What Is Rheumatic Heart Disease?
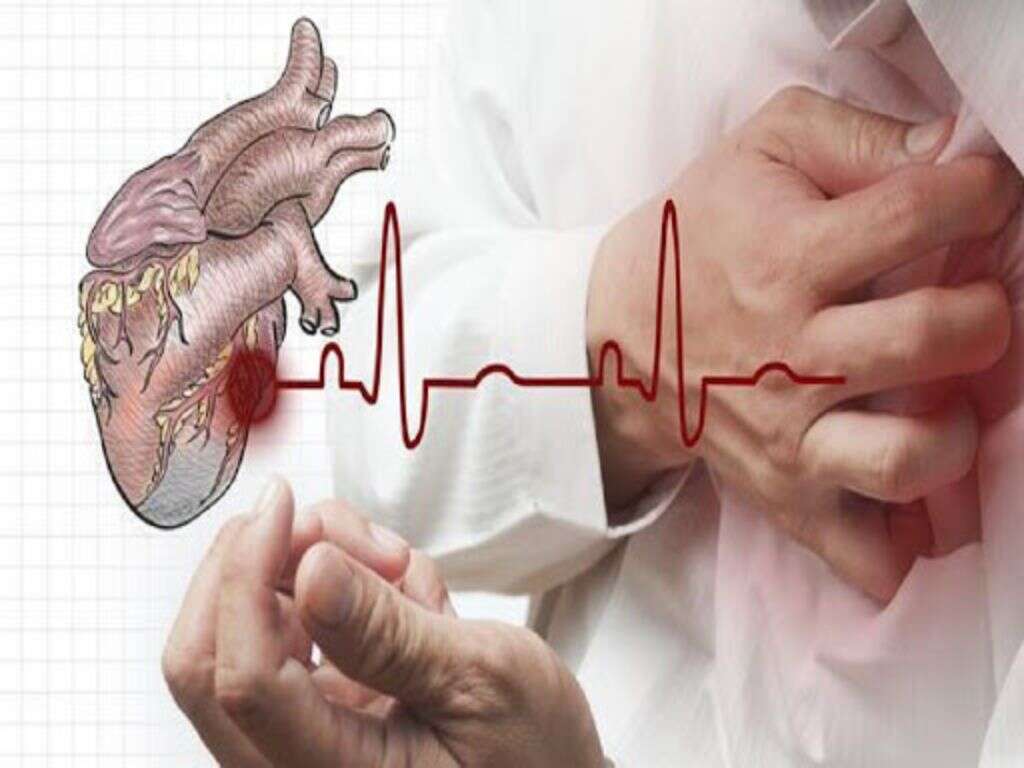
When a severe case of rheumatic fever causes permanent scarring of the heart, it is called rheumatic heart disease. The heart valves are the most common area affected. It can manifest as sudden acute episodes of illness or as a variety of chronic heart disorders.
Damage can begin shortly after infection and continues to develop slowly over time. You may not notice any issues for several years. In fact, most rheumatic heart disease symptoms will begin to appear 10 to 20 years after the infection. Despite the lapse in time between the disease and the cause, the heart damage will always be traced back to an incidence of rheumatic fever. Keep reading to learn the answers to 10 common questions about rheumatic heart disease.
1. What Are the Types of Rheumatic Heart Disease?
The type of disease that develops is dependent on which parts of the heart are damaged. Rheumatic heart disease most commonly affects the heart valves; however, damage can occur to other parts of the heart, including the pericardium (outer sac) and endocardium (inner lining). The heart muscle itself may also be damaged, making it difficult for it to pump blood effectively.
Valve stenosis is a narrowing of the heart valves that restricts blood flow, while valve regurgitation occurs when blood flows in the wrong direction through a valve. Both are common conditions of rheumatic heart disease. Without proper care, valve disorders can potentially lead to arterial fibrillation and heart failure.
