What Is Endometriosis?
Endometriosis is a condition where there is normal endometrial cells (from the uterine lining tissue) found in other locations besides the uterine cavity. It is most commonly found to occur in the fallopian tubes, ovaries, tissue around the uterus, and other parts of the body (rare). This tissue is capable of responding to the normal hormonal (menstrual) cycle.
It is a common condition that is debilitating and poorly understood. The patient is often greatly affected not only by severe pain but also the possibility of the impact of disease on fertility. It is a disease that is commonly misdiagnosed as it has similar symptoms with fibromyalgia, interstitial cystitis, pelvic inflammatory disease, and irritable bowel syndrome.
1. Pathophysiology
Although the exact mechanism is still unclear, there have been various theories that have been proposed. The pathophysiology is most likely to be multifactorial. As previously mentioned, endometriosis occurs when endometrial (uterine lining) tissues are found in other parts of the body besides the uterus. It is most commonly located in the dependent portions such as the ovaries, tubes, uterosacral ligaments, posterior, and anterior cul-de-sac. These tissue then respond to the hormone cycle resulting in proliferation, secretion, and sloughing of the menstrual material. These material then cause inflammation and scarring resulting in pain, formation of adhesions, and distortion of anatomy.
2. Risk Factors
Some of the risk factors for endometriosis include early age of menarche (first period), family history of endometriosis (six fold increase in incidence if there is an affected first-degree relative), heavy bleeding during menses (menorrhagia), short menstrual cycles (less than 27 days), and long duration of menstrual flow (more than 7 days).
Additional risk factors include: delayed childbearing, iron deficiency, hypoxia (low oxygen), defects in the fallopian tubes and uterus (such as obstruction of menstrual outflow), altered immune response, environmental toxins (such as dioxins), late menopause, and iatrogenic deposition (due to gynecologic procedures such as cesarean sections).

3. Statistics
In the United States, endometriosis is estimated to occur in 6% to 10% of women with 4 in 1,000 hospitalized annually. However, the exact incidence is unknown as definitive diagnosis requires a biopsy or visualization via surgery. Since it is an estrogen dependent disease, it generally affects women in the reproductive age group. Among infertile women, endometriosis has a prevalence of 20% to 50% while the numbers increase to 71% to 87% among women with chronic pelvic pain.
In a study involving adolescent females that have chronic pelvic pain, 45% of the study participants were diagnosed with endometriosis after laparoscopy. In the same study, 12% were 11 to 13 years old while 45% were 20 to 21 years old. Studies have not found any differences in incidence among different ethnic or social groups.

4. Patient History
Patients with endometriosis tend to be nulliparous (no history of childbirth) and have short menstrual cycles where there is prolonged flow (of 8 days or more). The pain is often followed by flow and generally resolves after 1 to 2 days of menstruation. The symptoms also generally improve after menopause and during pregnancy with recurrence after delivery or hormone replacement therapy.
These patients also may have a family member (first-degree relative) who has endometriosis. In some patients, the product from sloughing can become entrapped due to a cyst formation resulting in a mass known as an endometrioma. While it can occur in any location, it is most commonly located in the ovaries. This mass can become painful and, if ruptured, causes an acute surgical abdomen.
5. Symptoms
Some patients may remain asymptomatic. The degree of pain is correlated with the depth of tissue infiltration and intra-abdominal or intrapelvic adhesions. Besides pain during menstruation (dysmenorrhea), patients may also experience sleep disturbances, generalized muscle pain, fatigue, menorrhagia (heavy bleeding), irregular bleeding, lower back or abdominal pain, pelvic pain, dyschezia (pain during defecation), cycles of constipation and diarrhea, dyspareunia (pain during sex), inguinal pain, vomiting, nausea, bloating, pain during exercise, dysuria (pain during urination), increased urinary frequency, and more.
Another rare symptom is bleeding at uncommon sites during menstruation such as at the umbilicus, perineum abdominal wall, and surgical scars.

