What Is Seasonal Depression?
Seasonal depression is often referred to as seasonal affective disorder (SAD). However, it is simply a specific pattern in which Major Depressive Disorders or Bipolar Disorders can manifest, rather than a separate condition altogether. In fact, SAD is not listed in the DSM-V, which is a manual published by the American Psychiatric Association for assessment and diagnosis of mental disorders.
There is more to SAD than simply feeling down. If you have SAD, you notice that each year at around the same time, you begin to experience the same symptoms. Likewise, they start to ebb at approximately the same time each year. What this means, though, is that SAD is a recurrent syndrome that is linked to changes in seasons.
Most often, people are unaware of the fact that they are suffering from mental disorders. Thus, seeking treatment for SAD is often delayed. Moreover, seasonal affective disorder can have serious impacts on quality of life. It does not have to, though. There are treatments available that can help alleviate symptoms and improve day-to-day life.

1. Signs and Symptoms
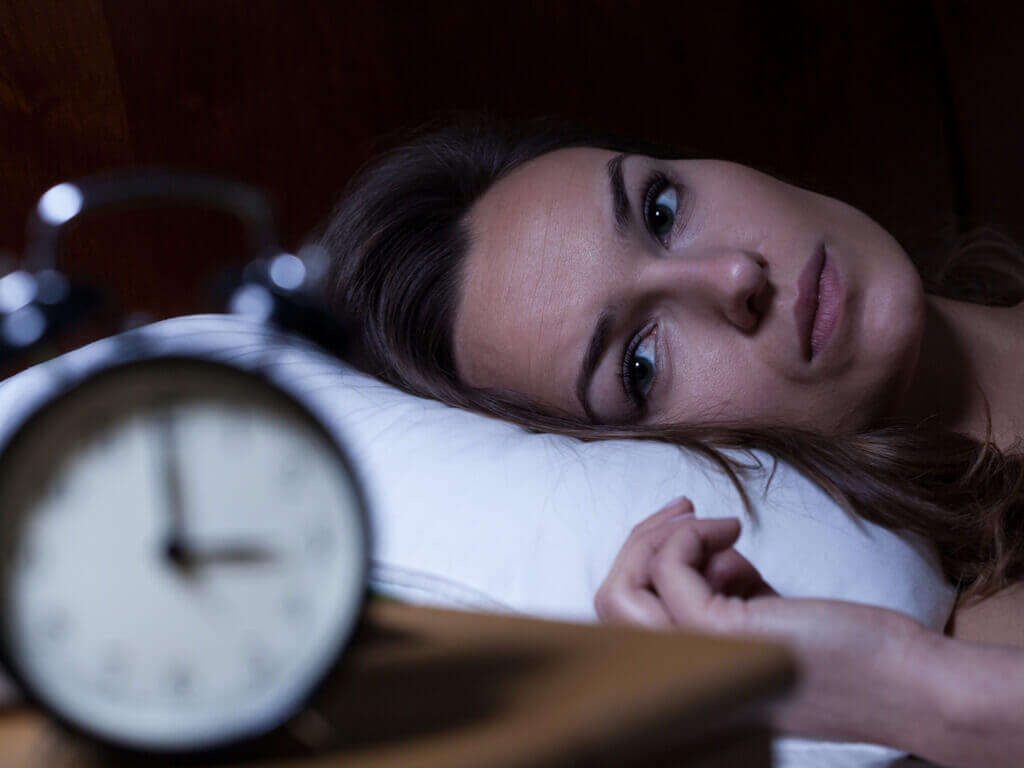
For most people, the symptoms of SAD start sometime in the late fall or early winter months. They typically disappear in late spring or early summer as daylight hours lengthen and the sun shines more often. If you have this disorder, you may feel depressed nearly every day and have low levels of energy. Sleeping difficulties and changes in appetite or weight are common.
People who have SAD often lose interest in activities they normally enjoy, are frequently sluggish or agitated, and can experience difficulty in concentrating. In addition, it is not uncommon to feel hopeless, guilty, or worthless during the winter months. Suicidal thoughts are also possible.

