What Is Pneumonia?
Pneumonia is a condition where there is inflammation in the lungs affecting the alveoli. It is usually caused by various microorganisms such as viruses or bacteria, autoimmune conditions, and medications. The air sacs can also be filled with pus or fluid, resulting in symptoms. Pneumonia can range from mild to life-threatening. It can also be classified based on how it was acquired.
Vaccines for the prevention of pneumonia are also available. Treatment of pneumonia will depend on the underlying cause along with supportive care. Although it can occur in individuals of all ages, it is more common among young children and the elderly, probably due to a weaker immune system. It is estimated to affect about 450 million individuals, resulting in about 4 million deaths annually. The incidence is highest among children less than 5 years old and adults more than 75 years old. It is 5 times more frequent in the developing world compared to developed countries.
1. Signs and Symptoms
In infectious pneumonia, the patient generally experiences productive cough, shaking chills, fever, breathlessness, tachypnea (increased breathing rate), and chest pain during deep breaths. Confusion can be the most prominent sign among the elderly. In children, additional symptoms include unwillingness to drink, vomiting, cyanosis (bluish tinged skin), decreased level of consciousness, extremes of temperature, and convulsions. Both bacterial and viral pneumonia usually causes similar symptoms; however, in some cases, it can also be associated with nonspecific symptoms. For example, pneumonia caused by Legionella can result in diarrhea and abdominal pain.

2. Causes
Pneumonia is usually caused by a bacterial or viral infection and less commonly by parasites and fungi. Although there are more than 100 strains of pathogens that can cause pneumonia, only a few have been implicated for a majority of the cases. In 45% of children and 15% of adults with pneumonia, it has been attributed to a mixed infection. Despite careful testing, as many as 50% of cases do not have an isolated causative agent.
The most common bacterial pneumonia is caused by Streptococcus pneumoniae. Other bacteria include Hemophilus influenzae, Chlamydophila pneumoniae, and Mycoplasma pneumoniae. Commonly implicated viruses are rhinoviruses and coronaviruses.
3. Mechanism
Pneumonia usually begins as an upper respiratory tract infection that progresses to involve the lower respiratory tract. In the upper airway, the normal flora provides protection by competing for nutrients with the pathogens. Once in the lower airways, it is protected by the reflex of the glottis, immunoglobulins, and complement proteins. When the secretions infect the lower airways, it results in pneumonia.
The progress of the disease depends on the amount of organisms, the immune response of the individual, and virulence of the organism. Bacteria usually enter the lungs through small aspirations that occur during sleep. Viruses can reach the lung via airborne droplets. They then invade the alveoli and cells lining the airways.
4. Diagnosis
Pneumonia can usually be diagnosed based on patient history, physical examination, and a chest X-ray. While the diagnosis of pneumonia is easily achievable, determining the underlying cause can be difficult.
Tests that may be performed include a complete blood count (CBC), pulse oximetry, sputum test, arterial blood gas, bronchoscopy, computed tomography (CT) scan, serum electrolytes, liver function tests, C-reactive protein level, and pleural fluid culture. Although a lung ultrasound can also be useful for diagnosis as it can be more accurate than a chest X-ray, it requires specific skills for both operation of the machine and interpretation of findings.

5. Classification
Pneumonia is generally classified based on how it was acquired. For example, community acquired, healthcare-associated, ventilator-associated, aspiration, and hospital-acquired pneumonia. It can also be classified based on the area of lung affected such as acute interstitial pneumonia, bronchial pneumonia, or lobar pneumonia.
It can also be classified based on the causative organism. In children, it can be classified based on the severity: non-severe, severe, and very severe. The setting of which pneumonia develops is important as it plays a crucial role in deciding the treatment for pneumonia. Depending on which setting it develops, it points to likely pathogens, possible mechanisms, and which antibiotics are the best option.

6. Types of Pneumonia
As the name suggests, community-acquired pneumonia is acquired in the community outside of the healthcare system. It is common and can affect individuals of all ages. It is the most common type of pneumonia and is the leading cause of illness and death globally. It can be caused by bacterial, viral, parasitic, or fungal infection.
In healthcare-associated pneumonia, the infection can be associated with a recent exposure to the healthcare system such as the nursing home, hospital, dialysis center, and outpatient clinic. Hospital-acquired pneumonia is acquired in the hospital 48 hours or more after admission. This type of pneumonia has a higher risk of multidrug resistant pathogens. Ventilator-associated pneumonia can be defined as pneumonia that occurs 48 to 72 hours after endotracheal intubation.
7. Prevention
The risk of pneumonia can be decreased through vaccination, treatment of other health issues, and environmental measures. Some experts have estimated that with proper prevention globally, the mortality among children could be reduced by 400,000. With proper treatment available readily, it could be decreased by another 600,000.
With influenza outbreaks, medications such as rimantadine and amantadine can help prevent pneumonia. Oseltamivir and zanamivir can be given to individuals at risk who are exposed to the virus; although the CDC states that this mode of prevention is not effective. Other measures include reducing indoor air pollution and stopping smoking. Those who are sick can also help by wearing surgical masks. Good hand hygiene may also be beneficial.

