What Is Tracheitis?
Tracheitis is an acute inflammation of the upper throat that makes it painful and sometimes hard to breathe. It can occur from a viral infection or a trauma to the windpipe. Often it is not dangerous, but in severe cases it may require hospitalization and treatment to reopen the airway.
In the beginning stages, tracheitis resembles several other respiratory illnesses, and is thus tricky for doctors to diagnose. Children are the most susceptible. Find out what causes this uncommon illness, how to treat it, and more.
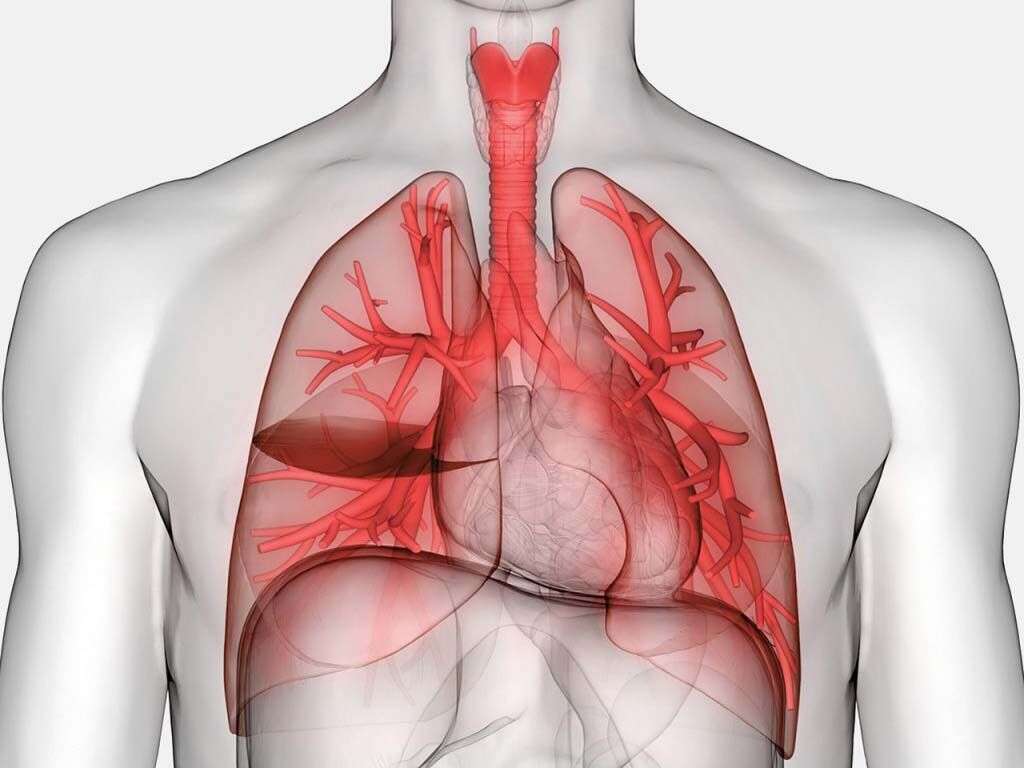
1. Throat Anatomy
When you inhale air or swallow food, both substances first hit the back of the throat, or pharynx. Food and air then diverge into two separate tubes, with the route for food ending in the stomach and the one for air spreading toward the lungs. A flap called the epiglottis separates the two paths.
After passing the pharynx, air goes down a passageway in the front of the throat called the larynx, also known as the voice box. Below this is the trachea. The trachea then branches into two more tubes (bronchi) that continue into the lungs. Tracheitis is an inflammation of any or all of these structures: larynx, trachea, and bronchi.
2. Symptoms
Patients first experience the familiar symptoms of an upper respiratory infection, including sore throat, runny nose, and cough. The symptoms may then worsen to include high fever, rapid breathing, bluish skin, barking cough, and a whistling sound when inhaling (inspiratory stridor).
Inside the body, white blood cell numbers rise as the larynx, trachea, and bronchi all become inflamed in an attempt to fight a growing bacterial infection. This immune response also triggers membranes inside the trachea to secrete mucus. These adherent or semi-adherent membranes further narrow the passageway for air and make it even more difficult to breathe.

