What Is Trench Mouth?
Gingivitis is a common gum condition that causes bleeding, irritation, and possibly tooth loss. Trench mouth is a more rare and advanced form of gingivitis. The symptoms can be similar but are often much more severe.
Trench mouth is known more scientifically as necrotizing ulcerative gingivitis or necrotizing ulcerative periodontitis. It is a severe form of gum disease that can eat away at the gums, eventually leading to soft tissue death. Fortunately, NUG is relatively uncommon, and not contagious. The condition is treatable, and many patients eventually make a full recovery.

1. History
The name “trench mouth” dates back to World War I. Among soldiers fighting in the trenches in Europe, oral hygiene was difficult to maintain. In the absence of regular brushing and flossing, the bacteria normally present in the mouth overgrew, causing serious infection of the gums.
However, the condition existed long before World War I. It was first identified in the fourth century B.C. Prior to World War I, it was more commonly known as Vincent stomatitis or Vincent angina, named after a 19th-century French doctor who discovered the bacteria that cause it.

2. Prevalence
Trench mouth is currently most prevalent in developing countries with poor access to dental care where oral hygiene may not be practiced regularly. In the United States, it is very rare, found in 1% or less of the population.
Trench mouth’s relative rarity may be due in part to the fact that it is noncommunicable. This means that it does not spread from person to person. Nevertheless, NUG is more likely to develop among certain segments of the population. Soldiers are still a vulnerable group, as are people with underlying medical conditions that compromise the immune system.

3. Symptoms
Like gingivitis, trench mouth can cause symptoms of gum irritation, swelling, bleeding, and bad breath. These symptoms may be much more severe with a case of NUG. Unlike gingivitis, trench mouth often causes pain, which can come on suddenly and is often severe. Because it is caused by a bacterial infection, NUG may produce systemic symptoms, such as fever or fatigue.
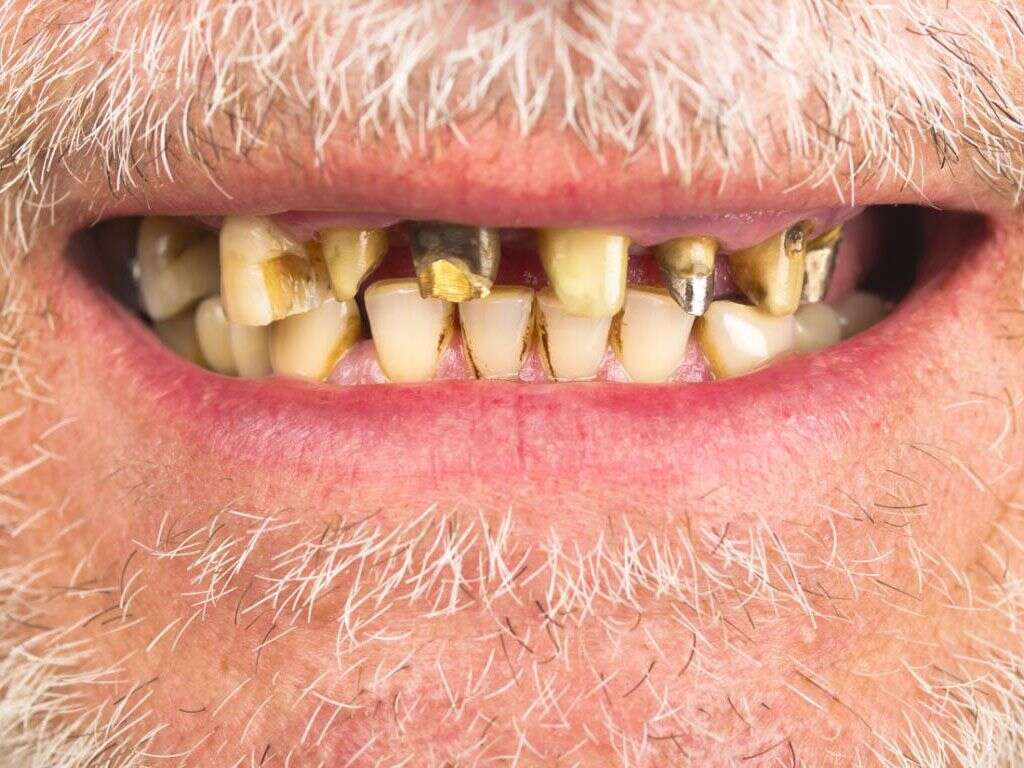
Between the teeth, there are small projections of skin called papillae. Trench mouth can cause these to become ulcerated. This causes a depression in the skin, similar to a volcano crater. The ulcerated papillae may be covered with a gray or yellow-white membrane.

