What Is Esotropia?
Esotropia is a condition where one or both of the eyes are misaligned and turn inward. It is a form of strabismus (condition where the eyes are not aligned when looking at one object). Esotropia can be present intermittently or constantly to give the individual a “cross-eyed” appearance.
Esotropia is the opposite of exotropia (misalignment to turn outward). It can result in a condition known as amblyopia. Amblyopia, also known as lazy eye, is a condition where there is reduction of vision that cannot be resolved through contact lenses or eye glasses. In esotropia, which causes double vision, the brain suppresses or ignores the image from the affected eye. Left untreated, this results in amblyopia.
1. Accommodative Esotropia
Accommodative esotropia refers to esotropia that occurs due to efforts of accommodation. Accommodation is the eye’s ability to focus on objects of different distance. Accommodative esotropia is often seen in individuals with hyperopia (farsightedness-unable to see close objects unless held further away). The chances of accommodative esotropia occurring may correlate with the amount of hyperopia present. A large degree of hyperopia means no clear vision can be produced with accommodation. When the degree is small enough for accommodation but large enough to disrupt binocular control, it will result in esotropia. There is no racial or gender predilection for accommodative esotropia. If present, the condition is usually noticeable by the age of 2 years.

2. Infantile Esotropia
Infantile esotropia refers to the inward deviation of the eyes before 6 months of age. A frequent consequence of infantile esotropia is amblyopia. The exact cause is still unclear and, therefore, an effective treatment plan is still unavailable. Infantile esotropia is a constant esotropia and often associated with ocular conditions such as dissociated vertical deviation, oblique muscle overactions, defective abduction, and manifest latent nystagmus.
This type of esotropia accounts for 28 to 54% of all esotropias. Based on a population study from 1965 to 1994, the birth prevalence is estimated to be 25 per 10,000 births. It affects 1% of full-term healthy infants and a higher percentage in those with prematurity complications. It may also be associated with higher prevalence of ocular, craniofacial, and neurologic anomalies.

3. Acquired Esotropia
Acquired esotropia refers to esotropia that occurs after infancy and does not always respond to farsighted glasses. It is a category on its own as it does not fit into the categories of accommodative esotropia or congenital esotropia. Although this type of esotropia may be found in those aged 1 to 8 years old, it generally develops in those 2 to 5 years old. More studies are required to help determine the cause of acquired esotropia.
Experts have agreed that some cases may be due to a primary motor anomaly while other cases are due to a primary sensory anomaly. Globally, of all children diagnosed with esotropia, 10.4% have been found to have acquired esotropia. The angle of deviation of the affected eye is usually smaller and surgery is more likely to be successful compared to patients with congenital esotropia.

4. Patient History
Since most patients are nonverbal or very young, guardians or parents may notice that there is an upward or inward deviation of the eye compared to the other. Verbally communicative patients may complain of seeing a single blurry image or double image where one is blurry and the other clear. There may be positive family history of eye conditions such as strabismus.
The age of onset of esotropia should be noted. Guardians and parents who are unsure may refer to photographs of the infant to determine if the condition was present before or after 6 months. In infantile esotropia, risk factors should be elicited. These include complications during pregnancy, prematurity, use of systemic medications, and use of supplemental oxygen.

