What Is Pancreatitis?
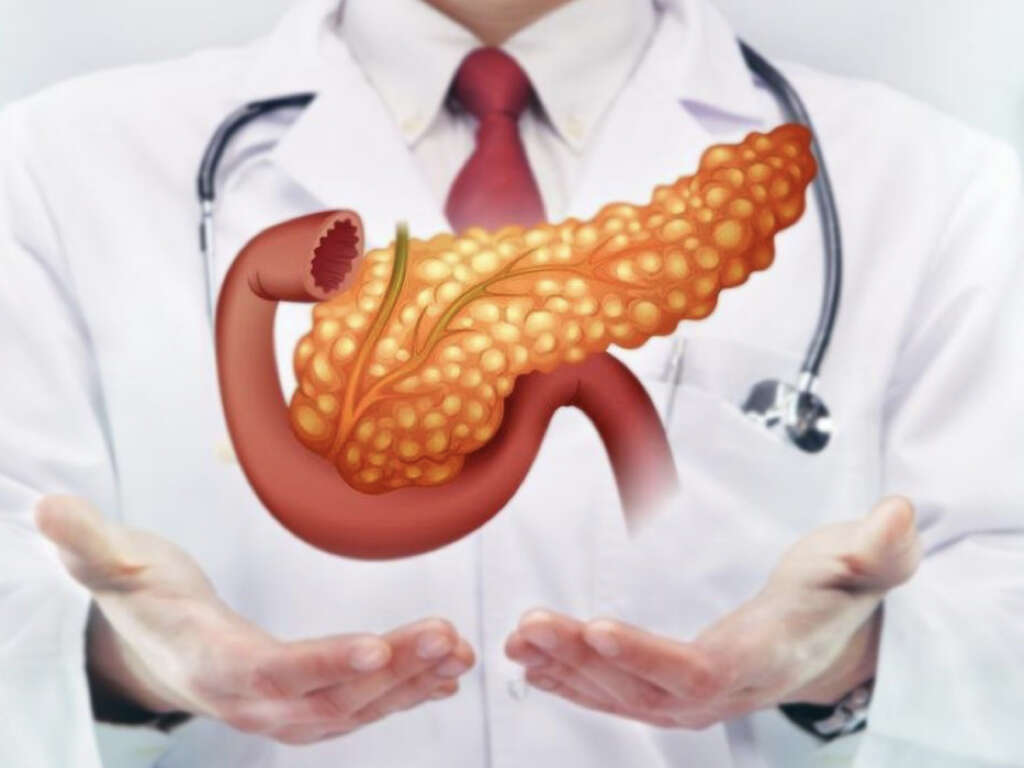
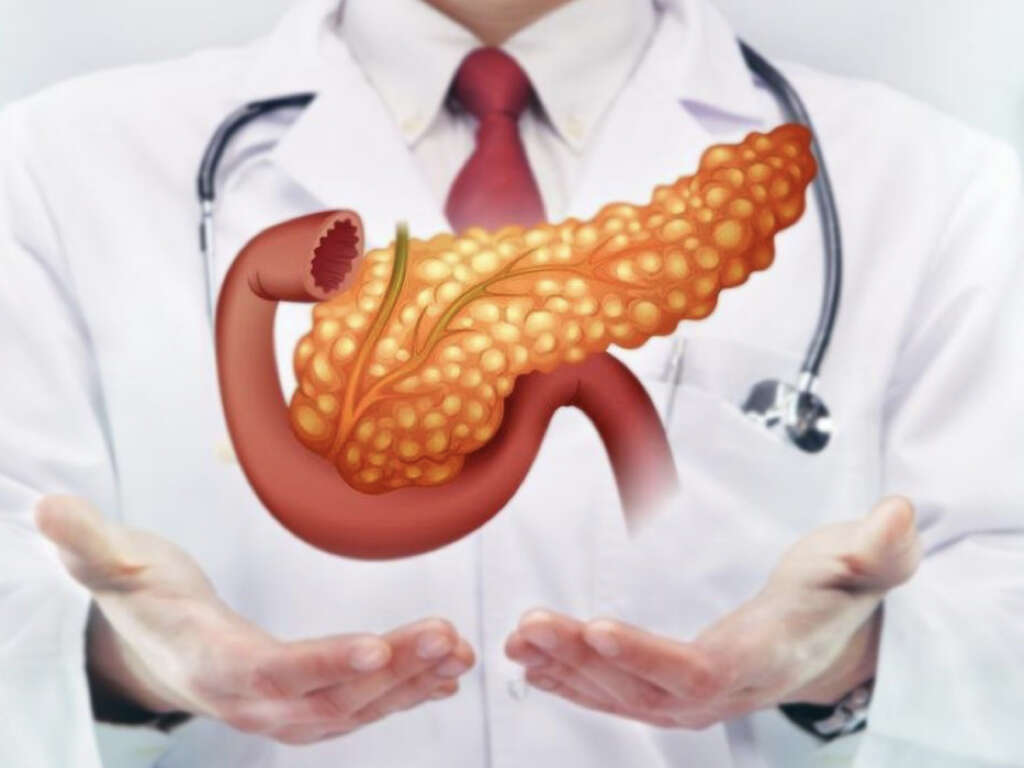
Pancreatitis refers to a condition where the pancreas is inflamed. The pancreas is an organ that functions to produce digestive enzymes and hormones. It can be found behind the stomach. Pancreatitis can be divided into acute and chronic pancreatitis. The inflammation in the pancreas occurs when the pancreatic enzymes autodigest the gland.
In acute pancreatitis, the pancreas is able to heal without any morphologic changes or impairment of function. When the pancreatitis recurs intermittently and gradually contributes to the morphologic and functional loss of the pancreas, this is known as chronic pancreatitis. It is important for healthcare providers to recognize patients with pancreatitis to achieve the best outcomes for the patients. Both acute and chronic pancreatitis may present with acute clinical findings. Management of the disease will depend on the severity of the condition.
1. Normal Function of the Pancreas
Located in the upper abdomen behind the stomach, the pancreas is responsible for the production of insulin, and the manufacturing and secretion of enzymes for the digestion of fat, protein, and carbohydrates. Despite only weighing 0.1% of the body’s weight, it has a high protein producing capacity. The enzymes are produced by the acinar cells and packaged into vesicles known as zymogens. These are then released into the pancreatic duct and secreted into the small intestine. After the food has been digested, a feedback mechanism limits further pancreatic enzyme activation.
2. Pathogenesis of Pancreatitis
Acute pancreatitis is thought to occur when the factors maintaining cellular homeostasis (tendency to equilibrium) are imbalanced. It may be precipitated by events that damage the acinar cell or affect the zymogen granule secretion. This can be seen as a side effect of certain drugs, alcohol use, and gallstones.
Despite being unclear regarding the exact cause of acute pancreatitis, experts believe that it could be caused by both intracellular and extracellular factors. In chronic pancreatitis, there is fibrogenesis in the pancreas due to a response to injury.

