What Is Dysthymia?
Most everyone knows that depression is a condition associated with feeling down and out, but few outside of the mental health profession realize the diverse forms it can take. Depression can be severe or mild, sudden or long-lasting, and even psychotic or bipolar. Dysthymia is one type of depression with distinct characteristics and manners of affecting a person’s well-being.
Dysthymia, or persistent depressive disorder (PDD) as it is more accurately called, is one type of depression. The symptoms have a subtle onset and their effects have been described as insidious; it is, therefore, one of the more difficult forms to diagnose and treat. The following 10 facts will provide information about its symptoms, diagnosis, treatment, and more.

1. Internal Symptoms
Some of dysthymia’s most debilitating symptoms are not apparent to anyone but the person suffering from the disorder. Even those who are able to keep up the appearance of normality on the outside feel sad and hopeless on the inside. They have a hard time understanding how other people can be in such a good mood. They may also have trouble concentrating and go through life feeling distracted and confused.
Another internal symptom is negative self-talk. Dysthymics tend to keep up a constant dialog inside their minds that is full of criticism and self-loathing. For example, they may tell themselves how ugly they are whenever they see their reflection; or when walking into a room, an internal voice might remind them that no one likes them. This barrage of self-deprecating thoughts changes the way they value themselves and leads to low self-esteem and low confidence in their abilities.

2. Physical Symptoms
Other symptoms of persistent depressive disorder can be obvious to other people. Sufferers may stop caring about their physical appearance. They may gain or lose a substantial amount of weight as a result of their eating and sleeping patterns being disturbed. Some eat and sleep too much, while others lose the desire to do either. They are conspicuously absent from social gatherings and avoid participating in events they once enjoyed.
These physical symptoms can take a toll on the overall health of the patient. Both insomnia and hyposomnia can cause obesity and heart disease, and lack of exercise and malnutrition have similar effects. One study found those with PDD to have a death rate higher than that of the general population from physical problems unrelated to their mental condition.

3. Name Change
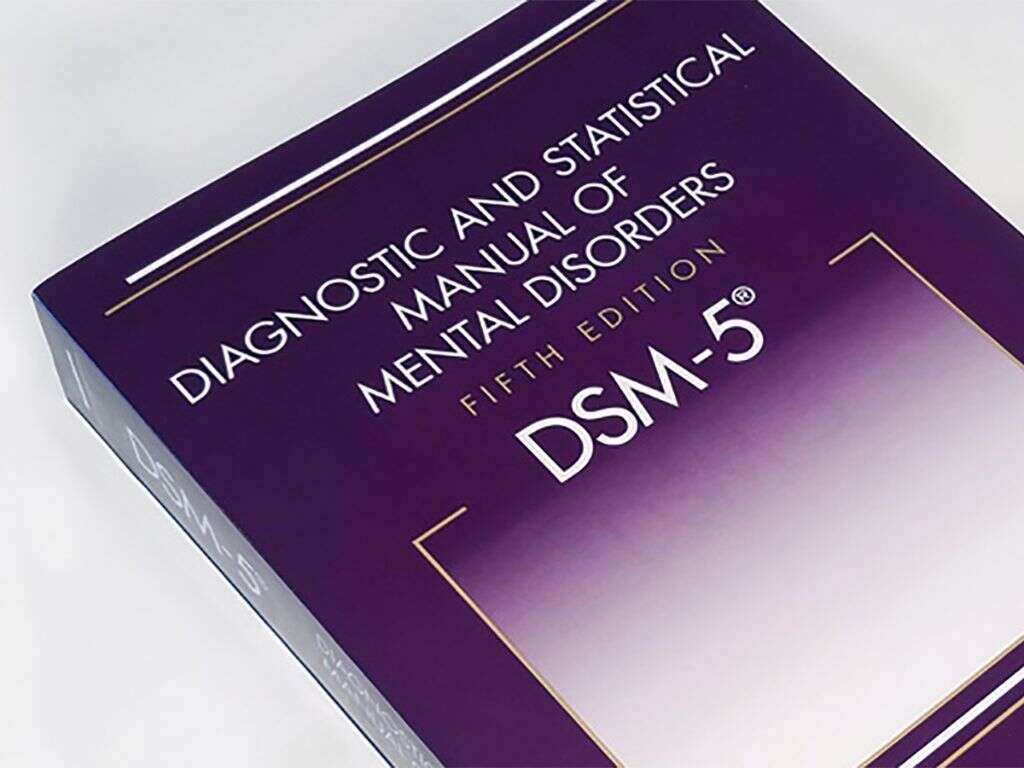
The Diagnostic and Statistical Manual of Mental Disorders describes more than at least 12 distinct types of depression. This handbook, published in 1952 by the American Psychiatric Association, catalogs every known mental illness and provides methods and criteria for diagnosing them. It is periodically updated to reflect new knowledge in the field, with the fifth revision being most recent. This current edition is frequently referred to as the DSM-5.
The word dysthymia was first coined in the 1970s as a replacement for the term’s neurotic depression and depressive personality. It was added to edition three (DSM-3) in 1980, where it was referred to as dysthymic disorder. It remained unchanged in the fourth edition, but in 2013, the editors of the newest DSM-5 merged it with chronic major depressive disorder and renamed it persistent depressive disorder.
4. Diagnosis
To differentiate between a depressive condition and a physical one, doctors usually run a series of laboratory tests. Blood tests can determine whether a patient might have a deficiency in certain vitamins or hormones that cause depressive symptoms. Blood tests can also test for the presence of psychoactive drugs. Psychological tests including the Hamilton Rating Scale of Depression or the Beck Depression Inventory then may be administered to help quantify symptoms.
The official diagnosis of persistent depressive disorder is made using criteria established in the DSM-5. To meet these criteria, the patient must have felt depressed for the majority of the day, on most days of the week, for at a minimum of two years. At least two depressive symptoms must have been present during this time, as reported by the patient or observed by others. Finally, the symptoms must either distress the patient or keep him or her from functioning well at home, work, or school.

