What Is Tularemia?
Tularemia is a disease that can be caught from other animals that are also infected. It cannot be spread from person to person as far as we know. Although rare, the disease is still found all over the world, especially in rural areas. This is because living in rural areas makes people more likely to come into contact with infected animals.
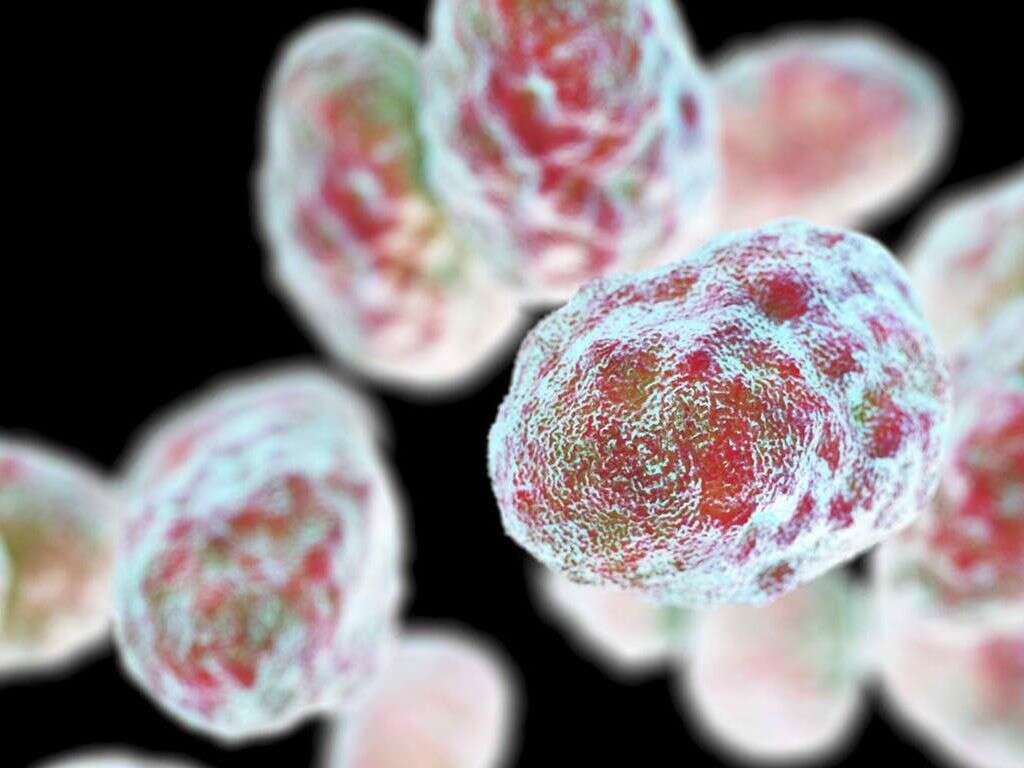
The disease is caused by the Francisella tularensis bacterium, and it is usually treatable. It will be fatal in a small number of cases, however, so treatment should be sought as soon as possible. It can be transmitted in different ways, and there are also different varieties of the disease.
1. Different Types
There are several different types of tularemia, and the most common of them all is ulceroglandular tularemia. This variety is known for causing skin ulcers where the infection took place. Glandular tularemiais similar, but it does not cause ulcers. There is also oropharyngeal tularemia, which will tend to be caught from contaminated meat or water.
Pneumonic tularemia is another variety that is known for causing the same symptoms as pneumonia. Another variety is oculoglandular tularemia, and this will affect the patient’s eyes. Perhaps the most serious type is typhoidal tularemia, but this is thankfully also the rarest variety of the disease.
2. Insect Bites
Tularemia can infect other animals that are prone to having parasites like ticks and flies that will feed off their blood. When a parasite does feed off an infected animal then the parasite will itself become infected. When the parasite feeds off a human, the bacterium responsible for tularemia can then be passed on again.
There are a number of potential ways that tularemia can be transmitted. One of these is by way of insect bites. It is usually tick bites that are responsible for spreading the disease, although it is also sometimes spread by deer flies. Precautions should be taken to avoid being bitten in high risk areas.

3. Contaminated Food
Food safety standards tend to be quite strict in developed countries, and for some very good reasons. If somebody was to eat food that was contaminated with a pathogen then it could cause them to fall ill. Dangerously so in some cases. One potential disease caught by eating contaminated food is tularemia.
When cooking game meat, it is especially important to ensure it is thoroughly cooked at a high enough temperature. This is to make sure that all bacteria and any other pathogens present are killed outright. The disease can also be caught from contaminated water, and boiling water will help protect against disease.

4. Exposure To Infected Animals
If you are unfortunate then you might contract tularemia by being exposed to animals that are infected with the bacteria. Infection can take place by being bitten, while even just handling animals can result in an infection if there are any breaks in your skin. Contracting the bacteria in this way is likely to cause ulceroglandular tularemia.
It is usually when handling rabbits that the disease is caught. In addition, rubbing your eyes after handling an infected animal can result in ocular tularemia. People that are likely to be exposed to infected animals should take precautions to protect themselves from the disease.
5. Airborne Bacteria
The bacteria responsible for tularemia can survive for some time on deceased animals and/or in the soil. If infected soil is disturbed then the bacteria can be flung into the air, and it can then be inhaled. Once inhaled, the bacteria can then infect the lungs and go on to cause pneumonic tularemia.
Those at high risk from this variety of the disease include people that are involved in construction, landscape gardening, and other vocations will expose them to the bacteria. People that work in laboratories will also need to take precautions to help prevent them from inhaling the bacterium.