8. Vaccination
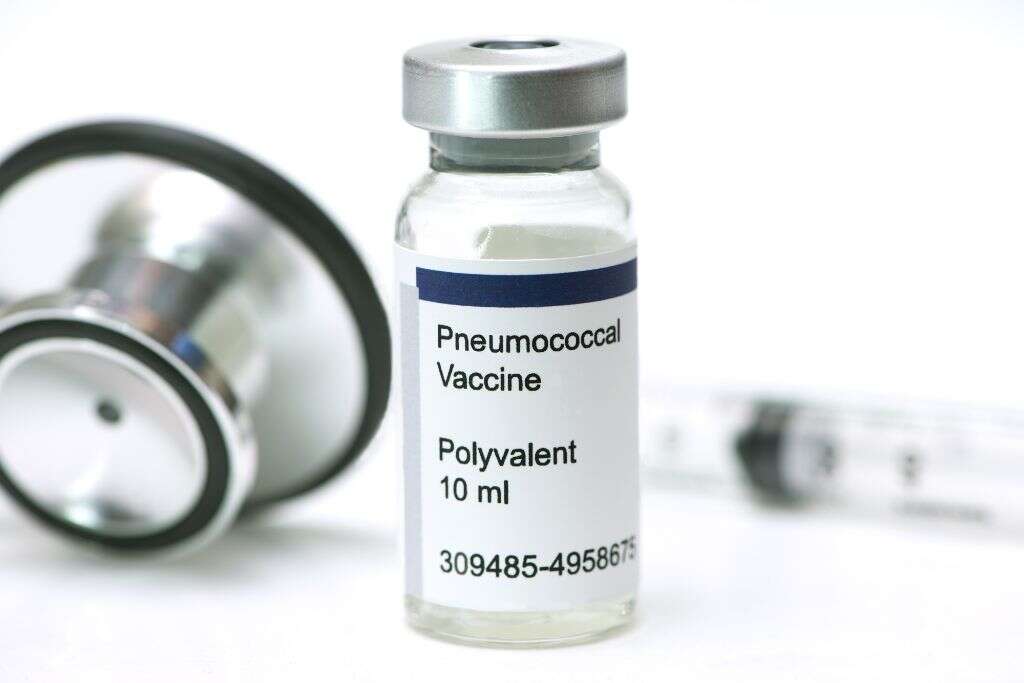
Vaccination for the prevention of both bacterial and viral pneumonia is available for adults and children. The Center for Disease Control and Prevention (CDC) has recommended that influenza vaccination should be given yearly for all individuals 6 months or older.
The immunization of healthcare workers helps decrease the risk of viral pneumonia as they come into contact with many people. Influenza vaccines have been shown to be modestly effective while vaccines for Streptococcus pneumoniae and Hemophilus influenza have good evidence. The vaccination of children against Streptococcus pneumoniae has decreased the rate of infections in adults. The pneumococcal vaccine is recommended for young children and the elderly (above 65).
9. Treatment and Management
Simple analgesics, rest, and fluids can help support the patient. Hospitalization may be required for those with significant breathing difficulties. For the treatment of bacterial pneumonia, antibiotics by mouth can be given for those suspected with a bacterial infection.
The choice of antibiotics depends on the individual: age, health, and how the infection was acquired. In North America, macrolides such as erythromycin or azithromycin, and doxycycline, could be the first line for community-acquired pneumonia. Corticosteroids have also been observed to improve the prognosis for adults with severe community-acquired pneumonia. Courses of treatment include neuraminidase inhibitors for viral and antibiotics for pneumonia.
10. Prognosis
Most types of bacterial pneumonia generally stabilizes within 3 to 6 days with treatment. However, it may take several weeks before the symptoms resolve. The recovery period may take more than 12 weeks for the elderly and individuals with lung issues. In those with underlying health issues or the elderly, complications of pneumonia may occur.
Examples include lung abscess, empyema, sepsis, acute respiratory distress syndrome, and bronchiolitis obliterans. The prognosis can also be predicted using clinical prediction rules such as the CURB-65 score and pneumonia severity index. The CURB-65 score takes into account any underlying diseases, age, and the severity of symptoms.