What Is PID?
Pelvic inflammatory disease is a potentially serious condition that affects women. Luckily, many cases of PID can be prevented through knowledge and protective measures.

1. What Is Pelvic Inflammatory Disease?
Pelvic inflammatory disease occurs when the reproductive organs of a female person develop inflammation and infection. Affected organs can include the cervix, uterus, Fallopian tubes, ovaries and the surrounding tissues.
It is important for cases to be identified and treated promptly to avoid complications. If recognized and treated, many cases can be resolved without long-term or permanent issues.

2. What Causes PID?
Pelvic inflammatory disease is typically caused by bacteria that is present in the vagina moving into the uterus to cause a bacterial infection. From the uterus, the infection can travel through the Fallopian tubes and affect the ovaries and surrounding tissues.
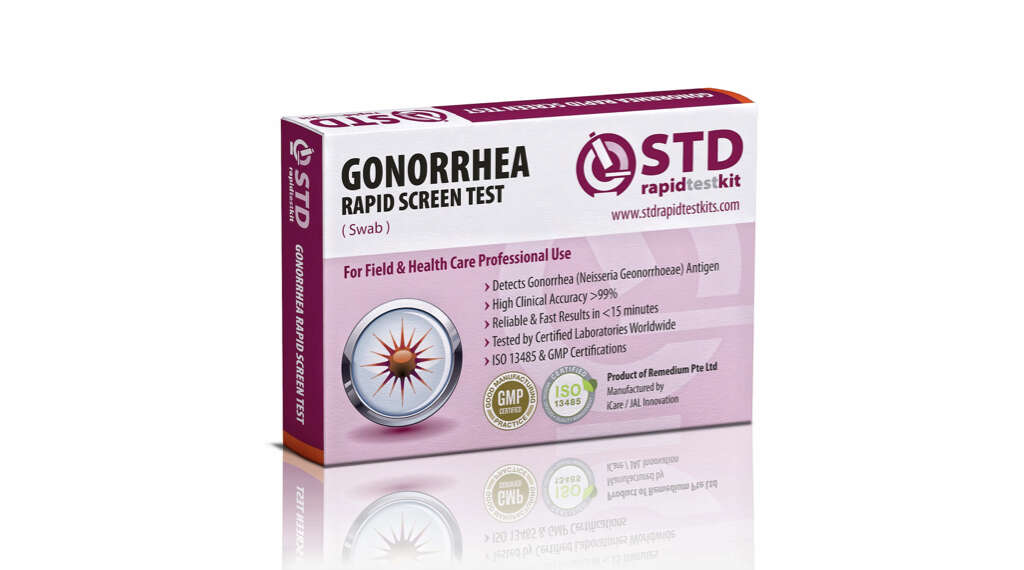
The most common cause of bacterial infection in the vagina is a sexually transmitted infection. Cases of gonorrhea and chlamydia can progress into PID if not recognized and treated. In some cases, bacteria that is normally present in the vagina travels into the uterus and causes an infection.

3. Are All Cases of PID Sexually Transmitted?
Although the most common way to become infected with PID is through sexual contact, not all cases are caused by sexually transmitted infections. It is normal for bacteria to be found in the vaginal canal, but this bacteria usually remains in place. However, sometimes the bacteria travels through the cervix and into the uterine cavity.
In the past, PID that was not sexually transmitted was frequently caused by douching. This practice is not recommended by doctors because of the potential to push bacteria up into the uterus and because it can remove healthy bacteria from the vagina. This can lead to an overgrowth of harmful bacteria. There is also a risk of PID during the first few months after an IUD is placed.

4. What Are the Symptoms?
Some women who have PID do not have symptoms at all or for a long period of time as the infection worsens. When symptoms develop, they can sometimes be mistaken for other conditions or are mild enough to ignore for a while. For some women, though, the symptoms can be severe and begin quickly after infection. Nausea and vomiting sometimes occur in conjunction with other symptoms.
The most frequently reported symptom is pelvic pain, often accompanied by a fever. The patient may also experience vaginal discharge that has an unpleasant smell. Pain may be present or worsen when urinating or during sex. Some of the symptoms may be attributed to the underlying infection, such as gonorrhea, but the physician should also check for PID.
5. When Should You Call the Doctor?
If you suspect you have a sexually transmitted disease of any kind, you should contact your doctor for an evaluation. STIs that are not diagnosed and treated in a timely manner can progress into PID, sometimes quickly. Even if you are not showing symptoms, if you have a sexual partner who has tested positive for a sexually transmitted disease, you should contact your doctor for a test.
Any symptoms of PID or STI are a cause for a doctor’s visit. Even if you are not sexually active, if you have the symptoms of pelvic inflammatory disease you should be checked. Other conditions can cause similar symptoms, so your physician can rule out other issues. If you have recently had an IUD placed and are showing symptoms, contact your gynecologist immediately.

6. How Is PID Diagnosed?
Pelvic inflammatory disease requires a diagnosis from a physician, such as a general medicine practitioner, family medicine doctor or gynecologist. The doctor completes a physical exam to check for tenderness in the abdomen in the areas surrounding the reproductive organs and look for visible signs of infection in the vagina and around the cervix.
If the doctor finds discharge, a sample may be taken for analysis. If the patient is sexually active, especially with multiple partners, tests for gonorrhea and chlamydia are usually performed. A test for a urinary tract infection is often performed, especially if the patient is experiencing pain during urination.
7. What Is the Treatment For PID?
The treatment for PID depends on the severity of disease advancement. Most cases can be treated with antibiotics. The type of bacteria causing the PID can be difficult to pinpoint, so it may take more than one course of antibiotic treatment to clear the infection.
More severe cases may need surgery, particularly if a pelvic abscess has developed and is in danger of rupturing. If antibiotic treatment has been tried without resolution, surgical intervention may be necessary to clean out the remainder of the infection.

8. Can PID Be Cured?
If caught early enough, pelvic inflammatory disease can be treated and resolved without any long-lasting or permanent damage. Antibiotic regimens should always be completed even after symptoms begin to go away to make sure the infection has resolved.
In more severe cases of PID, permanent changes to the reproductive system can occur. These changes may not resolve even when the infection has subsided.

9. What Are the Risk Factors for Developing PID?
Certain behaviors increase your risk of developing PID during your lifetime. Having multiple sexual partners or having one partner who has multiple sexual partners increases your risk of sexually transmitted infections as well as PID. Modifying your sexual behavior can reduce your risk of developing PID. Using a condom with every sexual encounter and only engaging in sexual activity with one partner both lower the risk.
While abstinence greatly reduces the risk of PID, those who are not sexually active can still develop PID by douching or through the use of an IUD. PID from IUD insertion is not commonplace. It is important to not douche and to follow up with your gynecologist within the first few weeks of an IUD insertion to look for signs of infection. Also, if you have had PID once, you are more likely to develop it again.

10. What Are the Dangers of PID?
Pelvic inflammatory disease that is left untreated can become a more severe infection. Some infections develop into a pocket of pus in the pelvic region, called an abscess. An abscess may require surgical intervention, especially if it is at risk of rupturing.
A severe infection can also lead to the development of scar tissue around the reproductive organs such as the ovaries and Fallopian tubes. This can cause pelvic pain or fertility issues that may be permanent. It is important to consult with your physician as soon as possible if you suspect PID to reduce the chances of these complications.