Pulmonary Embolism Symptoms
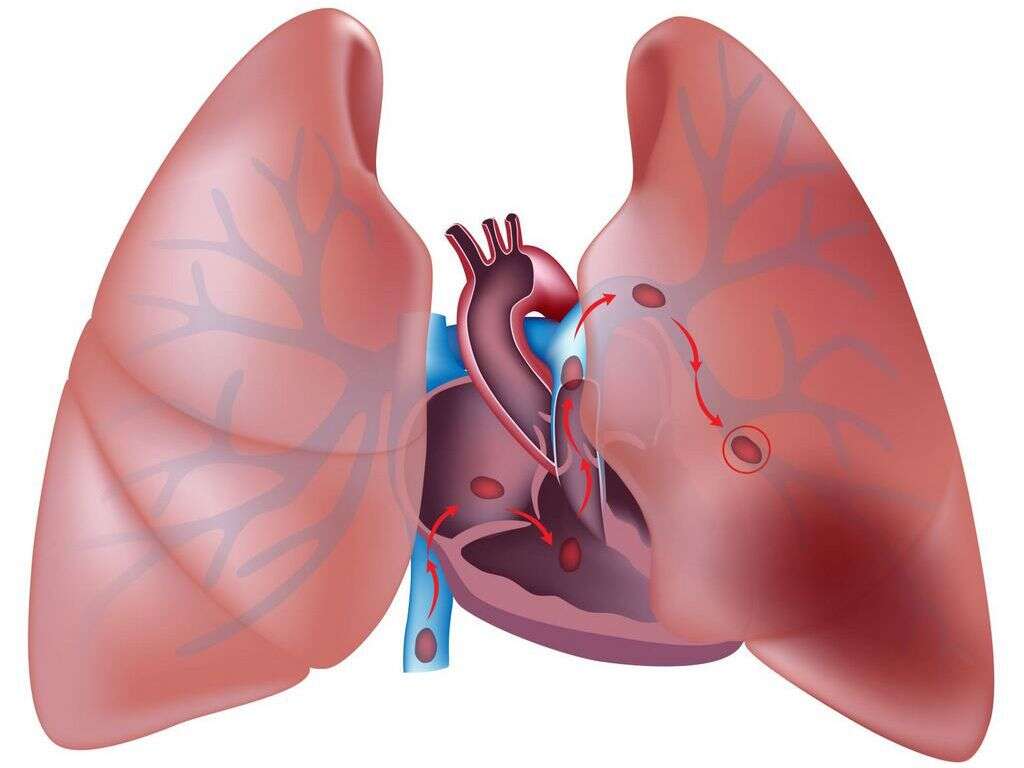
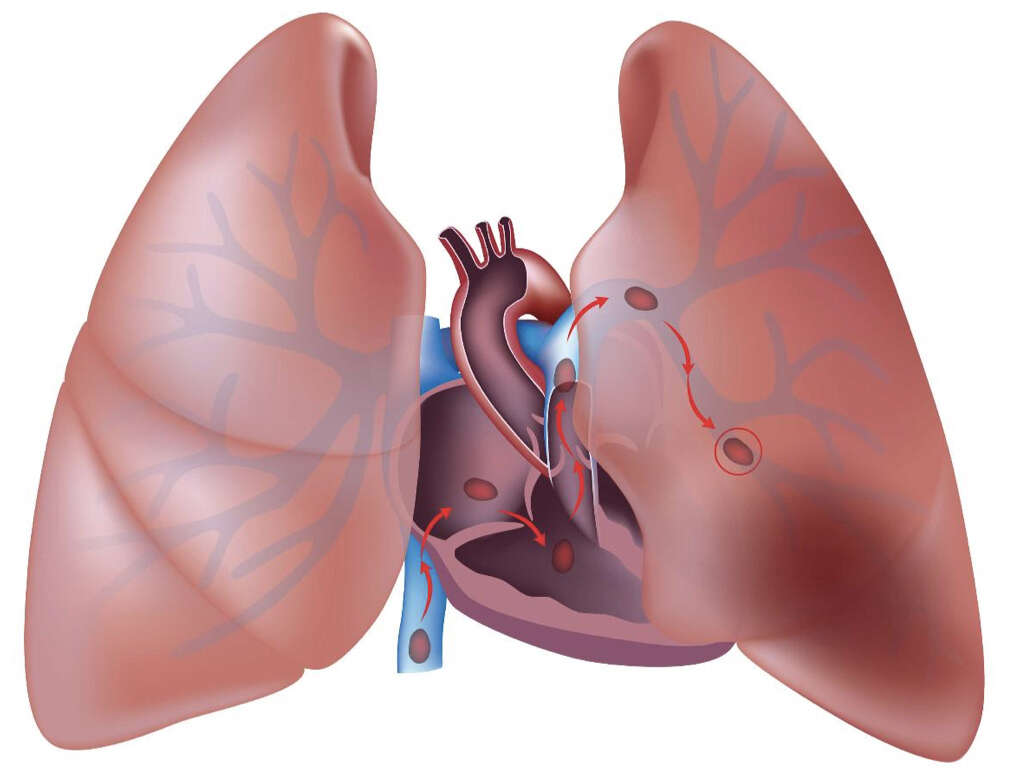
The pulmonary arteries carry deoxygenated blood away from your heart to the lungs. Oxygen exchange takes place in the capillaries, and the now-oxygenated blood flows back to the heart via the pulmonary veins. The heart then pumps the blood to the rest of the body, where the tissues crave the oxygen it carries. A pulmonary embolism interferes with this process by blocking the flow of blood to the lungs through the pulmonary arteries. Not only does this disrupt the flow of blood to the lungs, it also prevents the heart from providing oxygen-rich blood to the other areas of the body that need it.
A pulmonary embolism is an emergency requiring immediate medical attention. Unfortunately, however, it is sometimes difficult to diagnose because many of the symptoms are very similar to those of a heart attack. Doctors at the emergency room must quickly perform tests to diagnose the cause of the symptoms. It is possible to survive a PE, but the chances decrease the longer it takes to get treatment. Therefore, it is important to recognize the symptoms and seek emergency help immediately.

