Otosclerosis Symptoms, Treatments & More
 Article Sources
Article Sources
- 1. 'Otosclerosis.' National Institute of Deafness and Other Communication Disorders, U.S. Department of Health and Human Services, 14 Dec. 2020, www.nidcd.nih.gov/health/otosclerosis.
- 2. NHS Choices, NHS, www.nhs.uk/conditions/otosclerosis/.
- 3. BritishTinnitus. 'Otosclerosis and Deafness.' British Tinnitus Association, www.tinnitus.org.uk/otosclerosis.
- 4. NHS Choices, NHS, www.nhs.uk/conditions/tinnitus/.
Bone tissues regrowing and replacing themselves are a natural part of life. But when this process, called bone remodeling, happens abnormally, it can damage delicate structures in the body.
Otosclerosis is when abnormal bone remodeling makes it difficult for sound to travel from the middle ear to the inner ear. Over three million people in the United States are affected by otosclerosis, which can cause partial deafness, tinnitus and problems with balance. Treatments are available, but each type of treatment comes with its own risks. Understanding the condition and possible treatments can help those living with otosclerosis choose the best options for them.1‘Otosclerosis.’ National Institute of Deafness and Other Communication Disorders, U.S. Department of Health and Human Services, 14 Dec. 2020, www.nidcd.nih.gov/health/otosclerosis.

1. Symptoms of Otosclerosis
The most noticeable and most common symptom of otosclerosis is difficulty hearing which gradually progresses for months or years. Hearing loss starts in one ear and then affects both ears. It’s rare for a person with otosclerosis to become completely deaf, but they may not be able to hear deep or quiet sounds. A person with otosclerosis may speak quietly because their voice sounds abnormally loud to them. They may hear more easily with background noise, something that is not as common for other deaf or hard of hearing people.2NHS Choices, NHS, www.nhs.uk/conditions/otosclerosis/.
Some people with otosclerosis report dizziness and issues with balance. Tinnitus, a persistent roaring, buzzing or hissing sound in the ears, is another possible symptom.1‘Otosclerosis.’ National Institute of Deafness and Other Communication Disorders, U.S. Department of Health and Human Services, 14 Dec. 2020, www.nidcd.nih.gov/health/otosclerosis.

2. Causes of Otosclerosis
There is a lot about the inner ear that science doesn’t yet know. It’s known that abnormal bone remodeling causes otosclerosis, but what causes the bones to reform abnormally in the first place is unclear.
It does tend to run in families, suggesting a genetic cause. People who are pregnant and have otosclerosis tend to report worsening symptoms, meaning hormones could also play a factor.2NHS Choices, NHS, www.nhs.uk/conditions/otosclerosis/. Other possible causes include autoimmune disease or even past measles infections or injuries to the inner ear.3BritishTinnitus. ‘Otosclerosis and Deafness.’ British Tinnitus Association, www.tinnitus.org.uk/otosclerosis.

3. Who Is At Risk?
There is no known way to prevent otosclerosis and it could potentially happen in anyone, though white, middle-aged women are the group most likely to be diagnosed.1‘Otosclerosis.’ National Institute of Deafness and Other Communication Disorders, U.S. Department of Health and Human Services, 14 Dec. 2020, www.nidcd.nih.gov/health/otosclerosis.
It’s believed that otosclerosis can be inherited, so those with a family history of the condition have a higher risk. People with otosclerosis are most likely to first notice changes in their hearing in their 20s and 30s. If a person is concerned about symptoms that could suggest otosclerosis, it is recommended to see a doctor.2NHS Choices, NHS, www.nhs.uk/conditions/otosclerosis/.

4. Diagnosing Otosclerosis
The symptoms of otosclerosis can be similar to many other conditions that affect the inner ear. A specialist in conditions of the ear, like an audiologist or an ENT, is usually the person to diagnose otosclerosis.
A person with suspected otosclerosis will likely be asked questions about their symptoms and medical history. The specialist will attempt to rule out other diseases or health problems. Hearing tests like an audiogram or tympanogram will often be recommended. Sometimes otosclerosis will be confirmed with a CT scan.1‘Otosclerosis.’ National Institute of Deafness and Other Communication Disorders, U.S. Department of Health and Human Services, 14 Dec. 2020, www.nidcd.nih.gov/health/otosclerosis.

