All About Ovulation Pain
Ovulation pain is also often referred to as midcycle pain or mittelschmerz. The term mittelschmerz originated from a German word that translates to “middle pain.” Ovulation pain has been estimated to occur in about 20% of women with some experiencing it intermittently while others have it every cycle.
Ovulation pain is not an infrequent complaint. Since it occurs due to ovulation, the pain is usually present in the midmenstrual cycle. In most cases, it does not require medical attention. It is often managed symptomatically with pain relievers and home remedies.
1. Symptoms
The pain that women with ovulation pain generally experience is located in the pelvis or lower abdomen. It usually occurs about halfway through the menstrual cycle (around 14 days from the first day of menstruation). This pain can begin suddenly and resolve on its own within hours. For some women, it may last several days or even up till the next cycle. Some women can even tell if the right or left ovary is providing the egg as the pain will be localized on that side. Since ovulation occurs on a random ovary, but normally alternates, the pain may occur on either the left or right side. Other associated symptoms that women may experience would be the appearance of cervical mucus, mid-cycle bleeding, swelling of the vulva before ovulation, and swelling or tenderness of a lymph node in the groin.
2. The Menstrual Cycle
The menstrual cycle is the cyclical change occurring in the female reproductive tract that allows pregnancy to be possible. This cycle is necessary for the production of the oocyte (egg) and to prepare the body for pregnancy. The length of the menstrual cycle varies for each woman.
Those with less than 8 days difference between their longest and shortest cycle are considered to have a regular cycle. A difference of 8 to 20 days is considered to be moderately irregular while a variation of more than 21 days is considered to be very irregular. An average menstrual cycle lasts 28 days. The menstrual cycle can be described by the ovarian cycle and uterine cycle.
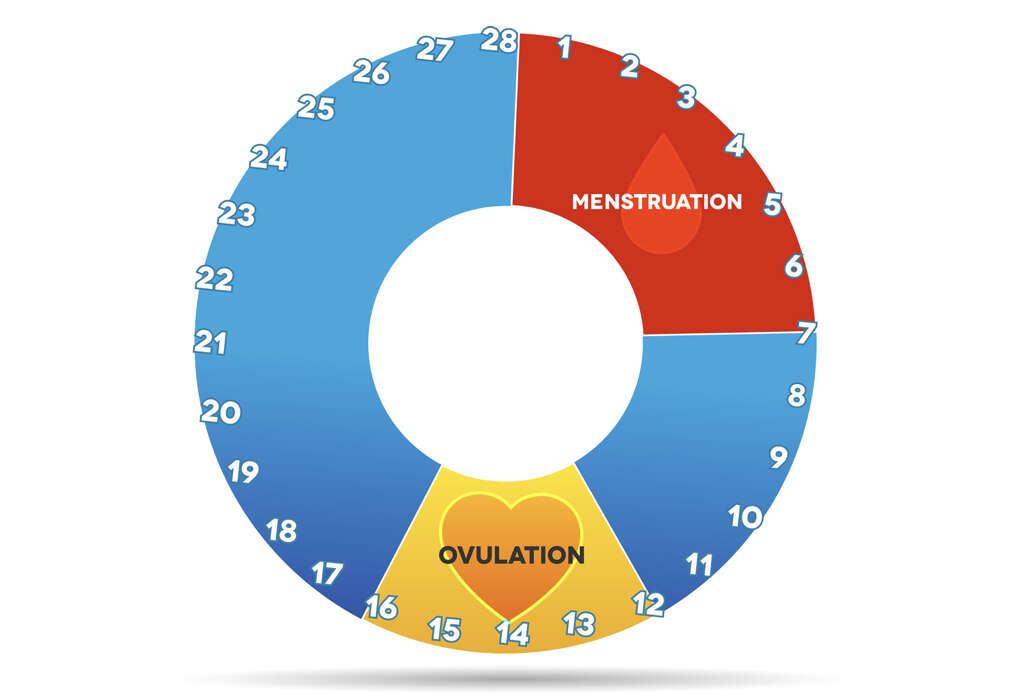
3. The Ovarian Cycle
The ovarian cycle describes the changes in the ovary throughout the menstrual cycle. It can be divided into the follicular, ovulation, and luteal phase. In the follicular phase, the follicle stimulating hormone (FSH) stimulates the development of several follicles.
These follicles are already present in the ovary during birth (in females). One follicle will mature fully (tertiary or Graafian follicle) and contains the ovum. In the ovulation phase, the luteinizing hormone (LH) level peaks. The LH helps the egg mature and weakens the walls of the Graafian follicle, allowing it to rupture and release the egg. After the egg is released, the luteal phase begins. This is where the FSH and LH functions to transform the remaining follicle to become the corpus luteum. The corpus luteum is important as it produces progesterone.
4. The Uterine Cycle
The uterine cycle reflects the changes in the uterus during the menstrual cycle. It can be divided into the menstruation, proliferative, and secretory phases. In the menstruation phase, the uterine lining sloughs off and is shed, resulting in menstrual bleeding. The flow of menses signifies that the woman is not pregnant. In the proliferative phase, the rising levels of estrogen causes the uterine lining to proliferate.
It also stimulates the formation of crypts in the cervix to produce cervical mucus (to help sperm swim up to the egg). When this cervical mucus is present, the woman is fertile. The secretory phase corresponds to the last phase in the ovarian cycle, the luteal phase. The progesterone produced by the corpus luteum makes the uterus receptive to the implantation of the fertilized egg. It is known as the secretory phase as there are increased uterine secretions and blood flow.

