What Is a Myelopathy?
A group of nerves running inside the spine along nearly its entire length make up the spinal cord. As a part of the central nervous system, the spine has a crucial role to play in relaying messages from the brain to the rest of the body. Compression of the spinal cord can damage it. The resulting symptoms are known collectively as myelopathy.
Myelopathy is sometimes confused with other conditions. For example, radiculopathy can cause similar symptoms. However, while myelopathy results from compression of the spinal cord itself, radiculopathy is caused by compression of the nerve roots that extend out from it. Because of the similar-sounding names, people may also confuse myopathy with myelopathy. However, myopathy is a completely unrelated muscular disorder.

1. Types
The spine has three levels. The cervical spine is located in the neck, the lumbar spine is located in the lower back, and the thoracic spine is the level between them in the area of the trunk. The level where the cord compression occurs determines the type of myelopathy.
Myelopathy can also be chronic or acute in nature. Chronic myelopathy develops over time, usually due to degenerative processes associated with aging. Acute myelopathy occurs suddenly.

2. Prevalence
Some types of myelopathy are more common than others. Because the spinal cord ends in the top section of the lumbar spine in most people, lumbar myelopathy is extremely rare. The most common type of myelopathy is cervical myelopathy, followed by thoracic myelopathy.
Cervical myelopathy is usually degenerative, and this variety affects an estimated 41 to 605 million people in North America. People over the age of 50 are most likely to experience myelopathy, particularly if it is degenerative.

3. Causes
Acute myelopathy may occur due to an injury or an infection. Sudden trauma to the bones of the spine can cause compression fractures of the vertebrae or bone fragments that put pressure on the spinal cord. An infection can cause swelling of the tissues surrounding the spinal cord, putting pressure on it by narrowing the space the cord has within the spine, which is called the spinal foramen.
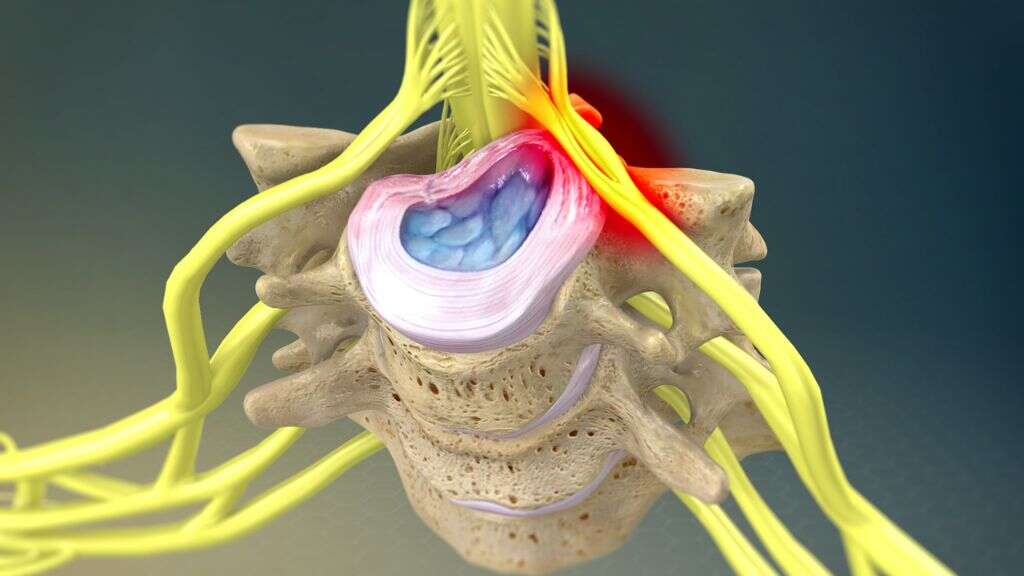
Chronic myelopathy may occur due to spinal stenosis, which is a narrowing of the spinal foramen over time. The most common causes of spinal foraminal stenosis include disk herniation and osteophyte formation. Disks are tough but flexible structures between the vertebrae, and herniation occurs when damage to the hard, outer layer allows the soft inner layer to leak out. Osteophytes are also called bone spurs and occur when the bones rub together because there is not enough cushioning between the vertebrae.
4. Symptoms
The symptoms of myelopathy may vary depending on the level where the compression occurs. You may experience pain in your back or your neck. You may also experience symptoms of weakness, numbness, and tingling in your arms or legs. Cervical myelopathy is more likely to cause symptoms in your arms, while lower extremity symptoms may result from compression at a lower level.
Because compression of the spinal cord can disrupt the neural signals from your brain, myelopathy can also cause deficits in both voluntary and involuntary functions. For example, you may experience difficulty walking, problems with fine motor skills, and issues with coordination and balance. Reflexes may become abnormal or increased, while bowel and bladder control may decrease.

