What Is Sarcoidosis?
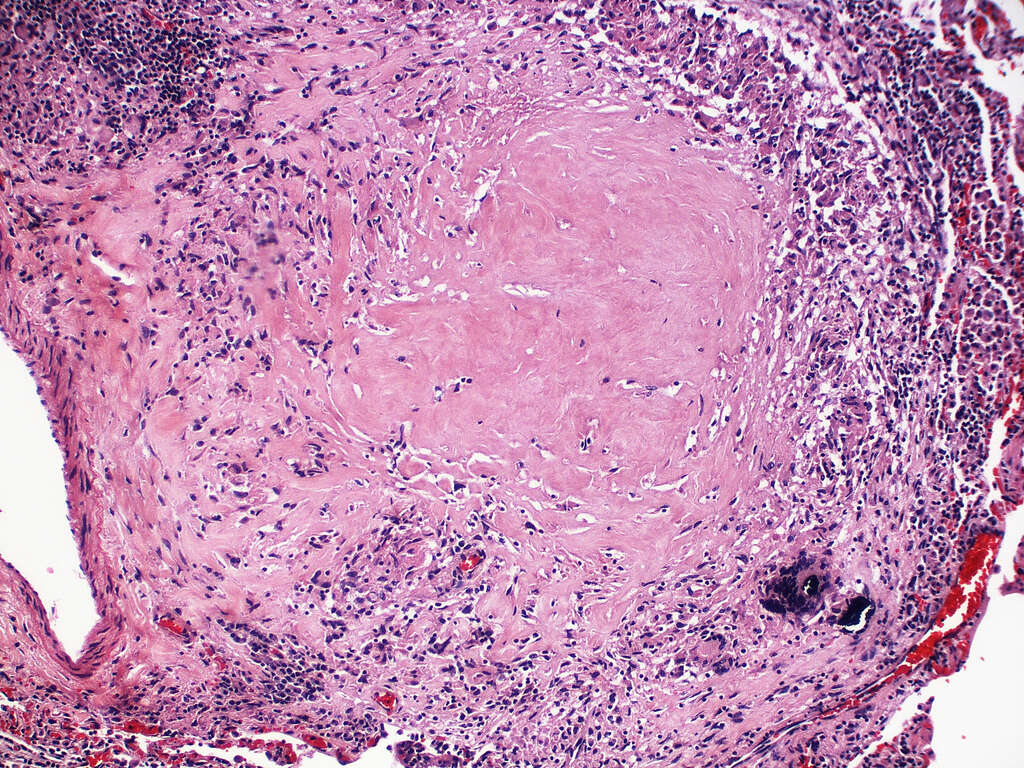
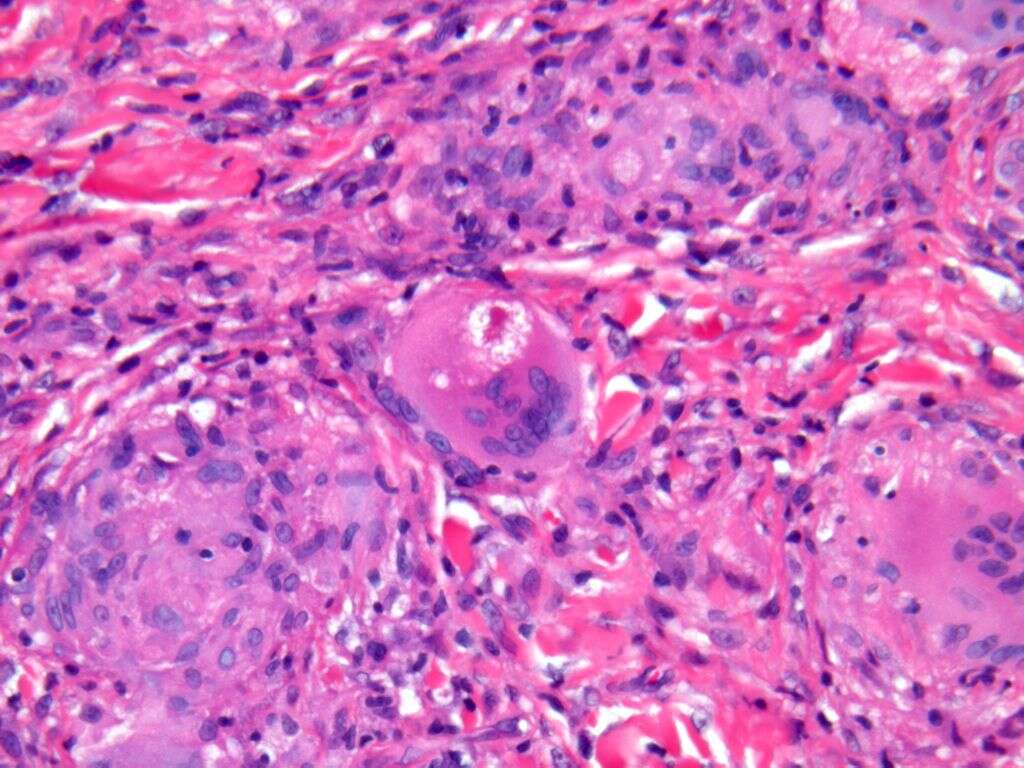
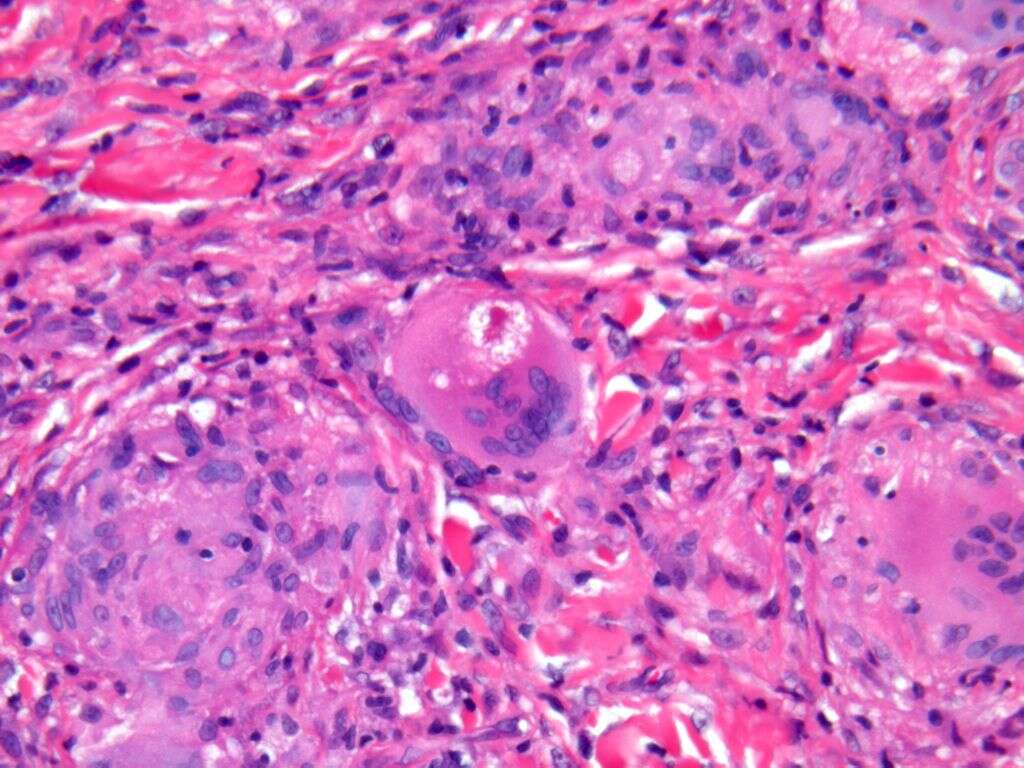
Sarcoidosis is a disease that presents itself in a variety of ways. The technical classification is an inflammatory disease, with the typical presentation being the formation of tiny clumps of inflammatory cells, or granulomas, in the organs of the body. The interesting thing about this condition is its varying degrees of evolution. Some patients will experience long-term symptoms, but others may have the disease go away on its own.
However, caution should be taken at any sign or symptom of the disorder because if the condition is left untreated, you may experience permanent scarring, or fibrosis, of organ tissue, which can lead to other complications. Before jumping ahead, it is necessary to understand the disease and what better way to do that than with some FAQs?
