What Is Respiratory Distress?
Any way you look at it, breathing is critical to survival. With each breath in, your body is able to extract vital oxygen from the air and send it throughout your body. This process, known as respiration, is an automatic action completed without any thought on your part no matter what else you are doing.
Unfortunately, there are times when your body is unable to draw enough oxygen from the surrounding environment, or when it has to work much harder to get the supply it needs. You then enter a state called respiratory distress. Here are 10 facts about respiratory distress that can help you stay informed.
1. Types of Respiratory Distress
Respiratory distress is a critical condition that can seriously affect your quality of life. Since your body is unable to get enough oxygen to supply vital organs and may also struggle to eliminate carbon dioxide, it should be addressed immediately for the best outcomes. The two main types of respiratory distress are characterized by their duration.
Chronic respiratory failure is a prolonged condition where the lungs are not able to exchange sufficient oxygen and carbon dioxide levels. This is commonly found in people with underlying lung conditions such as chronic obstructive pulmonary disease (COPD) or lung cancer, and treatment can be conducted at home. Acute respiratory distress is a sudden and short-lived medical emergency which may resolve with treatment in a hospital setting.
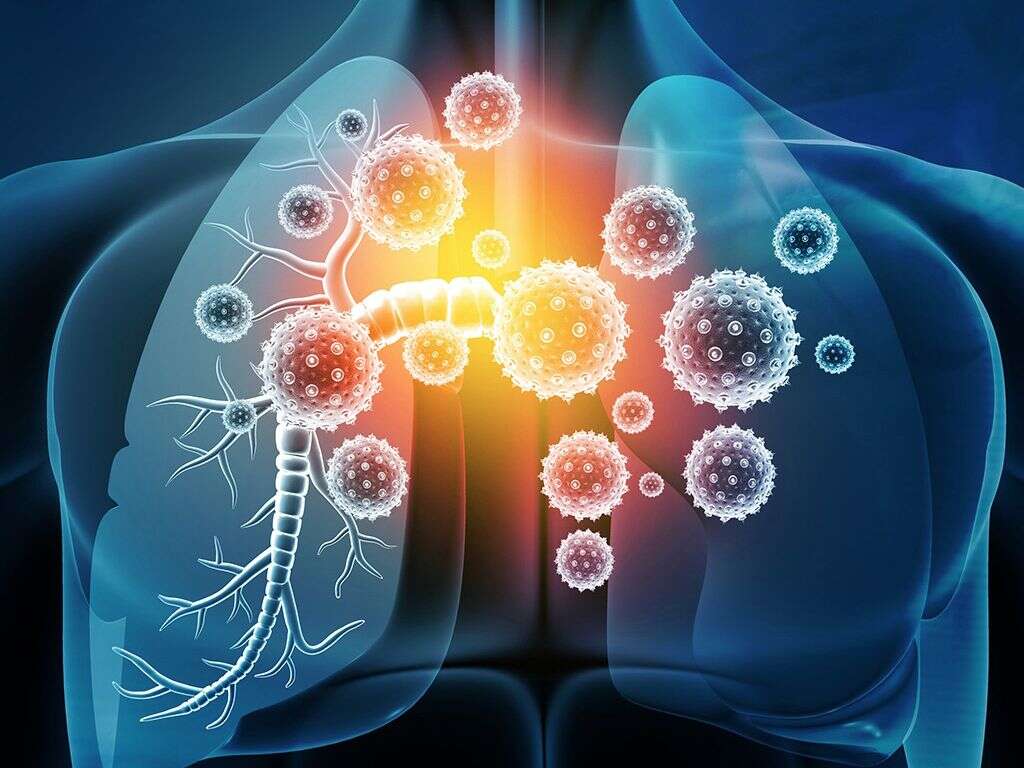
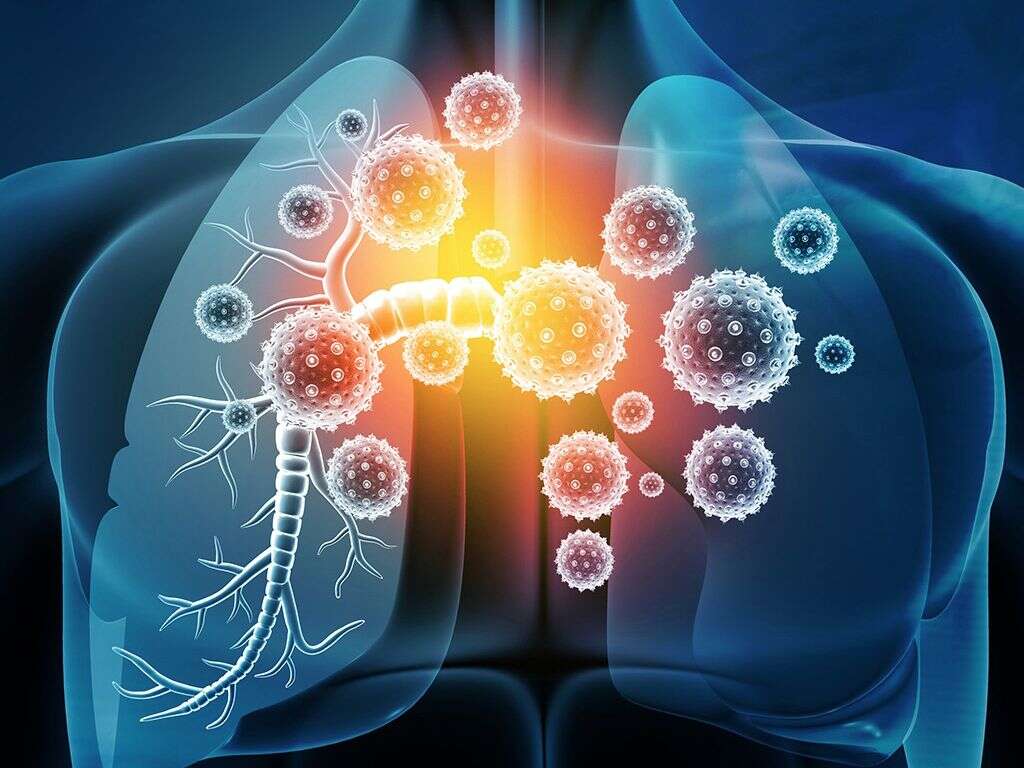
2. Acute Respiratory Distress Syndrome
A very specific disease, acute respiratory distress syndrome affects the lungs’ ability to function. The tiny air sacs inside the lungs fill with fluid instead of air, causing the surfactant that attracts oxygen particles to dissolve and making them ineffective.
ARDS often results from an underlying lung condition or illness. Symptoms may progress slowly over several days, or it can come on suddenly. Scarring of lung tissue is a common result, which makes a long-term recovery difficult.

