What Is Angina Pectoris?
For many people, chest pain is a frightening and persistent fact of life. Chest pain, also known as angina pectoris, may show up at times of stress or exertion, or even without any warning at all.
Angina pectoris can be a symptom of more serious problems, and you should visit your doctor if you’re experiencing pain, tightness, or discomfort in your chest. Angina is often unsettling to those who experience it, as well as to their family, friends, and coworkers. Learning all you can about the condition is an important step toward managing your symptoms and reassuring those who care about you.
1. What Is Angina Pectoris?
Angina pectoris, more commonly called angina, refers to chest pain that is caused by limited blood flow to the heart muscle. Angina can be a symptom of coronary artery disease, which needs medical attention. If you are experiencing persistent pressure or aching in the center of your chest, you should see your doctor.
Pain from angina can differ from person to person and is often confused with the discomfort or pain caused by other conditions. Indigestion and heartburn are among the most common conditions confused with angina, and some pain from angina can be mistaken for digestive distress.

2. What Are the Symptoms of Angina?
The most common symptom of angina is chest pain or discomfort. For some people, this discomfort may feel more like pressure than pain. Other symptoms can include shortness of breath, sweating, nausea, vomiting, and unusual paleness.
Sometimes the discomfort of angina is felt in the back, neck, shoulders, or jaw instead of the chest. This is a phenomenon called referred pain, in which discomfort is experienced in a part of the body other than its cause. Many people might not immediately associate referred pain in their back or jaw with a potential heart problem, so it’s important to be alert and informed about varying symptoms.
3. What Causes Angina Pectoris?
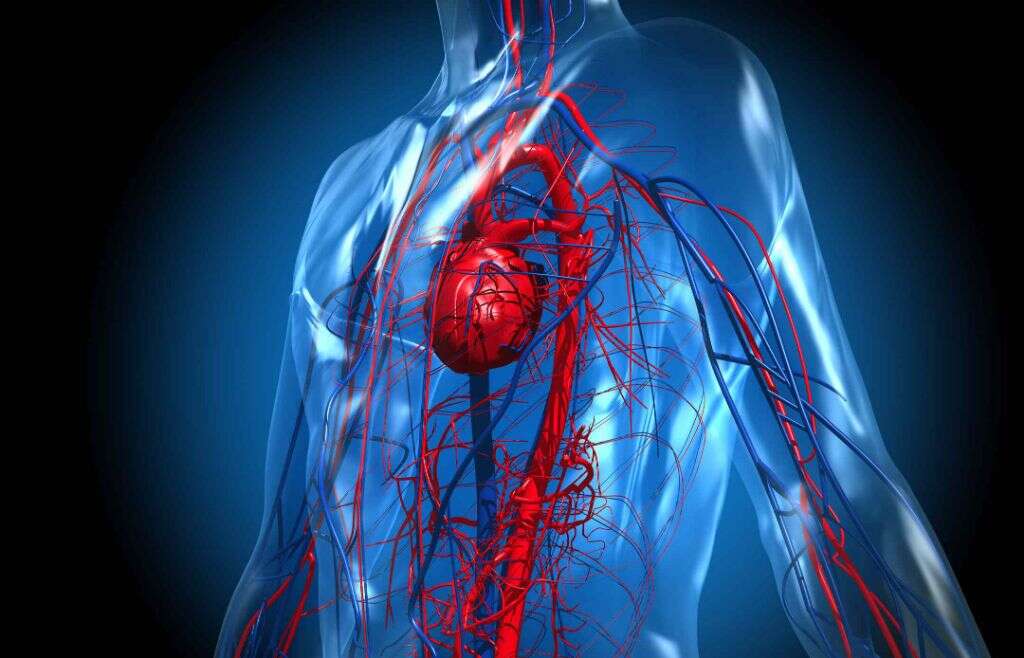
Angina is caused by restricted blood flow to the heart, usually as a result of an obstruction or spasm in the arteries that carry blood to the heart. Other causes can include anemia, abnormal heart rhythms, heart failure, and atherosclerosis caused by coronary artery disease.
One type of angina, called unstable angina, is more acute and often more dangerous than other types. Unstable angina is caused by fatty deposits or blood clots that suddenly become lodged in one or more arteries leading to the heart and requires urgent medical attention.
4. Stable Angina
Stable angina may be a prolonged or chronic condition and tends to develop after exercise or stress. If you have stable angina, it is generally predictable and similar to previous bouts of chest pain.
It is usually short-lived, frequently gone within five minutes, and may disappear even more quickly with use of medication. Stable angina requires a doctor’s care but can be manageable with medication and lifestyle changes.
5. Unstable Angina
Unstable angina is less common than stable angina and represents a medical emergency. Indications of unstable angina include changes in your regular pattern of angina, such as chest pain that is more severe or prolonged than usual and discomfort that may not improve or go away with medication.
Unstable angina can signal a heart attack and should be treated as quickly as possible.
6. Diagnosing Angina Pectoris
When you see your doctor about chest pain, he or she will talk to you about your symptoms, lifestyle, and family history. Your doctor may refer you for diagnostic tests, including blood tests and imaging. Doctors can use several tests to examine your heart and arteries to assess blood flow. Those tests might include an electrocardiogram, echocardiogram, stress test, X-ray, MRI, or others.
With treatment and lifestyle management, the prognosis for people with angina is often quite good. A 2007 study found that people with moderate to severe angina and an average age of 62 had a 5-year survival rate of 92%.1COURAGE Trial Research Group. ‘Optimal Medical Therapy with or without PCI for Stable Coronary Disease’. New England Journal of Medicine 356 (15), 2007.