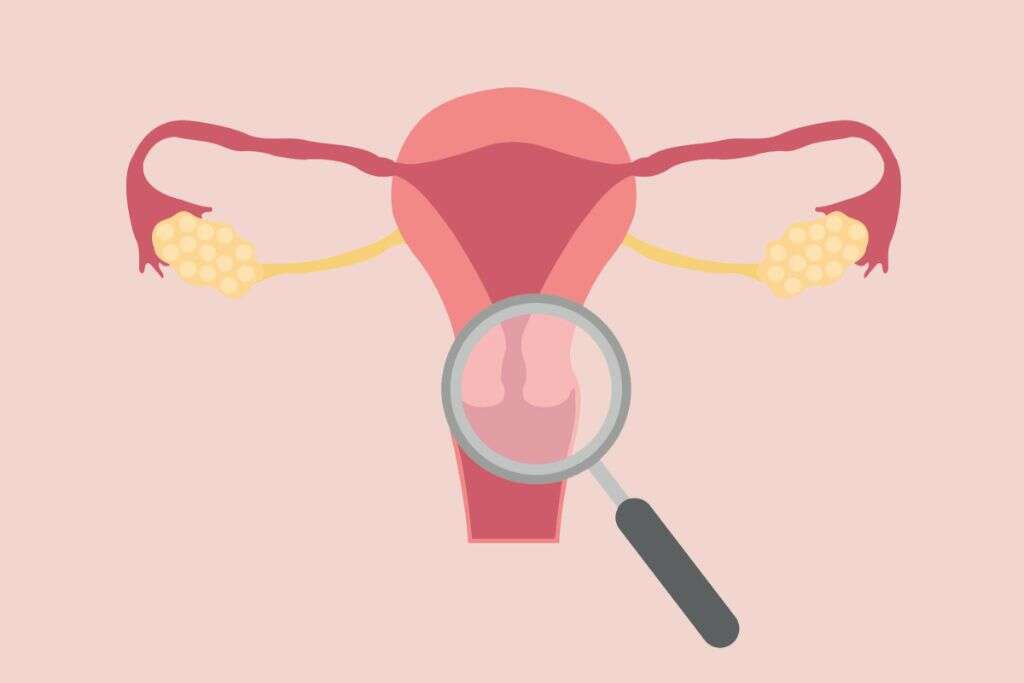
6. Diagnosis
There are few laboratory tests that can be beneficial in the diagnosis of endometriosis. However, there may be some that can help to rule out certain diseases. Computed tomography (CT) scans, pelvic ultrasonography, and magnetic resonance imaging (MRI) are only useful in advanced disease where there is an endometrioma or anatomical distortion.
Since visualization of the ectopic tissue is the definitive method of diagnosis, laparoscopy (minimally invasive surgery) is the procedure of choice. Additional laboratory studies that may be beneficial are complete blood count (CBC), urinalysis, urine culture, CA-125 levels, detection of autoantibodies against Thomsen-Friedenreich antigen, and CCR1 levels.

7. Treatment and Management
Since the symptoms of endometriosis occur according to the cyclical hormones, the medical therapy will be based on the cycle. Some of the medications include progestins, oral contraceptive pills, gonadotropin-releasing hormone (GnRH) agonists, aromatase inhibitors, and androgens.
Women who preserve their reproductive potential have a 44% chance of recurrent pain for surgical management and 53% for medical management. To help with conception, options include in vitro fertilization, superovulation, and intrauterine insemination. Other medication that may help but have little to no evidence to support their clinical use for endometriosis are nonsteroidal anti-inflammatory drugs (NSAIDs), opioids, pentoxifylline, statins, cyclo-oxygenase-2 inhibitors, and angiogenesis inhibitors.
8. Complications
Endometriosis is a progressive disease that can result in various complications such as adhesions (fibrous bands forming between organs and tissue), chocolate cysts of ovaries (endometrioma), pelvic cysts, internal scarring, bowel obstruction, ureter obstruction, ruptured cysts, and endometriosis associated infertility. When endometriosis affects the ovary, it can cause complications in pregnancy due to potential rupture and abscess.
When endometrial tissue is found in the thorax (thoracic endometriosis), the patient may experience recurrent pneumothoraxes (catamenial pneumothorax) that coincides with menstruation. A study involving 12,000 women with endometriosis over a 20-year duration found that women under the age of 40 diagnosed with endometriosis are 3 times more likely to develop heart-related issues compared to their peers.

9. Prognosis
In one-third of women with endometriosis, the condition has been found to resolve on its own without treatment. However, it is a progressive disease with unpredictable disease extent that can lead to complications. While as many as 95% respond to treatment for pain, therapy for infertility is generally ineffective. As many as 50% experience a return of their symptoms within 5 years with treatment; 80% to 85% of patients experience pain relief with a combination of estrogen and progestins while 90% reported adequate pain relief after 6 months of danazol therapy.
To improve fertility rates, minimally invasive surgery can be beneficial. Surgery (total hysterectomy with bilateral salpingo-oopherectomy - removal of uterus and ovaries) is the best chance for resolution of pain. About 30% to 40% of patients will be subfertile.

10. Patient Education
Patients should be educated regarding the importance of completing the full 6-month medical therapy. They should know that although the medical therapy may often help with pain relief, it may cause uncomfortable side effects. The healthcare team, friends, and family should help to encourage the patient to ensure she finishes the treatment course. After treatment, any recurrence of symptoms should prompt the patient to return for another evaluation.
Patients with severe cases of endometriosis should also be educated regarding the symptoms of ureteral and bowel obstruction as this can be an emergency. They should also be informed regarding available support groups and other important resources that may help with morale and encouragement.