2. What Causes Rheumatic Heart Disease?
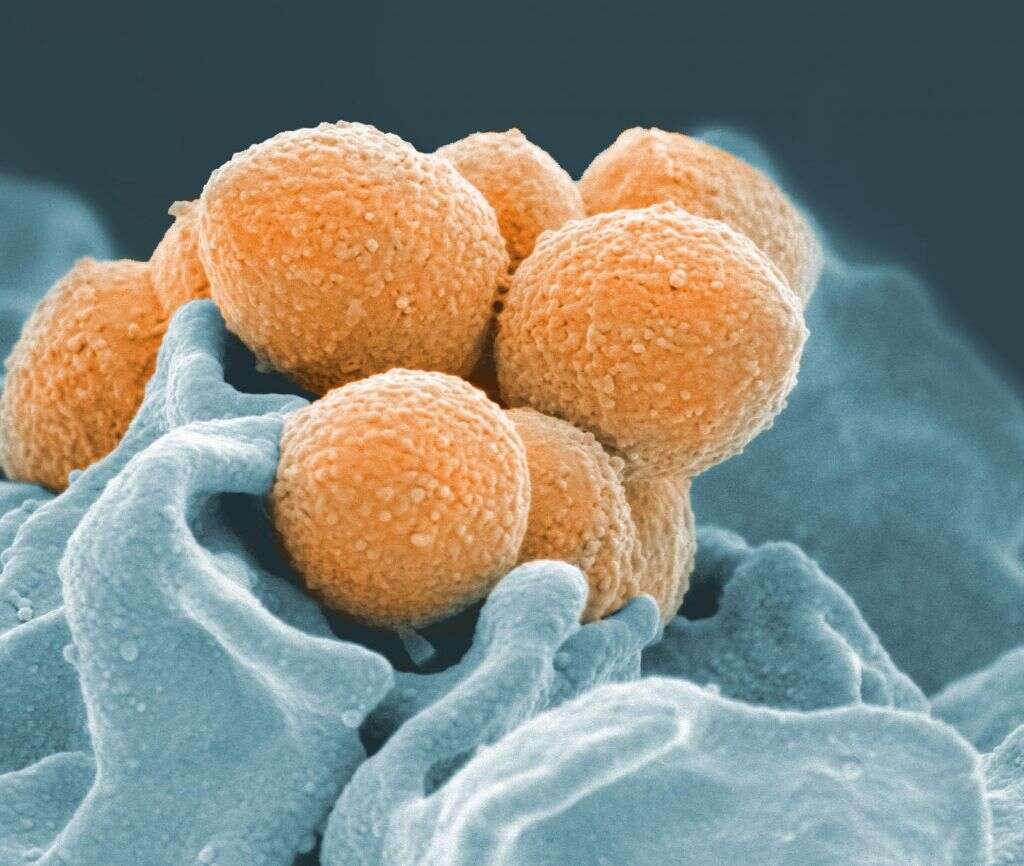
Rheumatic fever is an inflammation that commonly affects young people, and it is the cause of rheumatic heart fever. It develops when scarlet fever or strep throat caused by group A streptococcus bacteria is not treated correctly. Children between the ages of 5 and 15 are at the highest risk of developing an infection from this bacterium, so care should be taken to limit their exposure to sick people.
Left unchecked, rheumatic fever causes damage to connective tissues of the brain, joints, heart and skin. When that damage extends to the heart, it leads to rheumatic heart disease. That is why it is vital to get an accurate diagnosis of those conditions, no matter how minor they seem, and follow all treatment recommendations.

3. What Are the Symptoms of Rheumatic Heart Disease?
A diagnosis with rheumatic fever can be an early indicator of rheumatic heart disease. It is characterized by fever, painful and swollen joints and pain that radiates outward from the joints. Many people also develop a nonpainful rash with jagged edges along with the infection.
Rheumatic fever that has damaged the heart valves has its own set of symptoms that are characteristic of other heart valve disorders. These include chest pain, shortness of breath, lightheadedness, dizziness or syncope, heart palpitations and swelling of the feet or ankles.
4. How Is Rheumatic Heart Disease Diagnosed?
There is no specific test to diagnose or rule out rheumatic heart disease. Instead, it is often diagnosed after a complete physical exam and review of symptoms and your medical history. Your history must include an episode of rheumatic fever for a doctor to arrive at a diagnosis of rheumatic heart disease.