5. Hearing Aids and Otosclerosis
In mild cases of otosclerosis, treatment may not be necessary. The doctor and patient can decide together what level of treatment is appropriate.
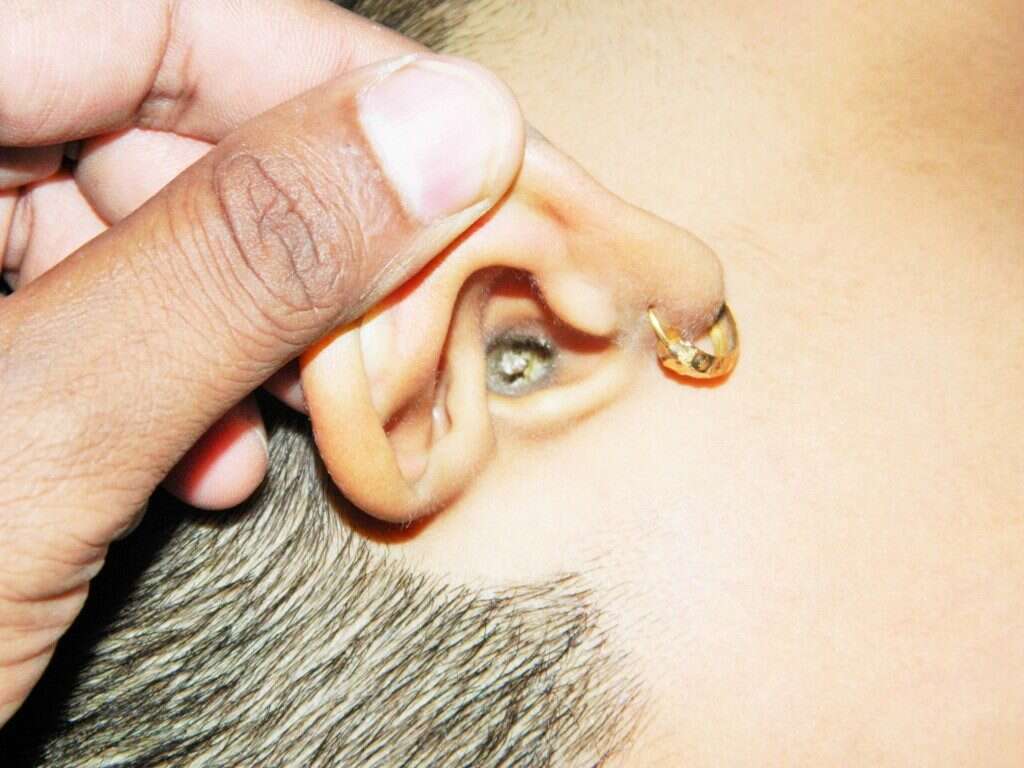
Hearing aids are a commonly recommended treatment for otosclerosis symptoms. A hearing aid is a small, discrete device that can be worn inside or just outside the ear to amplify sound. Many people with otosclerosis see an immediate improvement in their symptoms when using hearing aids, which are far less invasive than surgery.2NHS Choices, NHS, www.nhs.uk/conditions/otosclerosis/.

6. Surgery and Otosclerosis
If a person can’t or doesn’t want to use hearing aids or is worried about the otosclerosis progressing, surgery is another option. A stapedectomy involves removing some of the bone and placing an implant that allows sound to travel through the remaining bone and into the inner ear.
The surgery is usually successful, and can allow those with otosclerosis to hear without the use of a hearing aid and can sometimes keep otosclerosis from getting worse.2NHS Choices, NHS, www.nhs.uk/conditions/otosclerosis/.

7. Recovery and Risks of a Stapedectomy
People who get a stapedectomy for otosclerosis can in most cases go home within a day or two. A few weeks of rest are usually needed and patients notice improvements in a few weeks with minimal scarring.3BritishTinnitus. ‘Otosclerosis and Deafness.’ British Tinnitus Association, www.tinnitus.org.uk/otosclerosis.
But in about 1% of cases, the surgery actually worsens symptoms and patients can become completely deaf in that ear. While the surgery usually improves tinnitus, it can sometimes cause new or stronger tinnitus. Temporary vertigo and altered sense of taste are also reported.2NHS Choices, NHS, www.nhs.uk/conditions/otosclerosis/.

8. Risks of a Second Ear Surgery
Some people who have had a successful stapedectomy in one ear may wish to have the procedure done on their other ear. Some specialists recommend against this. In very rare cases, complete deafness can occur years after in an ear that has had a stapedectomy, and leaving one ear intact can allow the person to use hearing aids if this happens.
People who are concerned about the potential risks should talk to their specialist. An experienced surgeon can help people make these decisions.3BritishTinnitus. ‘Otosclerosis and Deafness.’ British Tinnitus Association, www.tinnitus.org.uk/otosclerosis.

9. Living With Tinnitus
Tinnitus can be one of the most challenging symptoms of otosclerosis. While not all people with otosclerosis have buzzing or ringing in their ears, those that do can experience disorientation, anxiety and depression. Treatments for otosclerosis often improve tinnitus, but there’s no guarantee that it can be resolved.
Soft music or sounds in the background can help ease tinnitus as can yoga and relaxation exercises. Support groups and self-help resources from trusted organizations can also help a person with tinnitus feel less isolated.4NHS Choices, NHS, www.nhs.uk/conditions/tinnitus/.

10. Later Life with Otosclerosis
It’s common for people to become hard of hearing as they get older and people with otosclerosis aren’t different from anyone else in this regard. Even those who have had a successful stapedectomy may need to use a hearing aid later in life.3BritishTinnitus. ‘Otosclerosis and Deafness.’ British Tinnitus Association, www.tinnitus.org.uk/otosclerosis.
If a person opts to use hearing aids to treat their otosclerosis symptoms, they can simply adjust the hearing aids to match their needs as they get older. Otosclerosis is not often associated with particular problems in old age.2NHS Choices, NHS, www.nhs.uk/conditions/otosclerosis/.