1. What Are the Symptoms of Sarcoidosis?
As sarcoidosis can affect different organs in the body, it is hard to stipulate definitive symptoms because the signs vary widely. Also, because of the varying degrees of the illness, some people have no signs of the disorder, while others are greatly affected. However, despite the difficulty of assigning a specific set of symptoms to sarcoidosis, many patients often present with Lofgren’s Syndrome, or a classic set of four symptoms: fever, swollen or painful joints, enlarged lymph nodes and erythema nodosum.
While the first three symptoms above don’t necessarily mean a definitive diagnosis, erythema nodosum, or red, tender bumps on the front of the legs, in combination with the other symptoms, is a good sign that the condition is present. However, due to the nature of the disease, there are a plethora of other possible symptoms, which means it is best to discuss all possible symptoms with your doctor.
2. What Causes Sarcoidosis?
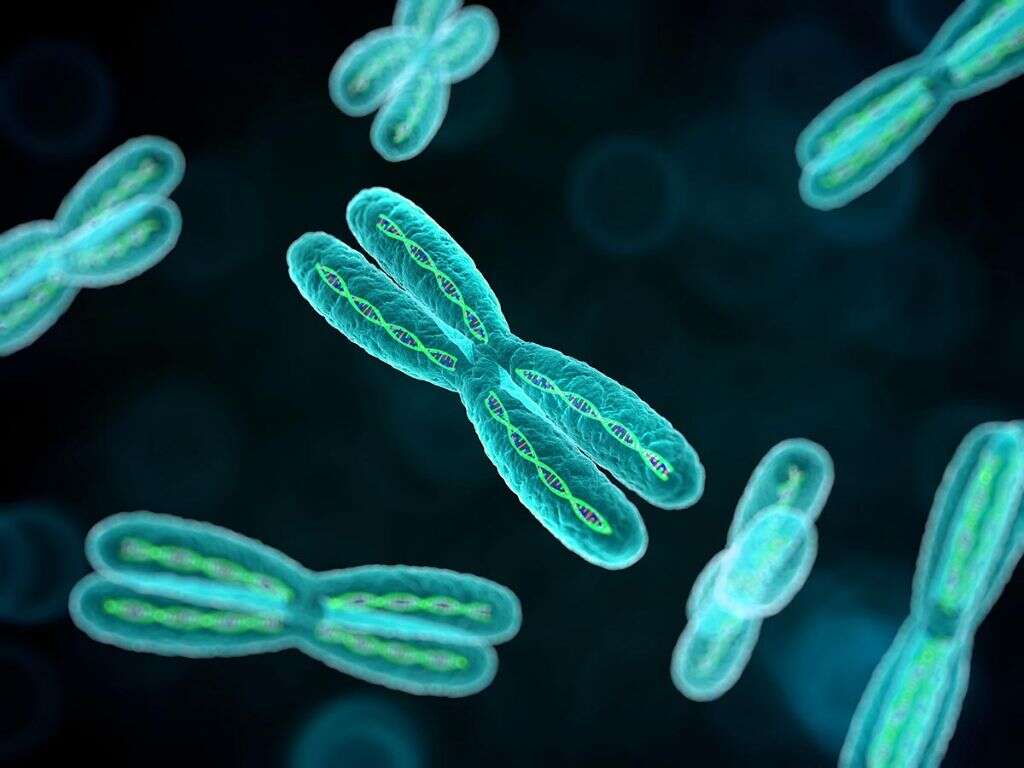
Unfortunately, there is no current explanation of the cause of sarcoidosis. Instead, there are theories and hypotheses. However, the most prevailing theory at the moment is that sarcoidosis affects people with a specific genetic makeup. In these people, an immune response is triggered in affected organs by some secondary element, likely bacteria. This response causes cells in the body to recruit inflammatory cells, leading to the inflammation of the affected organs.
Again, this is only a theory, but sarcoidosis does seem to involve an autoimmune response, but when it comes to identifying triggers, research has not come to any conclusions. Although, researchers do know that the condition is not as rare as it was once believed, as it affects millions of people worldwide, with an increased risk in people with other familial sufferers.