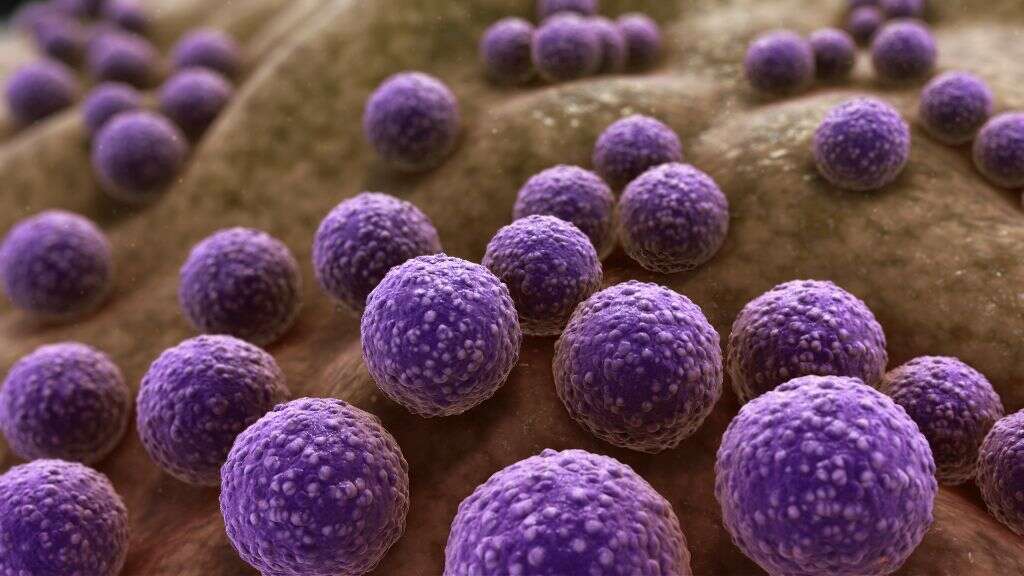
3. Causes
Doctors do not know the exact cause of tracheitis, but the disease tends to occur after another viral infection like influenza or a bacterial infection like pneumococcus has previously weakened the immune system. Trauma to the throat from medical procedures can also cause tracheitis. For example, a tracheostomy or an endotracheal tube can cause lesions that are vulnerable to bacteria.
Strains of Staphylococcus and Streptococcus bacteria that secrete toxins can cause tracheitis and also organ failure when they grow inside the trachea. Other pathogens responsible for tracheitis include the following: Moraxella catarrhalis, Haemophilus influenza type B, Bacteroides, Prevotella, and Mycoplasma pneumonia. Methicillin-resistant S. aureus (MRSA) is an antibiotic-resistant bacterium that has recently become implicated in cases of tracheitis in the U.S.
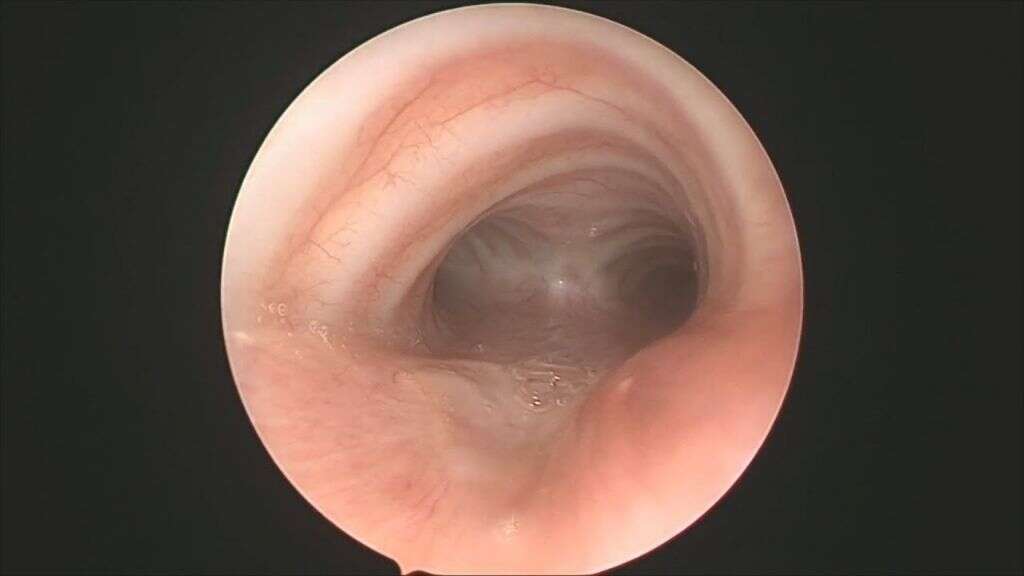
4. Diagnosis
Tracheitis is notoriously hard to diagnose, but doctors often test for it when children have symptoms of croup that do not respond to treatment. Besides a white blood cell count, a sample of fluid from the trachea is taken and cultured to determine whether bacteria are present.
The most conclusive way to diagnose tracheitis is through laryngotracheobronchoscopy. In this technique, a surgeon inserts a rigid telescope into the trachea of an anesthetized patient to get a direct view of the inflammation. If this technique is not available, X-rays can provide some information about the condition of the trachea.
5. Oxygen Therapy
The most serious problem for people with tracheitis is lack of oxygen due to a partially closed airway. A bag-valve-mask ventilator can be used to stabilize a patient temporarily. For longer-term care, babies receive oxygen by lying in an oxygen tent or breathing via soft prongs placed inside their nostrils.
More than half of patients with tracheitis require intubation to supply oxygen directly into the lungs. The tube is attached to a ventilator, which then breathes for the patient. When the doctor observes fewer tracheal secretions and the patient is able to breathe independently, the tube is removed.