3. Causes
In acute pancreatitis, the most common causes are biliary stone disease and chronic alcohol consumption. The cause is unknown in 10% to 30% of cases. In biliary stone disease, the gallstone lodges at the opening in the intestinal sphincter of Oddi and blocks the secretion of the digestive enzymes.
It has been estimated that at least 35% of acute pancreatitis cases are due to alcohol use as alcohol causes accumulation, activation, and premature release of digestive enzymes. Since alcohol increases the permeability of the ducts, this allows the enzymes to cause pancreatic damage. This disease is usually seen in individuals who have a habit of alcohol consumption of more than 5 to 15 years. Other potential causes of pancreatitis include endoscopic retrograde cholangiopancreatography (ERCP), side effects of drugs, trauma, hereditary pancreatitis, infection, developmental abnormalities of the pancreas, and hypercalcemia (excessive calcium in blood).

4. Statistics
In the United States, it has been estimated that acute pancreatitis has an incidence of 40 to 50 cases per 100,000 individuals annually, and alcoholic pancreatitis is most common. Globally, the incidence ranges from 5 to 80 per 100,000 individuals.
The highest incidence is thought to be in Finland and the United States. In Europe, pancreatitis is more commonly caused by gallstones.

5. Signs and Symptoms
One of the main characteristics for acute pancreatitis is abdominal pain that can be described as boring, steady, and dull. The pain usually starts suddenly and gradually increases in severity until there is a constant ache. It is usually located in the epigastric region (middle upper abdomen) but may present more to the left or right side depending on the part of the pancreas affected.
In 50% of cases, the pain tends to radiate straight to the back. Other associated symptoms often present are loss of appetite, nausea, vomiting, fever, tachycardia, abdominal distension, and diarrhea. The pain is often relieved temporarily when the patient sits up and bends forward. A small number of patients may experience jaundice and breathlessness.

6. Diagnosis
Diagnosis is crucial for patients with acute pancreatitis. Once acute pancreatitis is suspected, laboratory tests can be helpful to determine the cause and check for complications.
This includes serum amylase, lipase, liver enzymes, serum electrolytes, blood urea nitrogen (BUN), creatinine, triglycerides, cholesterol, glucose, complete blood count, hematocrit, and C-reactive protein. Despite unnecessary for pancreatitis, diagnostic imaging can help provide morphologic confirmation of the diagnosis. Genetic testing can also be performed for those suspected for mutations associated with acute pancreatitis.

7. Treatment and Management
Patients with acute pancreatitis are kept nil per oral (NPO). This means that no foods of fluids are allowed orally while intravenous fluids will be provided. Prompt intravenous fluids will be needed in the first 24 hours as patients tend to lose fluids during this time. Analgesics will be given for pain relief. In moderate to severe pancreatitis, nasojejunal feedings should be started during admission.
When the caloric needs are not met, total parenteral nutrition (TPN) may be required. Antibiotics should be used when there is infected pancreatic necrosis. Routine antibiotics are not recommended. Surgical intervention may be necessary in some cases. An important part of management includes cessation of tobacco and alcohol use especially in those with chronic pancreatitis.

8. Complications
Complications of pancreatitis include acute fluid collections that generally regress spontaneously. An acute pseudocyst may develop after 4 or more weeks. One common complication is intraabdominal infection that is usually seen in the first to third week.
This can occur when the pancreatic necrosis or fluid collections become infected and negatively impact the prognosis. During week 3 to 6, an abscess may also develop. In most cases, the bacteria causing the infection is due to intestinal bacteria such as pseudomonas, Escherichia coli, Klebsiella, Staphylococcus, Streptococcus, Proteus, Enterobacter, and other anaerobic organisms. Other possible complications include hemorrhage, common bile duct obstruction, leaking pancreatic pseudocyst, or internal pancreatic fistula.

9. Prognosis
In acute pancreatitis, the mortality is thought to be 10% to 15%. However, pancreatitis caused by biliary tract disease tends to have a higher mortality compared to alcoholic pancreatitis. In about 20% of cases, patients present with more severe disease with a higher mortality rate of about 30%.
During the first week of illness, when deaths occur, it is usually due to multiorgan system failure. After the first week, infection also becomes a significant issue. Other issues that increase the mortality rate are acute renal failure, acute respiratory distress syndrome, hemorrhage, cardiac depression, and hypotensive shock. It is important for doctors to identify patients in the greatest need of medical treatment. In chronic pancreatitis, the overall survival rate is estimated to be 70% at 10 years and 45% at 20 years.

10. Patient Education
Patients with pancreatitis should be made aware of what they can do to prevent future episodes. Alcohol binging should be avoided. Other risk factors should also be taken into account. This includes having a healthy diet (by avoiding fatty meals). Furthermore, during the first few days after acute pancreatitis, bowel rest is required.
This means that the patient is not allowed any food or liquid by mouth and the fluids or nutrition needed will be provided intravenously. This gives the pancreas time to recover. In chronic pancreatitis, patients are advised to eat small frequent meals that are low in fat. When a flare up occurs, bowel rest is recommended for about a day but oral fluids are allowed. If the symptoms do not resolve, patients are advised to seek medical care.