Collapsed Lung Symptoms
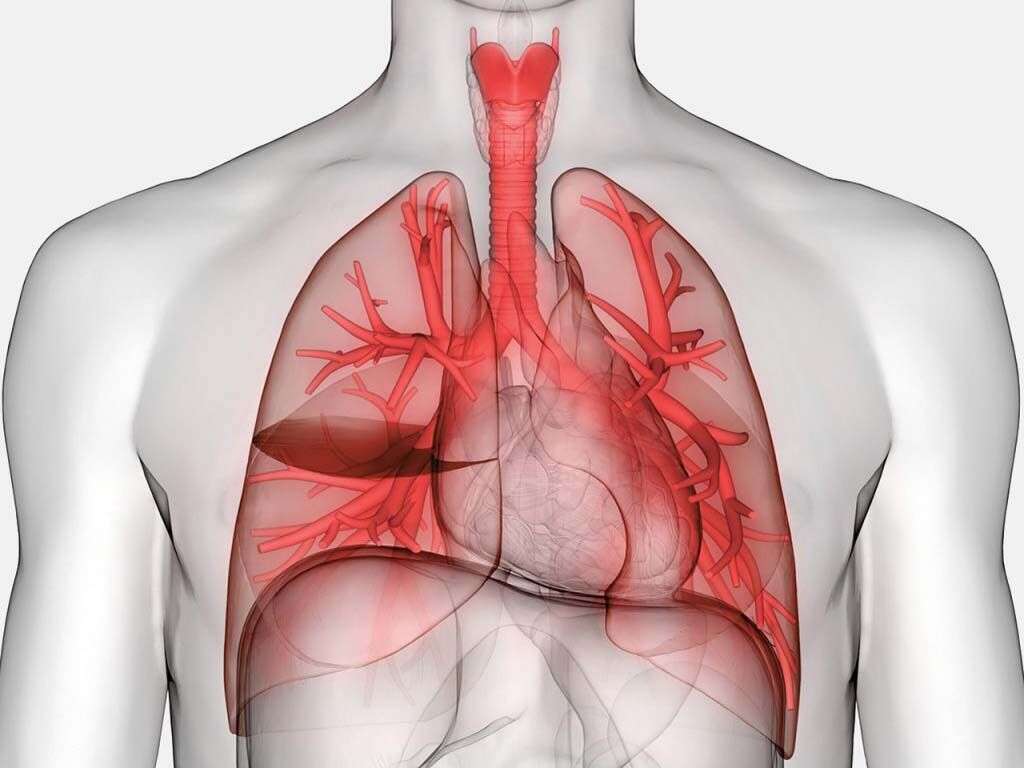
Collapsed lung, also called pneumothorax, occurs when air fills the pleural space that surrounds the lungs. The condition can arise if the chest wall is injured, opened, or if any tear or rupture happens in the pulmonary tissue. When air gets into the pleural space, it causes disruption of the intrathoracic pressure, which is responsible for keeping the lungs inflated.
When air enters the pleural space, it increases pressure internally, which deflates the lungs, besides other complications including pressure on the heart. If the amount of air is small, the condition is called spontaneous pneumothorax, which can heal without treatment. However, if the amount of air is huge, the resultant condition can be life-threatening. Possible causes of collapsed lungs include pulmonary diseases, accidents, violent sports, atmospheric pressure changes when you climb a mountain or go diving, and breathing via a ventilator. Following are 10 collapsed lung symptoms.

1. Sudden Chest Pain
Sudden, acute chest pain is one of the most serious symptoms of ill health, and is usually associated with cardiac problems, heartburn, angina, and other chest problems.
However, sudden chest pain is also the main symptom of collapsed lungs. Patients describe it as squeezing or crushing pain. When the pain is a result of pneumothorax, it is usually accompanied by other symptoms, in addition to an apparent cause of the collapse.

2. Shortness of Breath
Dyspnea, or shortness of breath, is one of the most difficult sensations you can experience. Imagine not being able to get enough air, it is terrifying. Patients describe shortness of breath as a tightening sensation over the chest, hunger for air, and difficulty in breathing. In severe cases, it feels like suffocation.
It is a common chest symptom that can result from different conditions such as extreme exercise, obesity, mountain climbing, and extreme cold or hot weather. These causes are natural and do not require medical help. However, if shortness of breath is accompanied by other symptoms or an underlying cause, seek medical help as soon as possible.

