varies from one person to another and from mild to severe. Mild cases don't usually require surgery, which may be necessary for severe cases.

Symptoms
Rectal prolapse symptoms may be slow to appear.1‘Rectal Prolapse Expanded Version.’ ASCRS, fascrs.org/patients/diseases-and-conditions/a-z/rectal-prolapse-expanded-version At first, a person may feel as though their anus is bulging, or they may feel as if they're sitting on a ball. A reddish bulge may peek through or extend out of the anus.
In some cases, a small part of the rectum may emerge during bowel movements and retreat either by itself or when pushed back into place. Activities such as sitting, walking or exercising may also push out the rectum. In severe cases, the rectum's inner lining may bleed. Passing stool, gas or urine may also become difficult.

Types
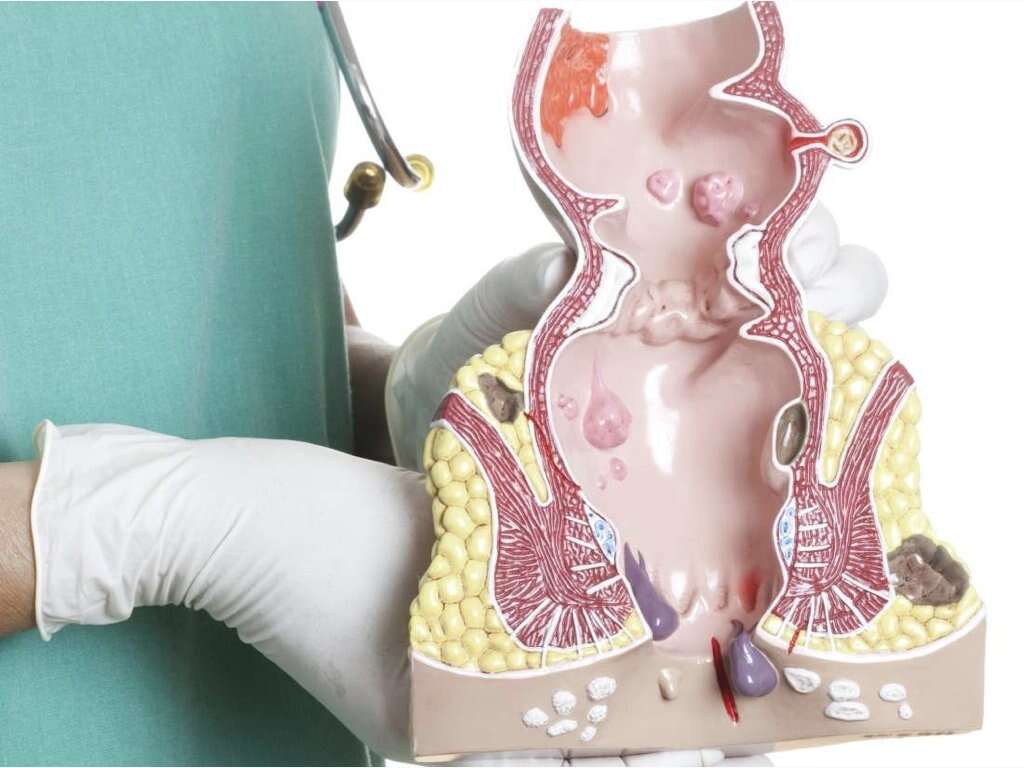
Rectal prolapse may take three forms: internal prolapse, partial prolapse and complete prolapse. The extent of the movement of the rectum is commonly used to identify the type of rectal prolapse a person is experiencing.
With an internal prolapse, the rectum begins to drop but doesn't yet emerge from the anus. In a partial prolapse, a part of the rectum emerges from the anus. In a complete prolapse, the entire rectum extends out of the anus.

Causes
Several medical conditions may cause rectal prolapse. These include nerve damage, a weakened anal sphincter and chronic constipation. Damage to the nerves that control the anal and rectal muscles may lead to rectal prolapse. Nerve damage may occur due to pelvic surgery, a spinal injury or pregnancy.
The anal sphincter muscle allows stool to pass through the rectum. Pregnancy, childbirth and age may weaken it. Chronic constipation may also strain the rectum and push it down, especially when strained bowel movements occur over many years.