5. What Causes Mittelschmerz?
The exact cause of ovulation pain is unclear. However, several theories have been proposed by various experts over the years. The first one would be that the pain occurs due to the stretching of the ovary before ovulation occurs, causing pain. This theory helps explain ovulation pain that occurs on both sides of the abdomen.
Other experts have also suggested that when ovulation occurs, the release of the egg also results in the release of blood or fluid into the abdomen, causing irritation to the abdominal lining resulting in pain. The rupture of the ovary to release the egg itself can also be the cause of the pain. Another theory is that ovulation causes the tubes and uterus to contract due to the increased prostaglandin levels, resulting in pain.
6. Diagnosis
The diagnosis of ovulation pain can be made if the pain occurs during the woman’s mid-menstrual cycle and the pelvic examination does not show any abnormalities. During a pelvic exam, an external exam will look at the vulva vagina for any abnormalities. A speculum is then inserted into the vagina to examine the internal reproductive organs (uterus, fallopian tubes, ovaries, cervix, vagina). Samples are collected from the cervix for further examination.
A bimanual exam (two gloved and lubricated fingers are inserted into the vagina to check the uterus and ovaries) and rectovaginal (gloved finger inserted into rectum to check for anomalies) exam can also be performed. Other diagnostic procedures such as an ultrasound of the abdomen can also be performed to rule out other issues. Cervical cultures and blood tests may also be beneficial.

7. Treatment
In ovulation pain, most patients do not usually require any treatment. The pain is usually not debilitating and does not signify the presence of underlying disease. For those who have prolonged or more intense pain, pain relievers such as paracetamol (acetaminophen) or nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen, naproxen sodium, and diclofenac sodium can be used. NSAIDs are particularly useful at blocking the effects of prostaglandins.
Keep in mind that pain relievers can be harsh on the stomach, especially for those with reflux or ulcers. It is best to take the pain relievers with meals and to consult your doctor before using them. The use of hormonal forms of contraception can also be beneficial as it prevents ovulation and, in turn, stops ovulation pain from happening.
8. Self-Care
Some nutritionists and fitness experts recommend the consumption of dark leafy greens as they contain high amounts of magnesium and calcium that can help reduce bloating and constipation during ovulation. Avoidance of processed foods can also worsen ovulation symptoms as it can cause more bloating and cramps. Having a regular exercise routine is always good.
The stretching of muscles and release of powerful endorphins can help with ovulation pain. Adequate hydration may increase blood flow to muscles and alleviate bloating or cramping. Taking a warm shower or bath also helps both the body and mind to relax. Ensure that you get enough rest every day (at least 7 hours a day for adult women). Try to avoid alcohol as it dehydrates the body and has the potential to intensify the symptoms of ovulation pain.

9. Foods and Supplements
The consumption of papaya may be beneficial as it contains the enzyme papain, which can help alleviate the discomfort associated with ovulation. Studies have also shown that taking vitamin D supplements can help reduce the severity of cramps during ovulation. Omega-3 fatty acids may also help as it can reduce inflammation.
Some women have found that drinking a cup of chamomile tea helps them relax, An average cup of chamomile tea also boosts the levels of an amino acid known as glycine. This helps contracting muscles to relax and can be greatly beneficial for those who experience cramps during ovulation.
10. Should I Worry about Ovulation Pain?
Ovulation pain is relatively common and is usually harmless. In some cases, especially those with severe and prolonged ovulation pain, it can be a symptom of an underlying medical issue. For example, the affected woman may have endometriosis, which is an inflammatory condition that can cause pain during ovulation. Endometriosis can affect the ovaries and fallopian tubes.
For those who have had previous surgery, such as the removal of the appendix or a caesarean section for the birth of a child, the presence of scar tissue can restrict the ovaries and the surrounding structures, resulting in ovulation pain. Ovulation pain may also occur due to the presence of sexually transmitted infections such as chlamydia as it causes scarring and inflammation around the ovaries and tubes. Other possibilities include an ovarian cyst, salpingitis, and appendicitis.