5. Subtypes
Some professionals, concerned that dysthymia covers too broad a range of symptoms, recommend breaking the disorder into two subtypes. One subtype is anxious dysthymia, which describes patients whose condition causes them a great deal of anxiety and are likely to seek help. Their attempts at self-medication often include overeating and using drugs, such as benzodiazepines, alcohol, marijuana, or opiates. They respond well to treatment with selective serotonin reuptake inhibitors.
A second subtype is anergic dysthymia, which describes patients more debilitated by the condition. They tend to be lethargic, lack motivation, and have an inability to feel pleasure. Prescription drugs that increase natural levels of norepinephrine and dopamine hormones are better suited for this type of patient. A diagnosis of PDD can also be qualified by indicating the presence of melancholic, atypical, or mood-congruent features, or by describing it based on time of onset.

6. Treatment
As with most psychological disorders, treatment consists of medicine and behavioral therapy. Drugs typically prescribed are MAO inhibitors (phenelzine), serotonin uptake inhibitors (fluoxetine), and tricyclic antidepressants (imipramine). In the 1990s, the drug Prozac was extremely popular. A 2011 survey found that 1 in 10 Americans were prescribed an antidepressant for various forms of depression, including PDD.
Cognitive-behavioral therapy is used to change dysfunctional patterns of thinking into more realistic and productive ones. Through it, PDD patients learn to improve the content of their self-talk and to relate to other people in mutually beneficial ways. They also learn to change destructive daily activity patterns. Interpersonal therapy also can be employed to manage more serious conflicts with others.

7. Occurrence
It is difficult to determine the exact numbers of people affected by depression. Based on existing evidence, experts currently believe that about 6% percent of the general population has persistent depressive disorder. Of patients seeking help for depression, 36% have a diagnosis of PDD, and 25% will probably go on to experience severe depression sometime in their lives.
During childbearing years, women are more susceptible than men are to dysthymia; pre-pubescent and post-menopausal women are affected equally. Men, however, are more likely to die because of the condition. PDD appears to run in families because patients are likely to be related to other individuals with some type of depression. One study also found African Americans and Mexican Americans more likely to develop dysthymia than Caucasians.

8. Childhood Dysthymia
It was once believed that children were not mature enough to experience clinical depression. However, scientists now know that 1% of children aged 3 to 4, 2% of those aged 5 to 12, and 5 to 8% of older children do experience depression of some kind. Of those with dysthymic disorder, one study showed that 76% went on to become severely depressed and that 13% developed bipolar disorder within 12 years.
Children are susceptible to all the same symptoms of PDD as adults, but they often will manifest in slightly different ways. For example, the most common sign of depression in children is extreme irritability. Because volatile moods and defiance of authority are normal parts of adolescent behavior, caregivers can sometimes be oblivious to childhood depression. Parents who notice a bad mood lasting for over two weeks should enquire as to the child’s feelings and consider seeking help from a professional.

9. Causes
There is no one widely-accepted cause for persistent depressive disorder. There are, however, many associated factors. For example, people under stress that is either severe or chronic can experience a change in brain chemistry that affects the regulation of mood. Specifically, levels of the hormone cortisol increase in response to stress, and neurotransmitters like dopamine decrease. Corticosteroid medications can produce similar changes.
Some individuals, due to either heredity or habit, have poor strategies when it comes to dealing with problems. Those who tend to brood and over-think problems instead of employing creative problem solving are especially prone to DPP. Also at risk, are people with personality traits that are gloomy, pessimistic, or overly sensitive to criticism. Traumatic experiences become overwhelming for people with these characteristics, and they can easily fall into depression.

10. Suicide Risk
A person diagnosed with dysthymia is not necessarily suicidal. People can live for years with PDD without suicidal thoughts. However, the greater the length of time a person suffers from depression, the more likely it is that these thoughts will occur. Symptoms also tend to worsen over time.
A person with dysthymia is significantly more likely to take his or her own life than a person who does not suffer from any type of depression. While depression alone cannot explain suicidal behavior, depression combined with other mental conditions, especially manic episodes, does appear to put people at high risk. Those with the anxious subtype of dysthymia tend to make unsuccessful suicide attempts, often as a way of seeking help. Up to 15% have a drug dependence, which is also a contributing factor.