What Is Erysipelas?
Our skin is perhaps our first barrier of defense against harm. It helps to prevent us against physical harm and it also helps to prevent us against diseases. It is also very effective at helping to keep us safe, but it is not impervious. We will sometimes be harmed, and our skin itself can sometimes be harmed directly.
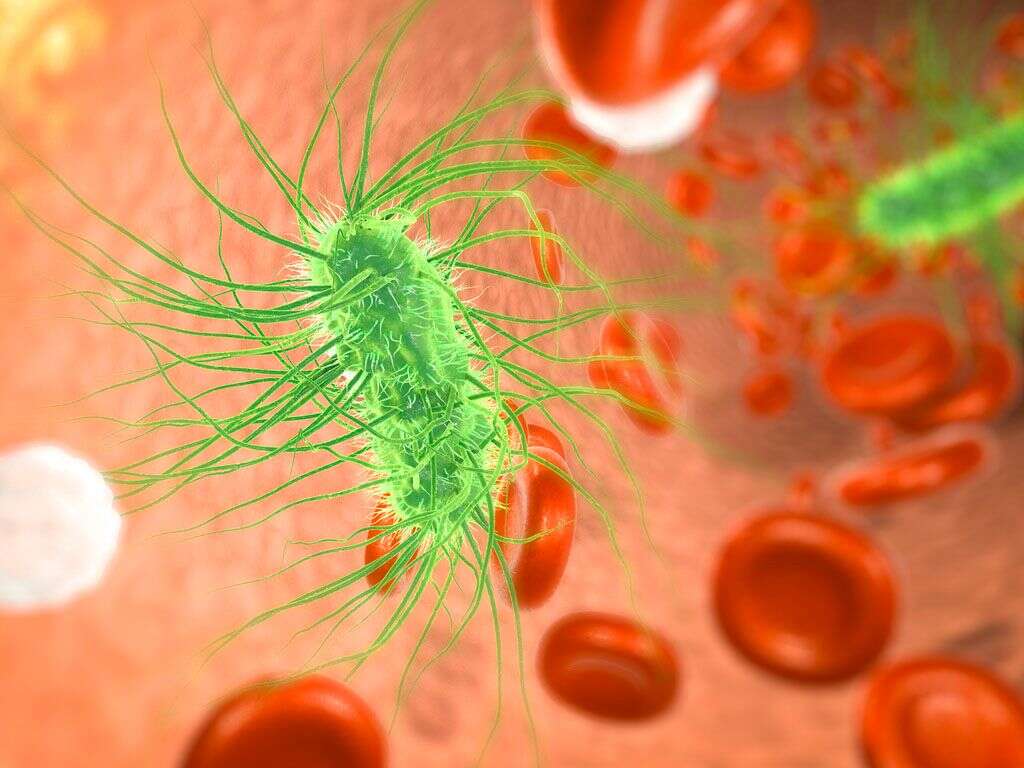
At any one time, our skin is likely to be covered in bacteria. The vast majority are harmless, but some can cause problems if we are unfortunate. Some pathogens will infect our skin if given the opportunity to do so, and one example of such an infection is erysipelas.

1. What Is Erysipelas?
Erysipelas is a condition that affects the upper layer of the skin. It is a bacterial infection and is another form of another type of skin infection that affects the lower layer of the skin. The other condition is known as cellulitis, and cellulitis can be serious in some cases. Erysipelas is, thankfully, not usually a serious condition.
Although it is not usually serious, Erysipelas can still be uncomfortable and unsightly. It should be treated because otherwise it might develop into something that can be dangerous for the patient. Thankfully, treatment is fairly straightforward so it is uncommon for erysipelas to become dangerous.

2. Group A Streptococcus
The bacteria responsible for erysipelas is known as group A Streptococcus. This is actually a fairly common type of bacteria that is also responsible for another well known disease: strep throat. The bacterium is often found on your skin and, the vast majority of the time, it will cause no harm at all.
Your skin is usually an impenetrable barrier for most bacteria. If the skin is broken in some way, however, then it can provide an opportunity for the bacteria to get through. There are various ways in which the skin can be broken in a way that allows the bacteria to penetrate.

3. Causes
Our skin is able to resist quite a lot without being damaged. It’s flexibility also means it can flex instead of breaking under pressure. It is far from indestructible, though, and there are various ways the skin can be broken. Among the most common of all is some form of injury, and this can include wounds that were caused by surgery procedures.
People that have skin ulcers are more also more prone to developing erysipelas, and other skin conditions like psoriasis can also cause it. Edema, which is swelling, can also cause the skin to become broken, and insect bites can also make a way for the bacteria to enter the body. Injecting drugs is potential another cause.

4. Symptoms
While erysipelas is not usually dangerous, it can still cause some very unwelcome symptoms. These include a fever, chills, and malaise. The presence of an infection can cause the patient’s glands to be working harder than usual and this can cause them to become swollen.
The infected area can become red and swollen, and there can also be a raised edge around the infected area. Blisters will also appear on the infected area in some cases. Erysipelas will sometimes be located on the patient’s face, and this can cause the patient’s face to become swollen, especially their cheeks and their nose.