3. Does Sarcoidosis Affect Multiple Parts of the Body?
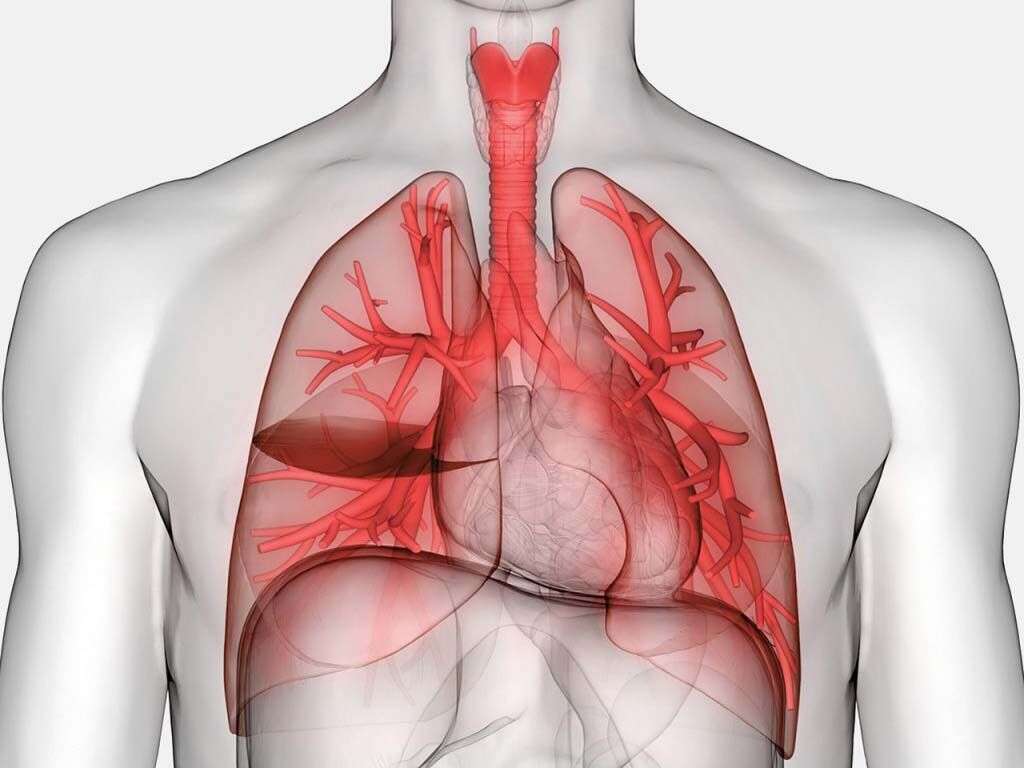
Yes. Sarcoidosis is considered a systemic disease, meaning that it can affect multiple organs in the body. The condition most often present in the lungs, causing chest pain, trouble breathing and dry coughing. In more severe circumstances, sarcoidosis in the lungs can evolve into several other conditions: pulmonary fibrosis, pulmonary hypertension, bronchiectasis, fibrocystic disease or aspergilloma.
Sarcoidosis also affects the lymph nodes in up to 90% of cases. While swollen lymph nodes can cause discomfort, they rarely cause further medical complications.
This disease can also affect other organs in the body, but likely with less frequency. For example, skin and the heart are affected in about 25% of cases, and only about 15% of cases affect the brain and nervous system. However, as always, if you are concerned that you may have sarcoidosis, then seek advice from a medical professional.

4. How Is It Diagnosed?
While many people wish there was a conclusive test for the diagnosis of sarcoidosis, there is not. In fact, this condition is considered a diagnosis of exclusion. In other words, a doctor must rule out all possible diseases related to your symptoms before confirming a sarcoidosis diagnosis. Therefore, your primary care physician will likely need you to submit to several tests.
These tests will likely include a mix of invasive and noninvasive procedures. Eleven tests are common in the pursuit of a diagnosis: lung function tests, chest X-ray, MRI, PET scan, blood tests, CT scans, nuclear imaging, echocardiogram, heart rhythm monitoring, lung biopsy and other biopsies.

5. Are There Any Known Complications?
Some complications may arise from the ongoing inflammation and formation of granulomas caused by sarcoidosis. For example, hypercalcemia is a condition where too much calcium form in the blood, and it can occur in up to 10% of patients. Also, sarcoidosis can lead to the suppression of PTH, which can lead to hyperthyroidism. Another common issue caused by this disease is vitamin D dysregulation, or low levels of vitamin D.
