What Is Pericarditis?
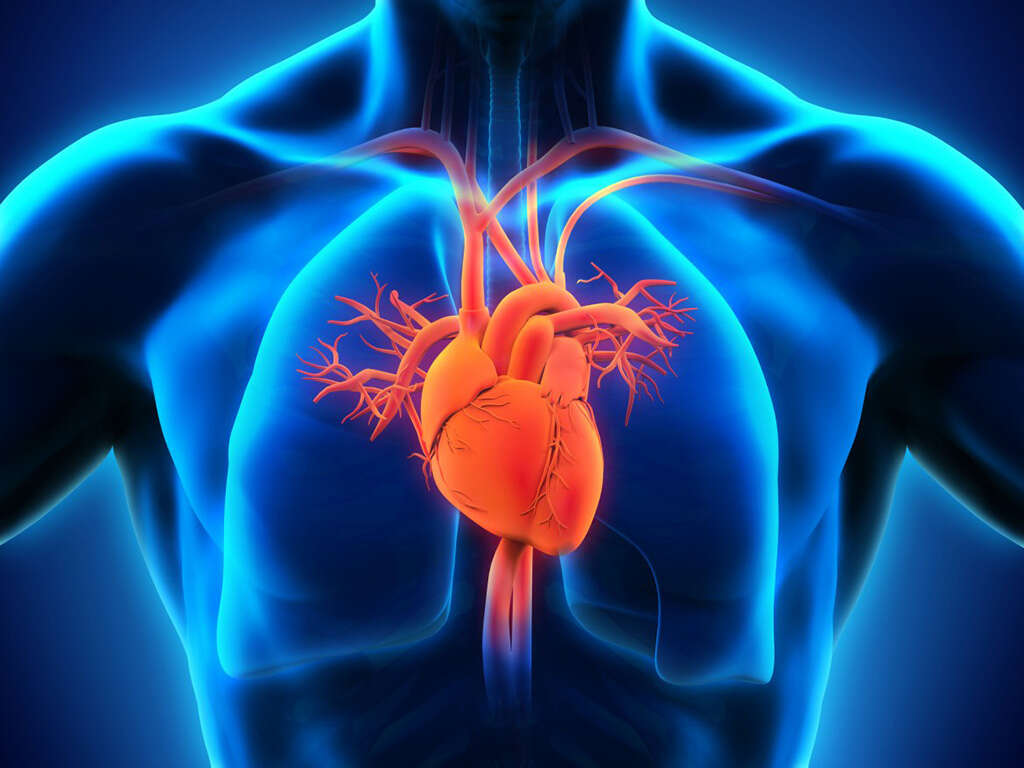
The pericardium is a flexible two-layer membrane that surrounds the heart. There is a thin layer of fluid that separates the layers of the pericardium, allowing free movement. The heart is a vulnerable organ in the body and plays a vital role in sustaining life. The pericardium acts as a supportive and protective layer, keeping the heart in place and preventing potential infection.
Pericarditis results from inflammation of the pericardium, causing rubbing of the two layers as the heart relaxes and contracts. People experiencing pericarditis may describe the symptoms as similar to a heart attack, with an irregular heartbeat and chest pain.

1. What Are the Causes of Pericarditis?
Pericarditis can have many origins, and as the condition presents uniquely in different patients, it is difficult to profess one root cause. However, most cases stem from an infection or a virus. When a cause is unknown, doctors may present a diagnosis of idiopathic pericarditis.
Heart surgery may also result in the condition. Researchers believe the agitation to the heart muscles during surgery leads to the inflammation of the pericardium. When surgery or other cardiac event is the underlying cause, Dressler’s syndrome, an autoimmune condition, may be the cause. Researchers suggest dead heart tissue in the blood system could trigger the immune reaction against the pericardium.