1. DVT Blood Clots
Any substance that could block the flow of blood through the pulmonary arteries, such as air bubbles or tumor fragments, can become an embolism. However, the most common cause of PE is a blood clot that forms in the deep veins of the legs or, more rarely, the arms. The medical term for this condition is deep vein thrombosis. The clot breaks off and travels through the bloodstream to the lungs, where it forms a pulmonary embolism that blocks the flow of blood.
Unfortunately, a DVT sometimes occurs without any symptoms at all. It can form a pulmonary embolism before you even know there is a problem. Other times, however, a DVT causes symptoms in the lower leg where clots usually occur. Due to a partial blockage of the vein, the calf may swell up and become red in the area of the clot. This may be accompanied by a persistent pain that is throbbing and feels like a cramp, or a sensation of tightness in the calf muscle. Symptoms of a DVT should be evaluated as soon as possible. If the clot is successfully treated, a pulmonary embolism may be avoided altogether.

2. Acute Chest Pain
A pulmonary embolism can cause sharp, sustained pain in the chest. This is a symptom that should always receive immediate medical evaluation because it is suspicious for both a heart attack and a PE, each of which could prove fatal if left untreated.
However, there can be a difference between the quality of pain that you experience with a pulmonary embolism compared to a heart attack. The latter tends to cause a sensation of pressure or squeezing, as though an elephant is sitting on your chest. A pulmonary embolism causes sharp pain that can get worse when you change position to stoop or bend over. Sometimes, merely attempting to breathe in deeply makes the pain worse. Coughing, another symptom of PE, can also exacerbate the pain in your chest.

3. Shortness of Breath
Also called dyspnea, shortness of breath due to a pulmonary embolism can occur very suddenly. This is another symptom that a PE has in common with a heart attack and can make it very difficult to differentiate the two without the aid of medical imaging and other diagnostics. Shortness of breath that gets worse with physical activity is called dyspnea on exertion. Though this can also occur with a heart attack, it is always present in cases of pulmonary embolism.
Patients who have chronic lung illnesses may attribute shortness of breath to the pre-existing condition and not recognize it as a sign of a PE. For example, one patient reported initially attributing her acute breathing difficulties to her asthma, which can also cause sudden shortness of breath and dyspnea on exertion. It was ultimately discovered, however, that a pulmonary embolism was to blame.