Risk Factors
Some conditions may increase the risk of developing rectal prolapse, but they don't directly cause it. These include diabetes, cystic fibrosis and chronic obstructive pulmonary disease. Undergoing a hysterectomy may also increase this risk.
Women over the age of 50 are six times more likely than men to develop rectal prolapse.1‘Rectal Prolapse Expanded Version.’ ASCRS, fascrs.org/patients/diseases-and-conditions/a-z/rectal-prolapse-expanded-version Most women who have this condition are aged 60 years or older. Few men develop rectal prolapse, and the ones who do are typically 40 years of age or younger.

Rectal Prolapse vs. Hemorrhoids
Both hemorrhoids and rectal prolapse may be uncomfortable and excruciating conditions. Initially, rectal prolapse may seem like severe hemorrhoids.2‘Rectal Prolapse: Treatment, Diagnosis, Causes & Symptoms.’ Cleveland Clinic, my.clevelandclinic.org/health/diseases/14615-rectal-prolapse#:~:text=Is rectal prolapse just another, the anus and lower rectum Likewise, hemorrhoids on the anus may seem like a partial rectal prolapse.
Rectal prolapse involves movement of the rectum, whereas hemorrhoids involve the swelling of blood vessels in the anal or rectal walls. Hemorrhoids may itch and become painful despite being the less severe of the two conditions. Red blood on toilet paper may indicate the presence of either hemorrhoids or rectal prolapse.

Diagnosis
Diagnosis begins with a doctor reviewing a person's medical history and asking them to describe their symptoms. The doctor may also undertake a complete physical examination, in which the patient may be asked to squat and strain as if they're passing stool.
The doctor observes the anus and may place a gloved finger inside to assess the strength and health of the anal sphincter and rectum. The patient may also undergo a colonoscopy to determine whether any polyps are present in the large intestine.

Treatment
Very minor cases of rectal prolapse may be treated at home using stool softeners and pushing the prolapsed tissue back into the anus using the hand. However, surgery is necessary in many cases.
The extent of the prolapse, existing health problems, the person's age and the results of a physical exam and tests determine the type of surgery required. The surgeon's experience and preferences may also factor into their choice of surgery type. The most common approaches are abdominal and rectal surgery.

Rectal Repair Approach
Rectal procedures may be used in patients who are older or have existing medical problems. Rather than a general anesthesia, these patients may require epidural or spinal anesthesia.3Jan Rakinic, MD. ‘Rectal Prolapse Treatment & Management: Approach Considerations, Nonoperative Management, Surgical Options.’ Medscape, 24 July 2020, emedicine.medscape.com/article/2026460-treatment The common rectal repair methods are the Delorme and Altemeier procedures.
The Altemeier procedure involves cutting off or amputating the part of the rectum that emerges out of the anus and sewing two ends back together.4Trompetto, Mario, et al. ‘Altemeier’s Procedure for Complete Rectal Prolapse; Outcome and Function in 43 Consecutive Female Patients.’ BMC Surgery, BioMed Central, 3 Jan. 2019, bmcsurg.biomedcentral.com/articles/10.1186/s12893-018-0463-7#:~:text=Altemeier’s procedure is one of the pouch of Douglas In contrast, the Delorme procedure involves removing the fallen rectum's inner lining and folding and stitching the outer layers.

Prognosis
As painful and uncomfortable as it may be, rectal prolapse is treatable. A person who undergoes surgery for rectal prolapse generally has a favorable prognosis. They may be on soft foods and liquids for a period and may need to use a stool softener to prevent strained bowel movements and constipation.
The patient's health and the type of surgery they undergo determine the time they spend in the hospital after surgery. Full recovery may take about six weeks.

Prevention
Prevention of rectal prolapse may not be possible. Maintaining good intestinal health may reduce the risk of developing this condition. Specifically, making lifestyle choices that help prevent constipation may help a person avoid rectal prolapse.
Doctors may advise people to include high-fiber foods in their diets, such as vegetables, fruits, legumes and bran. Health care professionals also encourage people to reduce their intake of processed foods. It's also advisable to drink plenty of water, exercise regularly and reduce stress through relaxation techniques such as meditation.