2. What Are the Symptoms?
Symptoms of pericarditis are like a heart attack. Patients may experience palpitations, shortness of breath, swelling in the legs or abdomen, minor fever, weakness, cough or pain in the shoulder. They will also experience pain in the chest, although the pain may present in a central location or to the left, decreasing when leaning forward or sitting up.
While pericarditis is not a heart attack, it is difficult or impossible to tell the difference without a medical assessment. Anytime you experience chest pain, consult with your doctor, allowing them to determine the underlying condition and determine the cause of the pericarditis.
3. What Are Common Patient Characteristics?
Pericarditis is a common heart condition, and it can affect people of all ages and ethnicities. While women can present with the disease, variations of pericarditis are more likely to show in men between the ages of 20 and 50 years old; however, that does not mean that the heart problem will not affect patients outside of this parameter.
The condition can present in a variety of ways. Between 15% and 30% of patients diagnosed with acute pericarditis experience it again, and some of those patients end up developing chronic pericarditis.
4. What Are the Categories of Chronic Pericarditis?
Researchers may split chronic pericarditis into two categories: incessant and intermittent. The class of the chronic condition depends on patient treatment. If pericarditis reoccurs after six weeks of weaning treatments for the acute condition, it is incessant. However, if it occurs after reducing treatments, it is intermittent.
While most clinicians prefer the two-category system, some will break the condition down further into fluid types. There are five further classifications of the disease: hemorrhagic, fibrinous, caseous, purulent and serous.

5. What Are the Possible Complications of the Condition?
Complications of pericarditis typically result from non-treatment. When any condition is left untreated, it is likely to worsen over time. With pericarditis, the illness can become severe without medical intervention, often developing into one of two conditions: cardiac tamponade or constrictive pericarditis.
Choosing to leave pericarditis untreated can lead to a fatal blood pressure drop resulting from excessive fluid in the pericardium. The fluid buildup can prevent the heart from filling with blood, which results in cardiac tamponade.
Constrictive pericarditis, while rare, causes scarring and the thickening and hardening of the pericardium, restricting the heart muscle. While restrictive pericarditis may not be fatal, it can cause uncomfortable swelling of the legs and feet and shortness of breath.
6. How Is the Condition Diagnosed?
The diagnosis of pericarditis begins with an initial examination. The doctor will listen to the chest for the rubbing of the pericardial layers. The friction between the layers can create a distinctive sound. If the sound is present and other symptoms align with the diagnosis, then the physician will order further diagnostic testing to confirm.
Several diagnostic tools may help confirm the pericarditis diagnosis: chest X-ray, MRI, CT, electrocardiogram, or an echocardiogram. X-rays can offer a good depiction of the fluid buildup around the heart, but a CT provides a more detailed image.

7. What Are the Treatment Options for Pericarditis?
The treatment for pericarditis depends on the severity of the illness. For minor cases, a doctor may prescribe no action, choosing to let the illness run its course. When dealing with a mild to severe case, a doctor may prescribe drug-based treatment options, ranging from over-the-counter medications to prescriptions, like colchicine or corticosteroids; however, doctors prefer not to prescribe steroids as it may cause a relapse.
In severe to extreme cases of pericarditis, surgery may be the best option for the patient. The two most common operations are pericardiocentesis and pericardiectomy, with the latter being more extreme, resulting in the removal of the pericardial sac. Depending on the invasiveness of the surgery, recovery may last anywhere from a few days to a few months.

8. How Do a Heart Attack and Pericarditis Relate to Each Other?
First, it is necessary to stress that pericarditis does not cause a heart attack, especially when treated. However, the condition may result from a previous heart attack. The presumption is that the agitation caused by the initial attack may traumatize the surrounding sac, resulting in inflammation of the tissue.
Also, like with heart surgery, an attack can cause dead heart tissue to enter the bloodstream, which results in an autoimmune reaction. A patient’s immune system attacks or reacts to the pericardium, causing inflammation.

9. What Is the Outlook for Patients?
Pericarditis is typically a nonlethal illness that resolves quickly with rest and minor medical intervention. Most patients will not experience another attack because only a small percentage of sufferers develop chronic pericarditis.
However, if a patient does not receive treatment for the condition, then it can worsen. Progression of the illness can cause life-threatening situations. Always consult with your physician whenever you experience significant chest pain. Do not assume that these symptoms are typical digestive discomfort, especially when prolonged.

10. Where Can You Go to Get Help?
Your doctor is the primary source of help and consultation on pericarditis. However, you can review informational medical websites and those dedicated to the condition. If you suffer from pericarditis, you are not alone, and you can find support through online and local communities and networks.
Pericarditis is a heart condition affecting the pericardial sac. While most cases resolve without medication or surgical intervention, you still need to seek a doctor’s opinion. If you have any more questions, contact your doctor.