7. Treating Angina Pectoris
When a patient is diagnosed with angina, a doctor will commonly prescribe medications that can help improve blood flow to the heart, like nitroglycerin and other nitrates. Other medications can treat the conditions that contribute to angina, like blood thinners to reduce clotting, beta-blockers to reduce blood pressure, or statins to improve cholesterol levels.
In some cases, your doctor might recommend a surgical procedure to help your angina. This might be a procedure like balloon angioplasty or insertion of a stent that widens the arteries. In more severe cases, coronary bypass surgery may be a better option. In coronary bypass surgery, surgeons use blood vessels taken from elsewhere in your body to create a new path for blood to flow to the heart, bypassing constricted arteries.

8. What Are the Risk Factors for Angina Pectoris?
Angina can affect anyone, but there are a number of risk factors that increase the possibility of developing the condition. These include smoking, diabetes, high cholesterol, high blood pressure, a sedentary lifestyle, and family history of heart disease. Age is also an important risk factor, with men over age 45 and women over age 55 being at highest risk.
There are also common factors that may precede a flare-up of angina, like physical activity, emotional stress, or eating a large meal. Some people are also more likely to experience angina in cold temperatures.
9. Angina and Women
Chest pain and heart conditions are often associated with men, but women can also develop angina. However, women’s experience of angina often differs from that of men. Women are more likely to have atypical, less severe, or absent symptoms, which can make angina in women harder to diagnose.
Angina symptoms in women may look identical to those in men but may also include anxiety, heart palpitations, weakness, and fatigue. When women do experience chest pain, they are more likely than men to describe it as a stabbing pain instead of pressure.

10. How Can I Reduce My Risk for Angina?
It is impossible to completely prevent the development of angina, and some risk factors, like your family health history, are out of your control. However, there are some important steps you can take to reduce your risk of developing angina.
Managing your stress and quitting smoking are great first steps to limiting your angina risk. You should also increase exercise, maintain a healthy diet, and get regular physicals to screen for elevated cholesterol and blood pressure or warning signs of diabetes. If you develop chest pain, unexplained pain elsewhere in your upper body, or unusual digestive symptoms, seeing your doctor promptly can help diagnose and potentially reduce the severity of angina.












