What Is Depression?
About 67% of individuals with depression are unaware that they are going through a treatable condition and, therefore, do not seek professional help. In some cases, the social stigma and persistent ignorance by the general public including many medical providers has led them to believe that it is a condition that can be wished or willed away. When many of these patients first seek treatment, they often present with vague somatic symptoms.
The Diagnostic Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) has classified the depressive disorders into different types. It can be further subdivided based on specifiers. The common features are often the presence of irritability, sadness, and somatic and cognitive changes, but differs based on timing duration and cause. This article will focus on major depressive disorder (MDD) in adults. MDD (or often referred to as depression) is a condition where there is at least 2 weeks of low mood accompanied by other symptoms.

1. Causes
The exact mechanism for MDD is unclear. Like most psychiatric conditions, it is believed to be due to multiple factors involving both genetics and environmental. Based on twin and family studies, depression seems to develop in early childhood and appears to be related to psychosocial influences.
Meanwhile, adolescent and adult onset depression appears to be more heritable. Genetics have been proven to play a crucial role in the development of MDD. Those with a first-degree relative with depression are 3 times as likely to develop depression. Although MDD can occur without precipitating stressors, the presence of interpersonal losses and stress can increase the risk of MDD. MDD is also more likely in the presence of medical illness, chronic pain, and psychosocial stress.

2. Risk Factors
As previously mentioned, the risk of MDD increases when there is a first-degree relative with depression, presence of chronic pain, existing medical illness, psychosocial stress, impaired social support, loneliness, caregiver burden, bereavement, and the occurrence of negative life events.
Those with Parkinson’s disease, Alzheimer’s disease, stroke, macular degeneration, cancer, multiple sclerosis, and seizure disorders have also been associated with a higher risk of depression. Alternatively, one study found that depression in early life increases the risk of Alzheimer’s disease. There are also studies that have reported depression due to poor parent-child interaction. This was observed when adults with depression reported that they had high maternal overprotection and low paternal involvement.

3. Statistics
From 2009 to 2012, it was estimated that 7.6% of Americans aged 12 years and above had depression. It is more common among females and those between the ages of 40 to 59 years old compared to other age groups. In 2015, about 16.1 million (6.7%) individuals 18 years or older had experienced at least one major depressive episode.
Globally, the prevalence rates of depression among adults are similar to the United States. However, data regarding adolescents and children is sparse. One study showed that the incidence of depression in preschool children to be 0.9%, in school children to be 1.9%, and in adolescents 4.7%. Another study showed more than 11% in male high school students and 22% in female high school students. Although rates of depression are highest in those aged 24 to 44 years old, the incidence increases with advancing age, especially when there is illness.

4. Signs and Symptoms
Some patients may not present with typical symptoms. When they first seek treatment, symptoms are often somatic and vague such as headache, abdominal distress, fatigue, and changes in weight. There may be difficulty concentrating and irritability instead of low mood or sadness. In children, symptoms may include social withdrawal and a decline in school performance. In the elderly, there can be a decline in functioning, confusion, and cognitive symptoms. A thorough family history is important as depression can be familial.
Symptoms to look out for include heaviness, sadness, numbness, anhedonia (loss of interest in activities they once loved), hopelessness, guilt, worthlessness, and ruminative thinking. When there are symptoms of psychosis, a careful history evaluation is required to rule out schizophrenia, bipolar, and substance abuse.

5. Physical Examination
A physical examination in a patient with suspected MDD should be performed to rule out organic conditions that may imitate depression. Most organic conditions that may imitate depression are infection, side effects of medication, tumor, endocrine disorder, and neurologic disorder.
In patients with severe MDD, there may be a decline in grooming, hygiene, and weight. This means that the patient may appear unkempt, withdrawn, disheveled, and gaunt. Family members may report a loss of reactivity, spontaneous movement, and a lack of emotional expression. The patient’s speech may become slow and lacking in content. Disorganized speech prompts evaluation for psychosis while pressured speech suggest mania or anxiety.

6. Diagnosis
Diagnosis is conducted by a trained psychiatrist or general practitioner. The assessment includes a mental state examination. The most commonly used criteria for diagnosis is based on DSM-5 where at least 5 of the following need to be present in the same 2-week period: depressed mood, diminished pleasure or interest, significant weight change or disturbance of appetite, sleep disturbance, psychomotor retardation or agitation, fatigue, feelings of worthlessness, diminished concentration or ability to think, and recurrent suicidal thoughts or presence of a suicide plan.
These symptoms should not be due to another medical condition, substance use, not better explained by another disorder, and cause significant distress or impairment in functioning. Depression can be mild, moderate, or severe. It can also occur with psychotic symptoms.