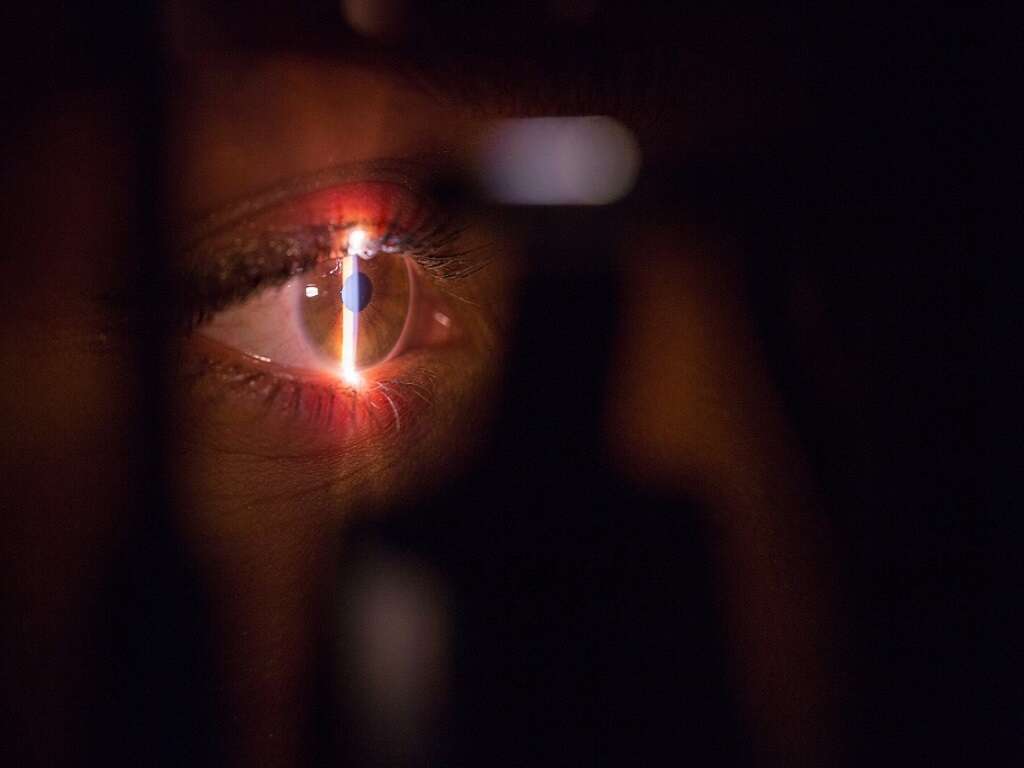
5. Physical Examination
In accommodative esotropia, examination of visual acuity usually reveals hyperopia. Visual acuity can be measured subjectively using methods such as Allen cards, preferential looking, visual evoked potentials, tumbling Es, and Snellen’s chart.
The stereoacuity (depth perception examination using LANG test, TNO test, Randot stereogram, or polarized glasses), eye movements, and the angle of deviation should be examined. The accommodative convergence/accommodation (AC/A) ratio can also be measured. The AC/A ratio should be normal in pure accommodative esotropia and true accommodative esotropia. A complete examination of the eye to assess the lens, anterior chamber, cornea, and fundus should also be performed.
6. Causes
Some possible causes of acquired esotropia are: Arnold-Chiari malformation, being farsighted and not wearing glasses, heredity, neurologic abnormalities, pregnancy and delivery abnormalities, and more. While the exact cause of infantile esotropia is still unclear, experts strongly believe that there is a genetic component.
Several studies have attempted to establish a genetic causation for infantile esotropia. in 1986, it was reported that a patient with severe strabismus had two siblings with infantile esotropia. There are also large studies showing that about 20% to 30% of children with a parent with strabismus will eventually develop strabismus.

7. Investigations for Acquired Esotropia
For acquired esotropia, if there is an absence of expected findings or presence of atypical features, neuroimaging studies should be considered. A computed tomography (CT) scan of the brain can be helpful to rule out diseases in the brain and head area. There are several factors that should prompt clinicians to perform brain imaging. These are the recurrence of acquired esotropia, presence of neurological signs, and older age at onset (more than 6 years).
CT scans of the orbits (eye socket) can also be performed to assess the presence of orbital mass, entrapment of the eye muscles, and possible fractures. X-rays and CT scans can be performed for the chest, neck, and abdomen to determine if there is any malignancy contributing to esotropia.
8. Medical Care
In accommodative esotropia, prescription glasses to correct the hyperopia is usually adequate treatment in 75% of cases. In cases where amblyopia is present, occlusive therapy by patching the normal eye is recommended. Medical care for acquired esotropia depends on the underlying cause. The goal is to optimize the vision and to obtain an acceptable appearance for the alignment of the eyes.
Depending on the patient, treatment options include eye glasses, increasing lens power, using prisms to eliminate double vision, vision therapy, and treatment of amblyopia. In infantile esotropia, medical care involves corrective lenses, occlusion therapy (if amblyopia is present), and injection of botulinum toxin into the medial rectus muscle.

9. Surgical Care
Surgical care may be necessary, especially when the condition is not responsive to optical treatment (eye glasses). In cases where treatment is delayed, surgery is often needed. The surgery involves removing or weakening the eye muscle that pulls the eye inward.
If amblyopia is present, surgery can be performed on the eye with amblyopia by weakening the medial rectus muscle (that pulls the eye inward), and strengthening the lateral rectus muscle (that pulls the eye outward). In acquired esotropia, surgery is recommended when the angle of deviation is great. Infantile esotropia generally has large angles of deviation and requires surgery. Surgery for the pediatric population is performed under general anesthesia.

10. Follow-Up and Prognosis
Those who are being treated for amblyopia should have a follow-up visit at 1 to 4-month intervals depending on the patient’s age. Regular follow-up is recommended to monitor the alignment of the eyes. If the strabismus and amblyopia are not treated before 4 to 6 years of age, permanent vision loss may occur. Early treatment of amblyopia improves the prognosis for the patient as it increases the likelihood of improved vision.
When glasses are worn faithfully, many patients with accommodative esotropia can maintain straight eyes without the need of glasses in their teenage years. In infantile esotropia, the infant is usually seen 3 to 14 days post surgery. Antibiotic and steroid ointment may be prescribed after surgery. Possible complications of surgery include infection, overcorrection or undercorrection, and conjunctival scarring.