Beyond the above conditions related to granulomas, sarcoidosis can also lead to problems in the eyes. For example, cataract formation can occur in 14 to 30% of patients as a result of inflammation or steroid treatments. Also, because sarcoidosis can lead to the increased pressure of the optic nerve, it is possible for patients to experience glaucoma, which is why doctors recommend sarcoidosis patients see an optometrist at least twice per year.
Sarcoidosis can also lead to other issues commonly referred to as sarcoidosis syndromes. There are seven common syndromes: fatigue, erythema nodosum, vitamin D dysregulation, small-fiber neuropathy, depression, pain syndromes and cognitive impairment.
6. What Is the Outlook for Sarcoidosis Patients?
While sarcoidosis is not a terminal disease, it is difficult to estimate or provide a definitive prognosis. The fact is the disease affects all patients differently. Some may experience only short-term symptoms and effects, while others experience ongoing issues for two to five years or more. The best news for those affected by sarcoidosis is that once they enter remission, they are unlikely to experience a relapse.
However, remission only occurs in about 60% of patients. The other 40% likely experience a progressive disease that leads to scarring of the affected organs. For those patients, it is best to find a doctor who specializes in sarcoidosis treatment, as most physicians do not have adequate experience with the disease. However, there are possible signs that might indicate the version of the disease that will burn out: ethnicity, age or a sudden or short-lived attack.

7. Is Sarcoidosis a Lung Disease?
Sarcoidosis does generally affect the lungs in most patients. However, it is not labeled as a lung-only disease, as it can affect multiple organs in the body. Patients who suffer from this illness do need to be closely monitored, especially when they experience trouble breathing, dry coughing or wheezing, as these are all signs the condition is in the lungs.
If sarcoidosis does appear in the lungs it is not uncommon for people to experience scarring. Also, this scarring and the immune response can lead to the formation of cysts. While surgery is not always necessary, in severe cases it may be needed to maintain adequate lung function.

8. What Are the Treatment Options?
The good news is that many cases of sarcoidosis do not need medical intervention, tending to resolve on their own. However, for those who are diagnosed with a persistent form of the disease, consistent treatment is likely required. It is necessary to understand that treatment is not to cure the condition, only to control the symptoms, prevent further complications and possibly improve patient outcomes.
As sarcoidosis affects multiple organs, a patient will typically have a multidisciplinary team of medical professionals overseeing their treatment. There are a few drugs that have proven effective for the treatment of symptoms: corticosteroids, immunosuppressants and antimalarial drugs.
Also, if the disease is affecting the lungs, a doctor may recommend oxygen therapy. In rare and severe cases, a lung transplant might be needed to preserve lung function.

9. Is Sarcoidosis Genetic or Contagious?
Sarcoidosis is not contagious. However, the genetic correlation is a little more complicated. There are currently no screening options for the disease because the likelihood of relatives getting the disease is too low. Although, research suggests that if a first- or second-degree relative has the presence of sarcoidosis, there is an increased risk to family members. In fact, some studies suggest this genetic correlation increase likelihood five-fold.
Still, the role of heredity in the development of the disorder is still uncertain. Researchers do know that certain genes play a role in susceptibility. However, the evolution and effect of the disease depend on how those genes combine. Unfortunately, sarcoidosis is still a mystery. While physicians and scientists are learning more every day, there is still a lot of work to be done before a definitive cause can be determined.
10. Is There a Cure?
There is no cure for sarcoidosis currently available. However, the disease does tend to resolve itself in nearly 60% of cases, with many cases lasting two to five years. For those cases that result in persistent flareups, there are medical therapies to help curb the adverse effects of the symptoms. Also, beyond medications, patients may find comfort in seeking group or one-on-one therapy. Chronic conditions, like sarcoidosis, can lead to emotional and psychological issues, like depression and anxiety. Therefore, it is often beneficial for patients to combine medical and psychological therapies, ensuring they learn to live with their disease and still live a healthy and satisfying life.
As an autoimmune disease, sarcoidosis can be a scary diagnosis, especially since it requires a battery of tests to diagnose, but it is not the end of the world. Yes, it will involve change, and the disease might last five years or more, depending on the specifics of the presentation. However, through treatment, many complications can be avoided, allowing a patient to continue living a fulfilling life. The necessary thing is to seek treatment sooner rather than later. Early intervention is key to reducing some risks related to scarring and other issues. Therefore, if you are concerned that you might have sarcoidosis, don’t waste too much time before going to see your doctor.