6. Symptoms
The symptoms of tularemia will vary according to which type of the disease has been contracted. It can take as long as two weeks for symptoms to show, but it will usually happen within three to five days. One potential symptom is ulcers on the skin where the infection took place.
Other potential symptoms include a fever, chills, headache, and lymph glands that are painful and swollen. Some people can also experience breathing difficulties, chest pain, and exhaustion. Eye pain and redness are other potential symptoms, along with a sensitivity to light and discharge from the eyes. Pneumonia is another potential symptom, as is an enlarged spleen and/or liver.

7. Complications
Some patients with tularemia will go on to develop pericarditis. This is the inflammation of a membrane that helps to protect the heart. This condition can affect the heart’s ability to pump. The bacteria can also spread to the bones, sometimes causing a bone infection, which is known as osteomyelitis.
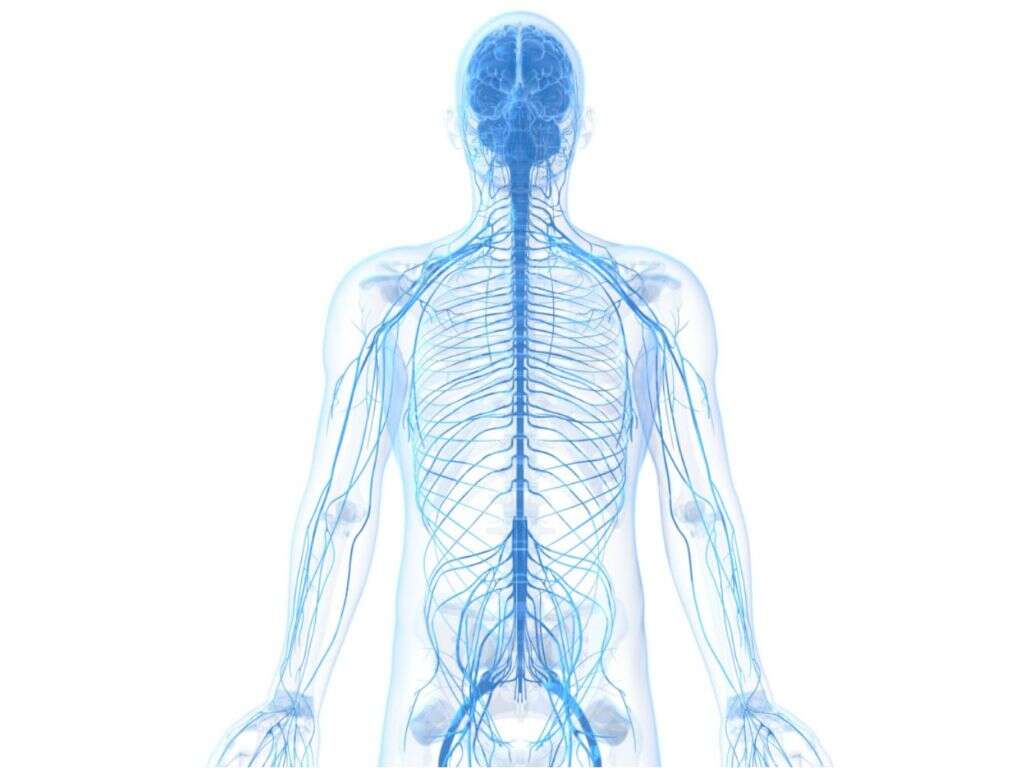
Pneumonic tularemia can result in respiratory failure, meaning the patient will not be able to take on oxygen or remove carbon dioxide from their body. If the bacterium spreads to the membrane protecting the spinal cord and brain, it can result in meningitis, which can be fatal in the more severe cases.

8. Prevention
There is no vaccine for the condition yet. However, people can take precautions that will help to decrease the likelihood that they will catch the disease. This includes handling wild animals with care, and avoid consuming animals that appear underweight or ill in some other way. Also, make sure to keep any pets safe from insects like ticks.
Wearing a mask while gardening can help to protect you against inhaling the bacterium. Wearing long clothing will help protect you from insect bites, and insect repellents can also help prevent bites. If you have been in a tick infested area, then you should check your body for ticks as soon as you can.

9. Diagnosis
Depending on the variety of tularemia you have, the symptoms of the disease are likely to be similar to other common diseases. This means the condition will often go undiagnosed. If tularemia is suspected, then your doctor is likely to want to request some tests to confirm the diagnosis.
With sputum and/or blood samples, experts are able to try and culture any bacteria that might be present. Blood tests can also help experts look for the corresponding antibodies, but this is unlikely to be accurate shortly after the initial infection. Imaging techniques may also be used to help look for signs of pneumonia.

10. Treatment
Treatment for tularemia will typically involve antibiotics. The exact type of antibiotic that is used will depend on which type of tularemia the patient has. The antibiotics may be taken orally, although they are also sometimes injected. The patient may also need treatment for any complications they may have.
In cases of pneumonia, the patient may need an oxygen mask to help them breathe. In the more severe cases, it may even be necessary to place them on a ventilator. Meningitis will also likely be treated with antibiotics, and the patient will likely need to be hospitalized. Getting treatment for the patient as soon as possible will help prevent serious complications from developing.