4. Cough
Distress to the lungs from a pulmonary embolism can cause coughing, a symptom that rarely, if ever, occurs during a heart attack. Often, a cough caused by a PE will be dry. However, the coughing may also produce some mucus, which is called sputum when it results from coughing.
If you have a cough caused by a pulmonary embolism, you may notice that the sputum is tinged pink or red with blood. Your coughing may also produce blood with no sputum. This is known as hemoptysis, and it is a much greater cause for concern than blood-tinged sputum. You may also observe that coughing makes the pain in your chest worse.
5. Excessive Sweating
With a pulmonary embolism, as well as a heart attack and a number of other conditions, both acute and chronic, you may experience excessive sweating. This causes your skin to become clammy and wet to the touch. The scientific term for excessive sweating is hyperhidrosis. Acute secondary hyperhidrosis occurs suddenly due to an underlying medical condition and is the type that you will most likely see with a PE.
When excess sweating is caused by a heart attack, it is often accompanied by a feeling of nausea. Therefore, acute hyperhidrosis that occurs with chest pain and shortness of breath but without nausea is more indicative of a pulmonary embolism than a heart attack; however, nausea can occur with a PE as well.

6. Changes to Heartbeat
Shortness of breath and other symptoms of pulmonary embolism can put stress on the heart. When this happens, the heartbeat can increase to potentially dangerous levels while at rest. The medical term for an increased heart rate is tachycardia. A resting heart rate over 100 beats per minute is the threshold for tachycardia, which can occur due to a pulmonary embolism or a heart attack. Tachycardia also sometimes affects a particular part of the heart. For example, ventricular tachycardia affects the ventricles, which are the two larger, lower chambers. Atrial fibrillation is another type of tachycardia that affects the two smaller, upper chambers of the heart.
In addition to increasing the heart rate, pulmonary embolism can also cause the heartbeat to become irregular. This is known as arrhythmia, and it too can occur due to either a heart attack and a PE. There are many different patterns that arrhythmia can follow. It can be regularly irregular, meaning that your heart skips after a certain number of beats in a predictable pattern. It can also be irregularly irregular, with no discernible pattern for the discrepancy.

7. Dizziness or Light-headedness
When a pulmonary embolism obstructs blood flow to your lungs, it means that your heart cannot pump enough oxygenated blood to the other areas of your body that need it, including the brain. When your brain does not receive enough oxygen, you may start to experience symptoms of light-headedness or dizziness.
A heart attack can also cause symptoms of dizziness and/or light-headedness and for the same reason: lack of oxygen to the brain. However, dizziness and light-headedness due to a pulmonary embolism can cause you to faint, while this rarely happens during a heart attack.

8. Cyanosis
Of course, it is not only the brain that suffers from a lack of oxygen due to a pulmonary embolism. All the other tissues of the body also experience oxygen deprivation. The body has a mechanism that kicks in when it is not getting enough oxygen. It sends the blood flow to the areas that most need it, including the brain and other vital organs. Non-vital areas, such as the extremities, therefore receive even less oxygen.
The lack of oxygen can cause cyanosis, which is a bluish discoloration of the skin. You may notice it particularly in the fingers, especially under the nails, and around the lips.

9. Low Blood Pressure
During a pulmonary embolism, the volume of blood circulating in your body may decrease. This causes low blood pressure, also known as hypo-tension. A potentially life-threatening condition on its own, it is only present in severe PE cases.
With a severe pulmonary embolism, hypo-tension typically occurs alongside right ventricular dysfunction. A doctor may treat hypo-tension due to PE with a mild intravenous saline solution to augment the flow of fluid in the blood vessels. However, he or she must take care not to overload the right ventricle in the process.

10. Fever
Fever, also known as pyrexia, is not a common symptom of pulmonary embolism. In fact, there is some controversy over whether PE causes fever at all or whether it is only present incidentally due to an underlying medical condition.
When fever is present during a pulmonary embolism, it is typically low-grade, meaning that it ranges from between 100 to 101 degrees Fahrenheit. It rarely reaches high-grade levels of 103 degrees to 107 degrees, nor does it reach the intermediate grade of 102 degrees Fahrenheit. A patient exhibiting a high fever during a pulmonary embolism may need assessment for an underlying condition once his or her condition is stable. If the temperature is dangerously high, i.e., between 104 and 107 degrees Fahrenheit, doctors may need to provide symptomatic treatment to lower the temperature before the assessment can take place.