5. Risk Factors
Certain underlying medical conditions can cause or contribute to myelopathy. For example, rheumatoid arthritis can cause spinal cord compression by attacking the tissues of the intervertebral joints. Diabetes can also contribute to myelopathy, and tumors can put pressure on the spinal cord.
Because myelopathy is often chronic in nature, your risk of developing it increases as you get older. Aging also contributes to other degenerative conditions that can cause myelopathy, such as arthritis. This causes decreased joint space between the vertebrae, which can lead to osteophyte formation.
6. Diagnosis
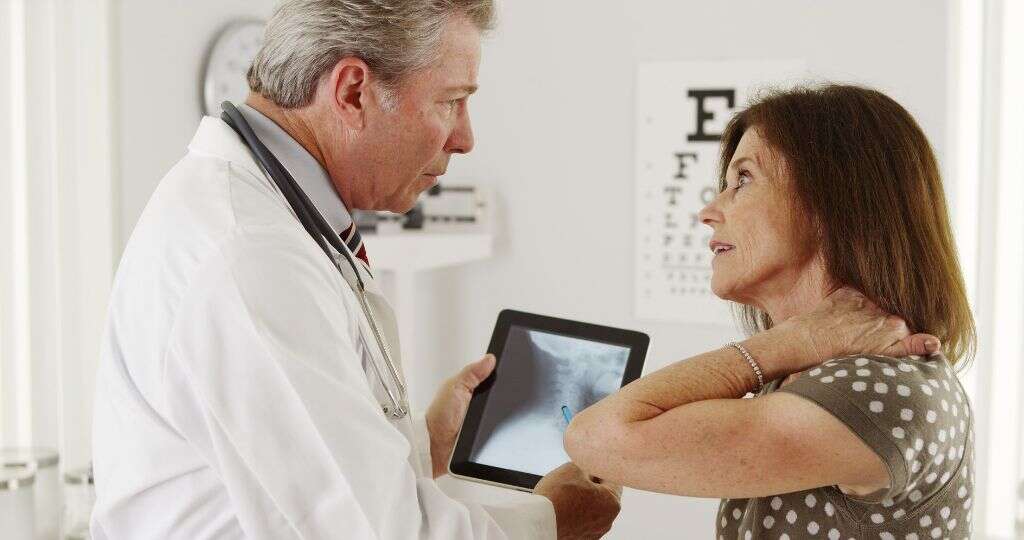
Your doctor may give you tests to measure the nerve function in your arms and legs. This provides an idea of how well the signals are communicating between your brain and your extremities. An MRI scan allows the doctor to observe the soft tissues of the spinal cord. This has become a vital tool in diagnosing myelopathy, but not everyone is able to have it.
If you cannot have an MRI, your doctor may conduct myelography instead. This can reveal spinal cord abnormalities by injecting a contrast medium and taking a scan using fluoroscopy, which is a special X-ray that allows the doctor to see images in real time. Plain film X-rays and CT exams may be useful in identifying osteophytes or other bone abnormalities. Your doctor will also conduct a physical examination and ask you questions about your symptoms.

7. Treatment
Your doctor may recommend nonsurgical treatments for your myelopathy at first. These may include medications to relieve the pain and reduce inflammation that may be contributing to your symptoms. Physical therapy may help to relieve the pain and symptoms by addressing the direct cause of myelopathy, prescribing specific stretching and strengthening activities, and treating how a person tends to move. Bracing is another treatment option.
If conservative treatments such as these are unsuccessful or your myelopathy is advanced, your doctor may recommend surgery to relieve the compression. Spinal fusion may be performed with decompression to reduce the motion of the affected vertebrae. Laminoplasty is performed to increase the space within the channel and relieve the compression on the cord.

8. Complications
Myelopathy isn’t a disease per se but a collection of symptoms. Therefore, it can’t really be said to cause complications, although it may be a complication of another condition. However, myelopathy treatments, particularly surgery, can have complications.
Risks of spine surgery include tearing of the sac of protective tissue surrounding the spinal cord, injury to the nerves, and infection. The less invasive the spinal procedure, the lower the risk of complications. While a spinal-fusion surgery may result in reduced flexibility, laminoplasty may retain your ability to move.

9. Management
It may be possible to recover completely from myelopathy depending on the underlying cause. For example, a course of antibiotics may be successful at resolving an underlying infection. Most patients report considerable improvement from laminoplasty or spinal fusion.
Depending on the extent of the damage, it may not be possible to resolve the symptoms of myelopathy entirely. However, it may be possible to manage symptoms with medications, hot and cold treatment, exercise, and lifestyle changes.

10. Prognosis
Sometimes decompressing the spinal cord is sufficient to relieve myelopathy symptoms. It is important to receive diagnosis and treatment early to prevent the damage from progressing. This offers a better chance of full resolution.
If the damage to the spinal cord is extensive and permanent, it may not be possible to reverse the symptoms of myelopathy. In that case, the best you can hope for is to manage the symptoms and keep them from progressing further.