4. Causes
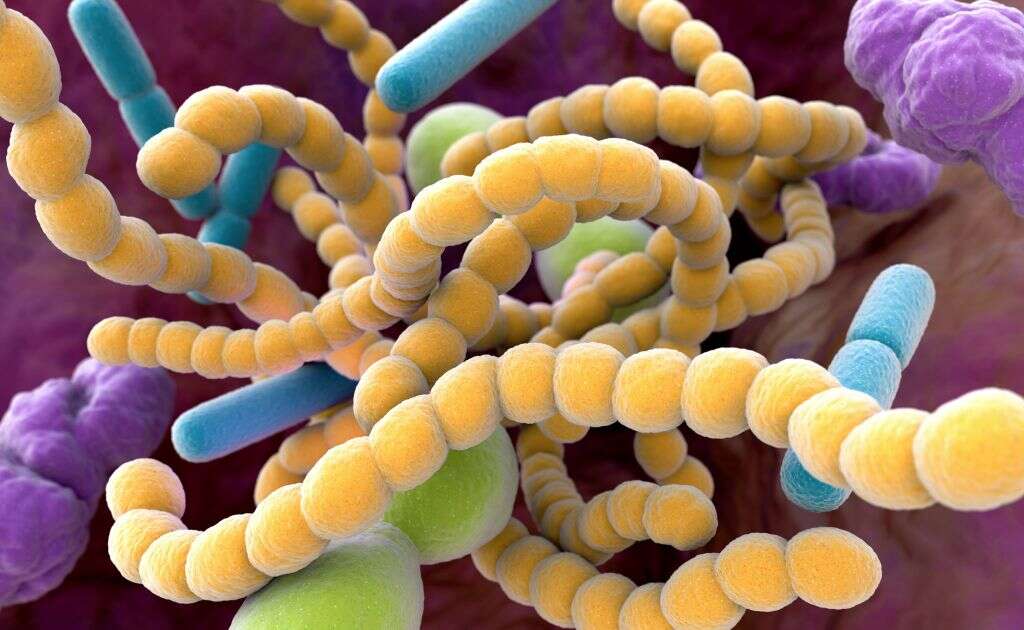
The human mouth normally contains many different species of bacteria. Usually, they exist harmlessly and do not cause any trouble. However, in the absence of oral hygiene to keep them in check, certain species of bacteria can become overgrown. When this occurs, they can cause an infection that results in trench mouth.
There are three species of bacteria that can contribute to trench mouth. Borrelia vincentii is a spirochete, which means that it has a coiled, spiral shape. Bacillus fusiformis is spindle-shaped, wide in the middle but tapering at either end. Prevotella intermedia is a rod-shaped bacterium that plays a role in other periodontal diseases besides trench mouth.
5. Risk Factors
Trench mouth most often affects young adults between the ages of 18 and 30. Men are more often affected than women. People who smoke or chew tobacco are much more likely to develop trench mouth than people who do not. Having gingivitis, or having had it in the past, puts a person at risk for developing trench mouth. People who do not brush or floss daily or do not see a dentist on a regular basis may be more susceptible to bacterial overgrowth and a resulting infection.
Trench mouth can also be a complication of an underlying medical condition. In healthy people, the immune system keeps oral bacteria in check. However, conditions that compromise or suppress the immune system, such as diabetes or HIV/AIDS, can allow the bacteria to proliferate.

6. Complications
Symptoms of trench mouth, such as pain and bad breath, can be severe enough to disrupt life activities. Patients may experience trouble swallowing as a result of the infection. This could make it difficult to receive proper nutrition. The destruction of the gum tissue, also known as necrosis, can lead to the loss of one’s teeth.
Trench mouth may spread to the jaw, leading to the development of other oral diseases that can cause damage to the bone. However, it is not always clear whether these conditions develop directly from NUG or a separate disease process.

7. Diagnosis
A dentist or doctor may suspect trench mouth on the basis of extremely bad breath. A physical examination to evaluate gum bleeding may confirm the diagnosis. An X-ray can indicate whether the infection has spread to the bone.
A provider may perform cultures of the mouth to check for bacteria. However, since the micro-organisms that cause NUG are typically present in a healthy mouth, this may not be a particularly useful diagnostic. Blood work may demonstrate an elevated white blood cell count, indicating infection, or help to identify a previously undiagnosed underlying condition that may be contributing to the condition of the gums.

8. Treatment
Initially, the goal of trench mouth treatment is to stop the disease progression and control the symptoms. Patients are advised to avoid eating foods that are spicy or hot during their recovery and to stop smoking. A doctor may prescribe painkillers or recommend over-the-counter pain relievers based on the severity of the patient’s discomfort.
Keeping the mouth clean is essential to stopping the progression of trench mouth. However, brushing may be too painful at first. Rinsing the mouth with equal parts hydrogen peroxide and water helps to remove dead tissue from the mouth in addition to helping to cleanse it and ease the symptoms. It may also be necessary to perform a debridement, i.e., surgical removal of the dead tissue.

9. Prevention
Oral hygiene is key to preventing both initial onset and recurrence of trench mouth. Patients should brush and floss at least twice a day, particularly after meals, and see a dentist on a regular basis for checkups and cleanings.
Generally speaking, a healthy lifestyle can help prevent trench mouth. This includes eating right, getting enough sleep, exercising regularly, managing stress, and avoiding tobacco use. Although trench mouth is a bacterial infection, doctors usually do not prescribe antibiotics unless there are systemic symptoms or the patient has a weakened immune system.

10. Prognosis
Most patients who receive treatment recover fully from trench mouth. Treatment may be more effective if it is caught early enough to halt the disease progression before tooth loss occurs. In this case, it is often possible to repair any damage to the gum tissue and prevent tooth loss altogether.
Patients who have had trench mouth must be careful to keep up good oral hygiene practices. Otherwise, the infection could recur. Having trench mouth once does not make one immune to it, and there is no vaccination against it.