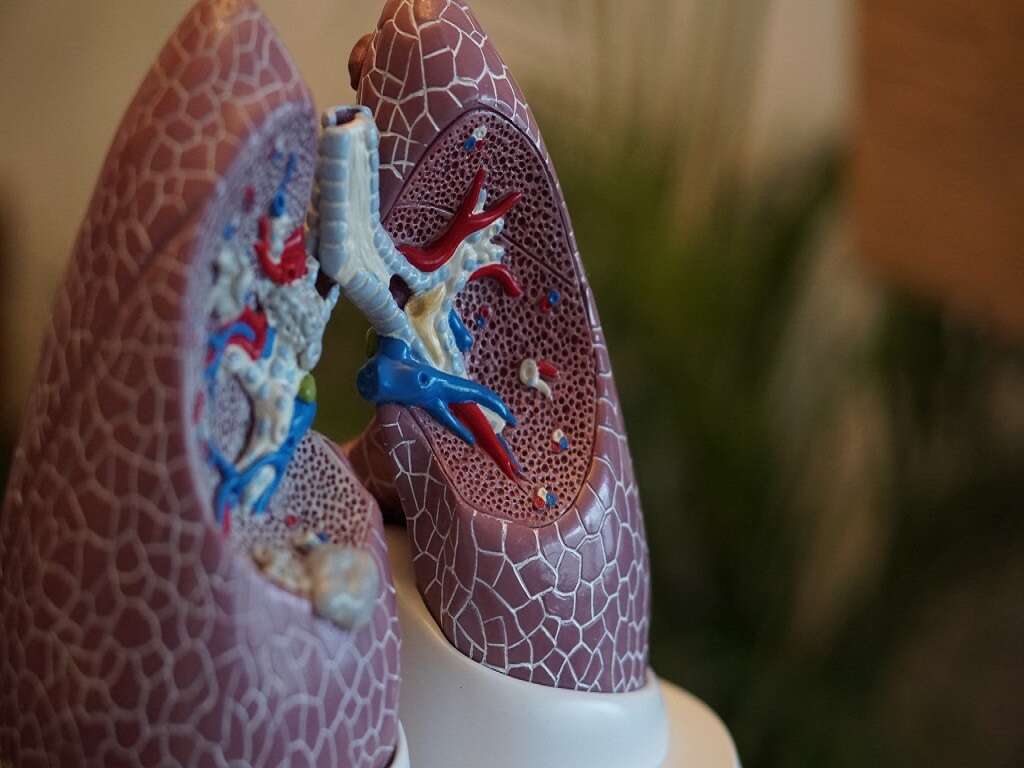
3. Low Oxygen Levels in Blood
Low blood levels of oxygen, or hypoxemia, is a condition in which blood in the arteries does not contain enough oxygen to supply to the tissues. This occurs because the collapsed lung has reduced capacity for air exchange.
If hypoxemia progresses, it can lead to major complications such as breathlessness, increased rate of breathing, and cyanosis. If the level of oxygen in blood becomes lower than 60 mmHg, the condition is severe and must be treated as soon as possible.

4. Discoloration of Fingers and Lips
Also called cyanosis, discoloration of tissues occurs due to low oxygen level in tissues. It is most noticeable on the skin and mucous membranes on the surface. These parts of the body appear bluish or purple. While cyanosis may also have other causes, it is an important collapsed lung symptom.
Once the first signs of cyanosis appear on fingers and lips, it is a sign that immediate intervention is required. Note that severe cyanosis can indicate severe circulatory failure that can be fatal.

5. High Carbon Dioxide Levels in Blood
A collapsed lung can lead to increased carbon dioxide in blood, also called hypercapnia. This occurs because the air surrounding the lungs and filling the pleural space prevents the lungs from expelling as much carbon dioxide as they normally would.
Hypercapnia leads to respiratory acidosis, which the kidneys try to balance by retaining alkali materials instead of expelling it in urine. If the pneumothorax is severe, it can lead to acute hypercapnia, which is a medical emergency. Chronic hypercapnia can be associated with scuba diving and mountain climbing.

6. Mental Confusion
Mental confusion can occur due to the reduced oxygen supply to the brain, and the accumulation of carbon dioxide in the blood. Respiratory acidosis that results from hypercapnia affects the brain and leads to this unclear state of mind.
If the condition persists, it may progress to serious complications such as delirium, hallucinations, convulsions, and coma. If the condition is left untreated, it can be fatal.

7. Rib Fractures
Traumatic pneumothorax is one type of pneumothorax. It can result from either blunt trauma or penetrating injury to the chest wall. It is usually associated with rib fractures.
The pain becomes more severe when the patient breathes in, and bruising may be observed at the site of the trauma. The fracture may affect one or more ribs. Pneumothorax is the direct result of rib fractures because the ribs cause injuries to the pleural space.

8. Changes in Breathing Sounds
There is asymmetric lung expansion in most cases of pneumothorax. It is also common to have diminished or distant-sounding breath sounds on the affected side.
This occurs due to the decreased air entry to the lung. When the doctor listens to the sounds, the difference in breathing sounds will usually be apparent. Wheezes and crackles may also be present.

9. Increased Heart Rate
Increased heartbeat, or tachycardia, is the most common cardiac symptom of pneumothorax. In some cases, the heart rate may reach 135 beats per minute. Low blood pressure or hypotension is another sign of pneumothorax.
It is a late finding, but is important to correct, especially before surgical intervention. High pressure in the jugular vein, a common occurrence in tension pneumothorax, should be differentiated from severe hypotension during treatment.

10. Respiratory Distress
Acute respiratory distress syndrome (ARDS) in cases of pneumothorax usually happens in traumatic pneumothorax. It is a severe medical emergency that requires immediate intervention. The condition occurs when fluid fills the lung, lowering the oxygen level in blood, and increasing the level of carbon dioxide.
ARDS can lead to organ failure if the tissues continue working without enough oxygen. Extreme shortness of breath and gasping for air are the most common symptoms of ARDS, which is life-threatening.