What Is Dysautonomia?
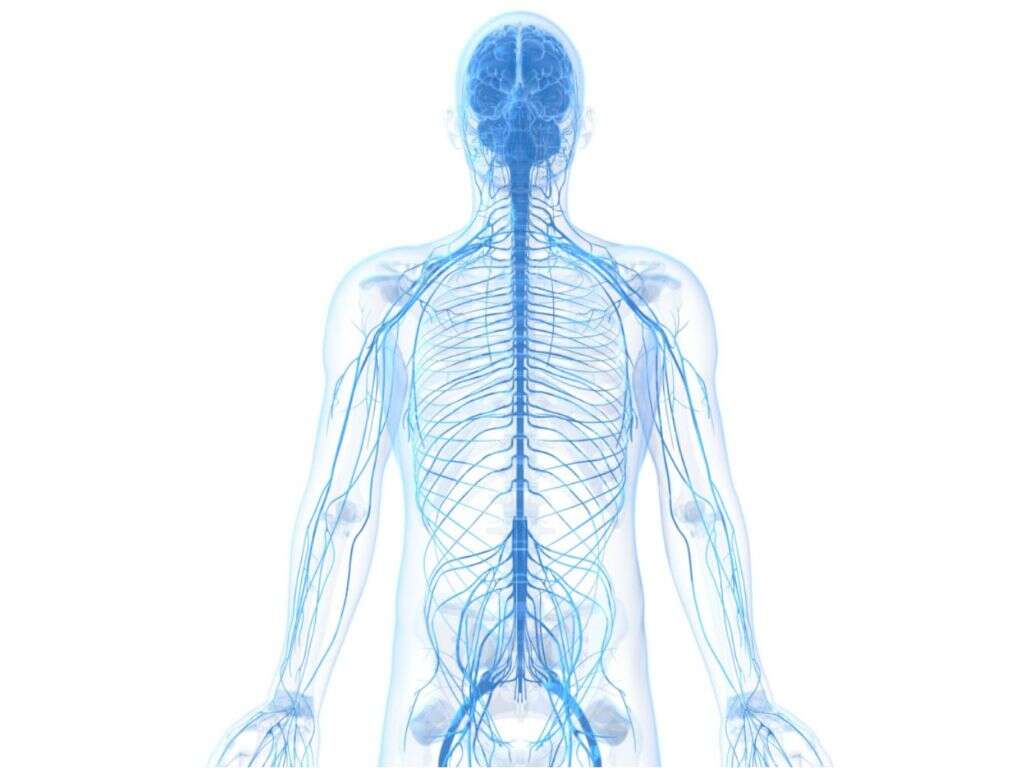
Our autonomic nervous system is responsible for helping to ensure the inner workings of our bodies are operating as they should be. This means things like regulating our heart beat, our breathing, our blood pressure, our digestion, and so on. These are all things that we don’t have to actively think about in order for them to operate.
If something was to affect this system, then it can have a negative impact on the functioning of our bodies. In some instances, it can be very dangerous and it can bring the patient’s life to a premature end. Here we look at the condition in close detail, and the impact it can have on people’s lives.

1. Dysautonomia?
Dysautonomia is a blanket term for conditions that affect our autonomic nervous system. Dysautonomia is a relatively common condition, and around 70 million people are affected by it worldwide. The severity of the symptoms can range considerably, and it can be very dangerous in some cases.
It can also affect people of all ages and from all walks of life. The condition is not well understood and will often not be diagnosed. In addition to health risks, the condition can have a considerable negative impact on the patient’s quality of life. There are numerous different types, and numerous potential causes.
2. Causes
When dysautonomia happens, it is often down to another medical condition. These conditions are sometimes caused by an accident or a medical condition that damages the body. They can also be inherited, meaning the patient is born with the condition. They are also sometimes caused by degenerative diseases.
One potential cause of dysautonomia is Parkinson’s disease, which tends to happen in older people. It can also be caused by rheumatoid arthritis, and multiple sclerosis is another potential cause. Diabetes mellitus is another potential cause, as is celiac disease, which is a type of autoimmune condition that is triggered by gluten.
3. Neurocardiogenic Syncope
There are more than 15 types of dysautonomia, and neurocardiogenic syncope is the most common of them all. Indeed, it affects tens of millions of people around the globe. It takes place when mechanisms that help the blood to return back up the body fail.
This causes blood to pool in the ankles and feet, and it also causes a decrease in the flow of blood to the brain. The lack of blood flowing to the brain causes the patient to faint; a phenomenon that is known as syncope. Most of the time it is only mild and may happen only once or twice. At other times, fainting can be a regular occurrence, and this can have an impact on the patient’s quality of life.

4. Postural Orthostatic Tachycardia Syndrome
Postural orthostatic tachycardia syndrome is a condition that affects up to around 3 million people in America. Only around 20% of people with the condition are male, and it is more likely to affect people that have an existing autoimmune condition like multiple sclerosis.
Typical symptoms of the condition include a fast heart rate, fainting, and lightheadedness. Patients will also often be short of breath, and pains in the chest are also common. Shaking is another potential symptom and patients will also sometimes have an upset stomach. Patients can also become overly sensitive to hot and/or cold, and they can also tire from exercise more easily than usual.