2. Winter vs. Summer Symptoms
While most people are affected by SAD during the winter months, there are those who experience symptoms during the summer. Symptoms that are specific to winter SAD include cravings for high-carbohydrate food and weight gain. Sleeping longer hours also occurs. Energy levels are low despite getting more sleep.
The onset of summer depression is typical during the spring months, with symptoms continuing through the summer. Those with summer SAD often have insomnia and consistently feel anxious or agitated. A loss of appetite with concurrent weight loss is common.

3. Complications
The symptoms of seasonal depression can worsen over time when left untreated. It is important to seek treatment if you experience symptoms of depression. If the condition worsens, it can lead to increased withdrawal from social life and contribute to problems at school or work.
Many people who do not get the help they need end up self-medicating, which can lead to substance abuse. It is not unusual to develop eating disorders or mental health conditions such as anxiety disorder. Suicidal thoughts and behaviors may also result from untreated SAD.

4. Causes
Scientists do not yet know exactly what causes Seasonal Affective Disorder. There are a few possibilities that may contribute to the disorder. A person’s circadian rhythm is a biological clock that is sensitive to light. When daylight hours decrease in the fall, this may lead to disruptions in an individual’s circadian rhythm, leading to depression.
Serotonin and melatonin levels may also come into play. Serotonin is a brain chemical that affects mood. The reduction of light in the late fall and winter months may cause a decline in levels, subsequently leading to depression. Similarly, melatonin is a chemical that has an impact on sleep and mood. The season change may impact melatonin balance and cause depression.

5. Epidemiology
As many as half a million Americans suffer from SAD, but, thankfully, most people experience a milder form. Moreover, more women than men suffer from SAD. The disorder typically begins early in adulthood, though children and teenagers can also develop seasonal depression. It is less common among older adults.
SAD is more prevalent in the higher latitudes and in regions where cloudy and rainy conditions are common, such as the Pacific Northwest in the United States. As the distance from the equator increases, so does the prevalence of seasonal depression.

6. Risk Factors
There are a few factors that seem to increase a person’s risk of developing seasonal depression. A person who lives in higher latitudes moves from a lower latitude to a higher one or moves from a sunnier location to a cloudier one is more likely to develop SAD.
People who have been diagnosed with bipolar disorder are also more likely to experience a worsening of their symptoms seasonally, as are those who have clinical depression. Finally, a family history of SAD or depression increases a person’s risk of developing this condition.

7. Diagnosis
Diagnosis of seasonal affective disorder can be challenging due to symptoms shared with a number of other mental health conditions. A doctor usually conducts a thorough physical exam and runs laboratory tests to rule out physical causes for depression.
If a physical cause is ruled out, a physician or mental health professional assesses your symptoms using a psychological evaluation. Moreover, the DSM-5 may be used to establish whether symptoms meet the criteria for diagnosis. According to this manual, in this pattern, depression should only be present at a specific time of year (fall/winter) and complete remission should occur at a distinctive time of year (spring). In addition, the patient in question should have experienced at least two episodes of depression in the last two years and seasonal episodes should outnumber nonseasonal ones.

8. Treatment: Medications
If you are diagnosed with SAD, your doctor may prescribe a combination of medication, therapy, and light therapy to alleviate your symptoms. Often, the same antidepressants that are used for the treatment of Major Depressive Disorder can be used to treat Major Depressive Disorder with a seasonal pattern.
Your doctor may suggest that you begin treatment before symptoms typically begin and continue past the time when they normally end. It can be a few weeks before the medication takes full effect, and it may take trial and error before finding the one that works best for you.

9. Treatment: Light Therapy
Light therapy can be especially beneficial in treating SAD, and it is frequently the first treatment approach recommended. Often, a special lightbox is used to mimic the type of light the sun emits.
The benefits of light therapy are generally felt within a few days, though it can sometimes take up to a few weeks. There are a number of different types of lightboxes available, so it is a good idea to speak with your doctor about which one is best for you. Your physician can also recommend when, how often, and for how long you should use the box.

10. Treatment: Psychotherapy and Mind-Body Connection
Psychotherapy and mind-body connection methods can provide coping mechanisms for dealing with the symptoms. Behavioral cognitive therapy, a type of psychotherapy, can teach a person how to manage stress, reduce avoidance behavior, and change negative thought patterns.
Mind-body connection techniques can help a person cope with the disorder and may improve mood. Yoga, tai chi, and meditation may all contribute to increased feelings of calm. Also, guided imagery may help to change thought patterns, and music and art therapy may help with relaxation.