6. Drug Treatment
Racemic epinephrine is the medicine given to patients with severe respiratory tract infections. This medicine improves breathing by dilating the capillaries and thus widening the trachea to allow more airflow. Showing no signs of improvement after taking this medicine is one sign of tracheitis.
Antibiotics are effective at killing the bacteria responsible for inflammation and blocked airways. A doctor administers them intravenously, through an IV bag attached to a vein in the patient’s arm. Cephalosporin, penicillin, vancomycin, and clindamycin are some of the antibiotics typically used.

7. Occurrence
Tracheitis is a rare condition. Worldwide, there are 0.1 cases per 100,000 children per year. In the U.S., the greatest number of cases occur during the fall and winter, with some experts citing an incidence of 4 to 8 cases per 1,000,000 children. Some areas, for example the Ohio River Valley, have disproportionately larger numbers of cases than other parts of the country.
Although all ages are susceptible, this illness most severely affects young children. Most patients range in age from a few weeks to 16 years old, with a mean age of 4 to 5 years. Boys with tracheitis outnumber girls by a ratio of 2 to 1.

8. Prognosis
Patients who receive oxygen and antibiotics during the acute stage of illness usually recover completely. They improve significantly within 5 days and remain hospitalized for an average of 3 to 12 days. Most suffer no permanent damage to the trachea.
Mortality occurs in 4 to 20% of patients, with the primary cause of death being lack of oxygen to the brain. Septic shock causes 2 to 6% of deaths, cardiorespiratory arrest causes 2 to 3%, and acute respiratory arrest causes 1 to 3%. Other causes of death like cardiac arrest, cerebral anoxia, pulmonary edema, pneumothorax, and toxic shock syndrome are rare and result in 1% or less of patient deaths.

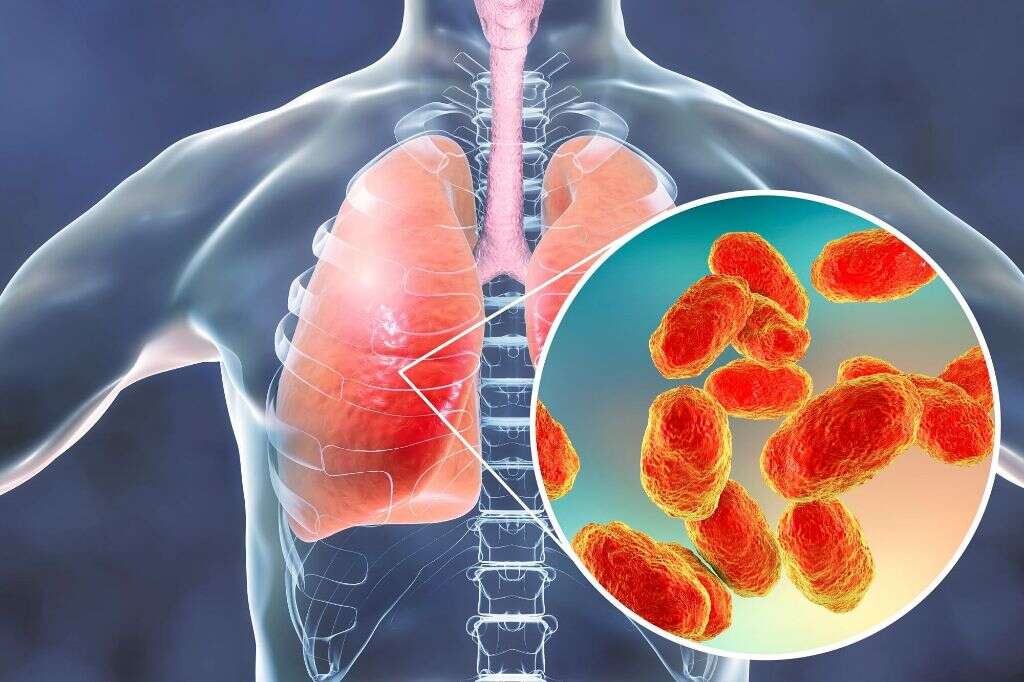
9. Complications
Pneumonia is a complication that occurs in 19 to 60% of tracheitis cases. Hospital-acquired pneumonia occurs when bacteria in a medical setting grow inside a person’s lungs. Health care workers can spread these bacteria, and patients on ventilators are especially at risk.
Other complications of tracheitis include damage to the airway as a breathing tube is inserted or removed. Complications also can occur if a doctor decides to remove the tube before a patient can breathe independently; sometimes this happens by accident. Other complications are related to bacterial infections that spread into the bloodstream such as septicemia and toxic shock.
10. Prevention
Because tracheitis most often occurs after a previous infection, keeping children up-to-date on their vaccinations is an important means of prevention. Hib meningitis, measles, and influenza are all serious illnesses that can be prevented. Vaccines are especially important for immunocompromised children.
People can prevent the respiratory infections that lead to tracheitis by maintaining good hygiene. Teaching children to wash their hands properly is an effective way to keep them healthy. When water is not available, hand sanitizer is a good alternative.