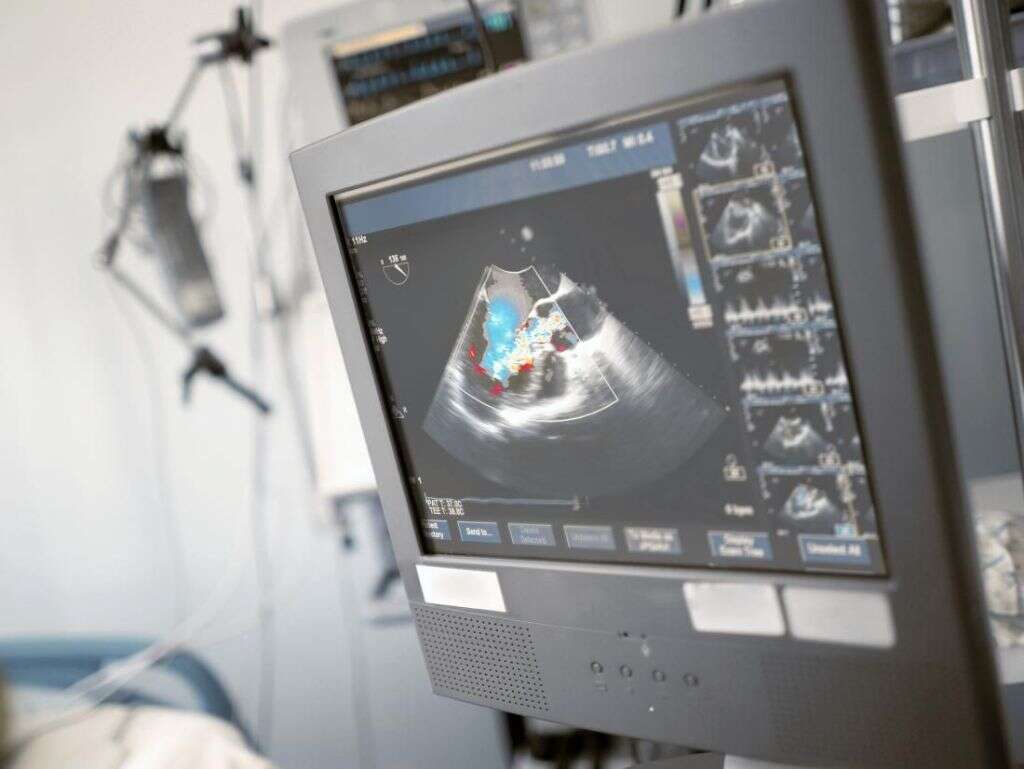
Specific tests are used to check for heart damage. An echocardiogram is a particular type of ultrasound imaging test that uses sound waves to create a detailed picture of the heart. It can often detect irregularities in the valves and their function. Chest X-rays are useful for uncovering any enlargement or failure of the heart muscle.
5. What Are the Risk Factors for Developing Rheumatic Heart Disease?
Although it does not guarantee you will develop heart disease, a past diagnosis of rheumatic fever is the most prominent risk factor for developing it. Children who have a history of repeated strep throat infections have a higher risk than others of developing rheumatic heart disease.
Other risk factors that contribute to general heart disease can increase your risk of complications from heart damage. These include smoking, lack of exercise and a family history of heart disease.

6. Can Rheumatic Heart Disease Be Prevented?
The only way to truly prevent it is to avoid infection with group A streptococcus bacteria. Treating strep throat or scarlet fever completely and early is the most effective way to prevent complications like rheumatic heart disease. Antibiotics can treat both conditions if appropriately administered.
Antibiotics are particular medications that treat bacterial infections. You should always take them as prescribed and finish the entire course of medicine, even if you feel better. Failure to do so can result in a resurgence of the infection and make it more resistant to treatment.
7. How Is Rheumatic Heart Disease Treated?
Treatment for rheumatic heart disease will vary depending on the level of damage sustained. Some therapies focus on repairing damage to the heart; others address symptoms of the disease. Steroids and anti-inflammatory medicines can help reduce swelling, while diuretics help reduce fluid retention around the heart or in your extremities.
Some people with extensive valve damage will need to undergo a valve replacement. Either biological valves from a donor or mechanical ones can be used to replace defective or damaged mitral valves.

8. When Should You See a Doctor About Rheumatic Heart Disease?
You should always contact your healthcare provider if you suspect there are problems with your heart. The sooner you receive care, the less permanent damage you are likely to incur. They can help you address symptoms and live the fullest life possible.
Some cardiac situations are emergencies, however. So, if you are experiencing chest pain and shortness of breath, dial 911 for emergency assistance. A few minutes can mean the difference between a full recovery and irreversible heart damage.
9. What Complications Result from Rheumatic Heart Disease?
Without proper treatment, you can develop a host of complications from heart disease. Heart failure can result from a narrowed or leaking heart valve. A damaged valve might rupture, causing an emergency and the need for a replacement valve to be inserted.
Bacterial endocarditis, an infection of the lining within the heart, can also develop from damaged valves. Additionally, women with rheumatic heart disease are at a higher risk than others for cardiac complications during pregnancy and childbirth. They should carefully discuss their condition with their doctor before becoming pregnant.
10. What Is the Prognosis After a Diagnosis of Rheumatic Heart Disease?
Receiving a diagnosis of heart disease is not a death sentence. Provided the damage is minimal, and you follow your healthcare provider’s advice, you can live a full and healthy life. Regular monitoring of heart function is useful for avoiding complications.
In cases where there is more extensive damage, you may need to make some adjustments to your routine. This can include restricting or modifying activities that would cause undue strain on your heart.