3. Signs of Respiratory Distress
The symptoms of respiratory distress are similar, regardless of the cause. They include shortness of breath, trouble drawing a deep breath, grunting on exhalation and wheezing. As oxygen levels become depleted, you may experience sweating, nose flaring and hollowness around the breastbone as you struggle to draw air into your lungs.
Color changes in extremities is another serious effect of low oxygen. The lips and fingers are the most common places to look for signs of hypoxia. A slight blue tinge will begin to appear, indicating that oxygen supplementation is necessary.

4. Diagnosing Respiratory Distress
The signs of respiratory distress are fairly straightforward, and it is often diagnosed through a physical exam. Your doctor will listen to your lungs for wheezing and congestion, check your heart rate and look for signs of hypoxia. There are also specialized tools that can be used to aid in diagnosing the condition and its severity.
A pulse oximeter is a simple, non-invasive device that is placed on your finger. It detects the amount of oxygen saturation within your blood within seconds and can be worn continuously to detect changes. An arterial blood gas test can be conducted to get an accurate measurement of both oxygen and carbon dioxide levels in the blood.

5. Treatment Options
Treatments consist of two main phases: those designed to address immediate respiratory distress and those that work to manage long-term symptoms. The longer your organs are without sufficient oxygen, the more likely they are to experience scarring or other damage. Immediate supplementation with oxygen through traditional or non-invasive ventilation can stop that process.
Medicines, including blood thinners, acid reducers and muscle relaxants are often used to address symptoms of distress. Body positioning, physical therapy and nutritional support can help manage the condition on an outpatient basis.

6. The Role of a Pulmonologist
Any time there is a condition that affects the health of your lings, it is wise to seek care from a pulmonologist. They have specialized knowledge about disorders of the respiratory system as well as the access to the latest diagnostic tests and treatment equipment.
Everything from caring for chronic lung disorders, ventilating a patient and performing lung transplants will be done by a pulmonologist. In the case of respiratory distress, they work to supply supplemental oxygen as needed, determine the cause of symptoms and diagnose any underlying conditions. In addition, respiratory specialists design care plans that can help you manage your condition over time.
7. Prognosis After a Diagnosis
While a diagnosis of respiratory distress can be scary, the prognosis for many people is very good if treatment is started right away. Once any acute episodes are addressed, treatment can often continue at home. You will need to be monitored with lung function, muscle strength and physical capacity tests. It is also important that any medication is taken exactly as prescribed.
Lifestyle choices can greatly impact your recovery process. One of the major contributors to repeat episodes is exposure to lung irritants, like those found in cigarette smoke. If you are currently a smoker, take steps to quit; if you aren’t, then don’t take up the habit. Regular exercise can also help strengthen the lungs and supporting thoracic muscles to make respiration easier and more efficient.

8. Risk Factors Associated with Respiratory Distress
Some people are more likely to develop respiratory distress and ARDS than others. Lifestyle choices, such as poor exercise habits and choosing to smoke, can greatly increase your likelihood of respiratory failure.
Genetics appears to play a role in developing respiratory distress as a family history increases your chances of developing it yourself. Demographics also appears to play a role. For example, ARDS is more common among non-white populations and males.

9. Causes of Respiratory Distress
Respiratory distress is the result of damage to the tissues within your lungs. This can be caused by a number of factors. Bacterial or viral infections that result in pneumonia are common contributors to that type of damage. Exposure to chemical and environmental irritants and certain medical procedures or conditions can also impact lung function.
In some cases, damage to the spine or to the muscles that support lung function results in respiratory distress. This may be the effect of trauma or an ongoing medical condition such as multiple sclerosis or amyotrophic lateral sclerosis (ALS).
10. Preventing Respiratory Distress
Unfortunately, there is no way to guarantee that you won’t develop respiratory distress, but there are things you can do to lower your chances. If you have an underlying medical condition, follow the advice of your doctor and take your medications as prescribed. Contact your provider if you notice any symptoms or changes in your condition.
Adopting a healthy lifestyle will also help. Limit your exposure to airborne pollutants and irritants whenever possible, and use appropriate filtration devices when you can’t avoid exposure. Make exercise a regular part of your routine to strengthen muscles and improve lung function and avoid high-risk behaviors like smoking whenever possible.