5. Complications
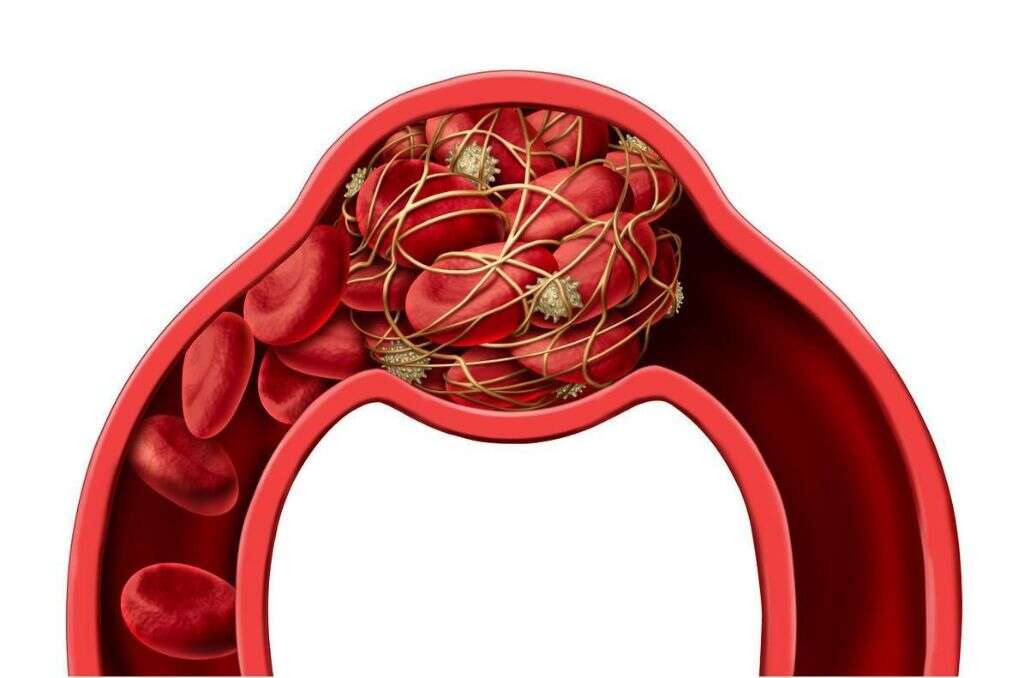
As mentioned, erysipelas can cause serious complications if treatment is not found in time. For example, abscesses can form and these can themselves lead to further problems. It can also result in blood clots which are also potentially dangerous, while the patient’s blood can also become infected.
Some people will develop infections in their bones and joints. The patient’s heart valves can also become infected, which can affect the heart’s ability to pump. The disease can also cause the death of the patient’s bodily tissues in another serious condition known as gangrene. The infection can even reach the patient’s brain in some cases.
6. Who’s at Risk
Erysipelas can infect anybody, but some people are more prone to it than others are. This includes older people, particularly those that are over the age of 60. Young children between the ages of 2 and 6 years old are also in a higher risk bracket. Extra precautions should be taken where practical to help prevent the risk of these people becoming infected.
Our immune systems will usually be able to fight off the bacteria if/when it enters the body. This depends on the immune system being strong enough to do so, however. Thus, people whose immune system have been weakened are at a higher risk of erysipelas. This includes people with illnesses like HIV/AIDS, and people taking certain medication.

7. Prevention
Because the bacteria responsible for erysipelas is so common, it means it is all but impossible to prevent it from happening. However, taking some simple precautions will help to keep you safe from the infection. One of these is to make sure that any wounds you might have are kept as clean as possible all the time.
Some diseases can cause the skin to become very itchy and it can be extremely difficult to resist scratching it. Excessive Scratching can break the skin, and this can leave the patient prone to erysipelas. If you have dry skin that cracks, try using moisturizers to help prevent the cracking. Also make sure to keep on top of treatment for any other skin conditions that you might have.

8. Diagnosis
When you see a doctor about your symptoms, they will want to perform a physical exam on you. This will involve checking the infected area and to see if other parts of the body are affected also. They may also need to ask about any other symptoms you might have. A doctor is also likely to ask you questions about your medical history.
In most cases, a brief physical exam and knowledge of the patient’s medical history will be enough to make a diagnosis. If the doctor is not sure, however, then additional tests may be needed. This can mean blood samples and tissue samples that will help to look for the group A Streptococcus bacterium.

9. Medication
In the majority of cases, erysipelas will be relatively straight forward to treat. An antibiotic should be enough to overcome the bacteria, and this can cure the patient of their condition. Antibiotics are not always effective, however, and this will mean that a different type of drug will need to be used instead.
If the condition is serious enough then hospitalization may be deemed necessary. This will allow doctors to administer antibiotics intravenously, which are likely to be more effective against the bacteria. If the condition is considered to be serious enough, then it might be necessary to perform surgery on the patient.

10. Surgery
If the heart’s valves have been damaged enough then they might need repairing or replacing altogether. Surgery might also be deemed necessary if the infection has resulted in blood clots in the circulatory system. Surgery might also be performed if the condition has resulted in gangrene.
Surgery for gangrene will generally involve removing dead tissues. This is necessary in order to help prevent the spread of the gangrene infection. In extreme cases, it might even be necessary to perform an amputation. Gangrene is an extremely serious condition and the patient will likely die if suitable treatment is not found in time.