5. Multiple System Atrophy
Multiple system atrophy is often mistaken for Parkinson’s disease to begin with due to the similarity of the symptoms. It affects 2 – 5 people in every 100,000, and most commonly affects people at around 55 years of age. There is little known about the condition, but we do know it is not contagious or hereditary.
The condition causes the gradual breakdown of certain areas of the patient’s brain. This is usually the basal ganglia, the brain stem, and the cerebellum. Symptoms include blood pressure issues, difficulties balancing, speech issues, and poor bladder control. Most people will die from the disease within 10 years of contracting it.

6. Diabetic Autonomic Neuropathy
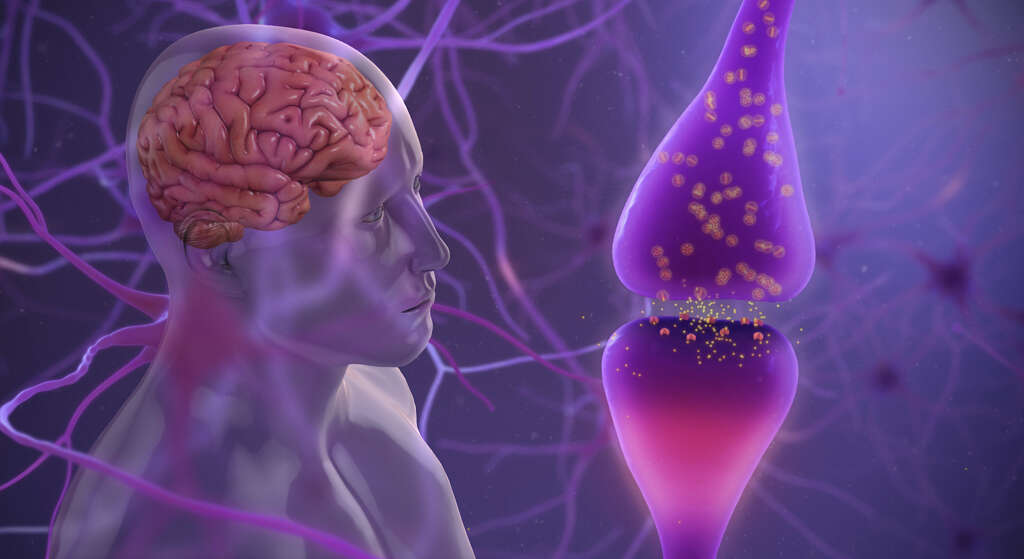
As the name suggests, diabetic autonomic neuropathy affects people that have diabetes, and it will affect around 20% of people with the condition. It affects the nerves that help to control blood sugar levels, control the heart, and regulate blood pressure.
Typical symptoms of the condition including a low blood pressure and a faster than usual heart rate. Patients can also have difficulty passing food through their stomach and some patients will also experience constipation. Problems with sweating are a problem for some people with the condition, and some will experience erectile dysfunction. Neurovascular disorders may also be present, which means functions like control of the artery width is affected.

7. Familial Dysautonomia
Familial dysautonomia affects only around 350 people in the entire world. It is a very serious condition and people with it can expect to have their lives cut considerably shorter, although life expectancy is improving for people with the condition thanks to advancements in treatment.
Familial dysautonomia can result in an autonomic crisis, which means the heart rate and blood pressure will fluctuate rapidly. It can also cause the patient’s digestive system to shut down, and they can also experience changes in their personality. Symptoms will usually show early on in the patient’s life, and it can cause a number of development problems for the patient.

8. Baroreflex Failure
Our blood vessels have what are known as baroreceptors. These are tiny detectors that help to measure the extent to which the walls of our blood vessels are being stretched. This, in turn, helps our nervous system to maintain a healthy blood pressure. Baroreflex failure is a type of dysautonomia that affects the this system, and by extension, their ability to maintain their blood pressure.
This means that the patient’s blood pressure can become too high when exercising or stressed. It can also become too low when the patient is resting. Symptoms of the condition include an abnormal heartbeat, headaches, and excessive sweating.

9. Autonomic Dysreflexia
As mentioned, some cases of dysautonomia can be caused by injuries, and autonomic dysreflexia is an example of this. It usually happens in people that have suffered injuries to the spinal cord. It occurs when there is an unresolved problem that someone with a spinal cord injury is unable to identify such as urinary tract infections, severe constipation, and fractures. It tends to affect the body below where the injury took place.
The injury means that messages cannot make it to the brain, and spikes in blood pressure levels can result. This leads to symptoms like a red face, blocked nose, nausea, slow pulse, and headaches. Patients will also often experience clammy skin and goosebumps around the area where the injury occurred.

10. Treatment
Treatment for dysautonomias depends largely on the specific type. There is no cure for the condition, but the patient’s symptoms can often be treated. In some cases, the patient will be encouraged to work on their physical conditioning to give them physical strength that will help compensate.
Patients will also need to be treated for symptoms they may have, including for conditions with the heart and blood pressure, for example. In many cases, the patient will also be given counselling to help them manage their symptoms better. While some dysautonomias will be deadly, some can be treated to help give the patient a reasonable standard of living.