7. Treatment and Management
In MDD, treatment includes psychotherapy, medication, and electroconvulsive therapy (ECT). For individuals under 18, psychotherapy is the therapy of choice. Based on the 2004 guidelines from the National Institute for Health and Care Excellence, antidepressants should not be prescribed for mild depression due to a poor risk-benefit ratio.
Antidepressants should be used in combination with psychosocial interventions for those with moderate or severe depression or long-term mild depression. Antidepressants should be used for 6 months to decrease the likelihood of relapse. The American Psychiatric Association recommends an individually tailored treatment plan that involves options such as medication, psychotherapy, ECT, exercise, light therapy, and transcranial magnetic stimulation. Psychotherapy options include cognitive behavioral therapy, family therapy, and interpersonal therapy.

8. Prognosis
MDD has significant potential mortality and morbidity due to the possibility of suicide, disruption in relationships, substance abuse, and absence from work. Seventy percent to 80% of individuals can achieve a significant reduction in symptoms with proper treatment. However, it is important to note that as many as 50% may not respond to the initial treatment trial.
At 1 year after diagnosis, 20% will continue to meet the criteria for MDD while an additional 40% will experience partial remission. The presence of psychotic symptoms and irritability before treatment may mean poorer outcomes. Based on the American Academy of Child and Adolescent Psychiatry, a history of dysthymia, anxiety disorders, a previous depressive episode, and subsyndromal symptoms of depression increases the risk of future depression. Those with late-onset depression have a poorer prognosis compared to younger patients.

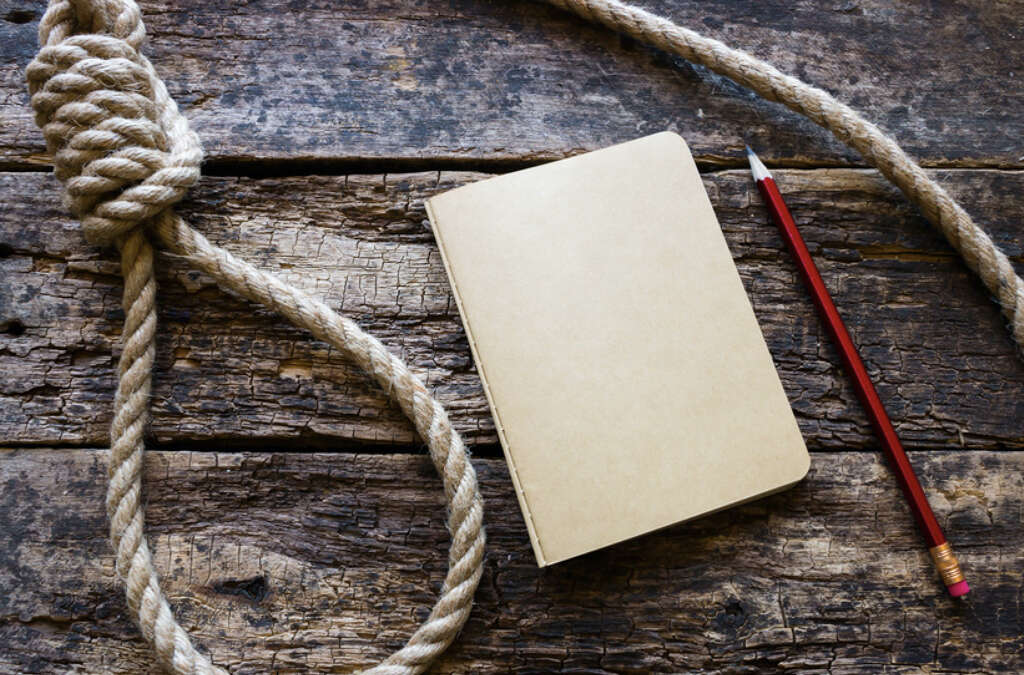
9. Suicide
Depression plays a significant role in suicide attempts. Those with untreated depression have a 20% lifetime risk of suicide. In 2009, suicide was reported to be the 10th leading cause of death, accounting for 36,909 deaths in the United States.
The highest suicide rate is among men above the age of 75 years old. Caucasian men complete more than 78% of all suicides with 56% of deaths involving firearms. Among females, attempted suicide is more common, with poisoning being the predominant method. The risk factors of suicide include depression, history of suicide attempts, stressful life events, medical illness, widowed or divorced, lack of social support, presence of gun in the home, high anxiety, rehearsal of the plan, and lack of reason not to commit suicide.
10. Patient Education and Support
Patient education plays an important role in the treatment of MDD. It helps increase awareness among patients and their family members so they may seek early treatment in the case of relapse. When the patient and their family members are involved in the treatment plan, it can increase compliance to medication and therapy. Referral to counseling may be recommended.
Having an engaging family can be crucial in pediatric and late-onset depression. This is due to their role of being helpful informants and ensuring compliance to medication. Since family members tend to spend more time with the patients, they are also more able to motivate and encourage patients to change behaviors that perpetuate depression. Both patients and family members can also obtain more resources and support from support groups, online forums, and various organizations.












