What Is Anhidrosis?
Anhidrosis or hypohidrosis refers to the condition where there is diminished or absent sweating despite presence of appropriate stimuli. In anhidrosis, there is complete absence of sweating while in hypohidrosis, there is less sweating compared to a normal individual.
Anhidrosis often leads several consequences as it means that the body is unable to sweat like normal individuals. This means that the body is unable to cool itself. Anhidrosis or hypohidrosis is in contrast with hyperhidosis, which is excessive sweating. Hyperhidrosis is usually a benign condition that causes mainly social consequences.

1. Causes of Anhidrosis or Hypohidrosis
Some of the causes of anhidrosis or hypohidrosis include the side effects of medications such as anticholinergic agents, carbonic anhydrase inhibitors, tricyclic antidepressants, and botulinum toxin. It can also be caused by radiation, burns, scars, sores, surgery, and tumors. Some skin conditions that can cause this issue include systemic sclerosis, graft versus host disease, Sjogren syndrome, Fabry disease, psoriasis and more. Other conditions that can be possible causes are diabetes mellitus, Horner’s syndrome, amyloidosis, alcoholism, encephalitis, cervical myelopathy, dementia with Lewy bodies, and multiple sclerosis.

2. Signs and Symptoms
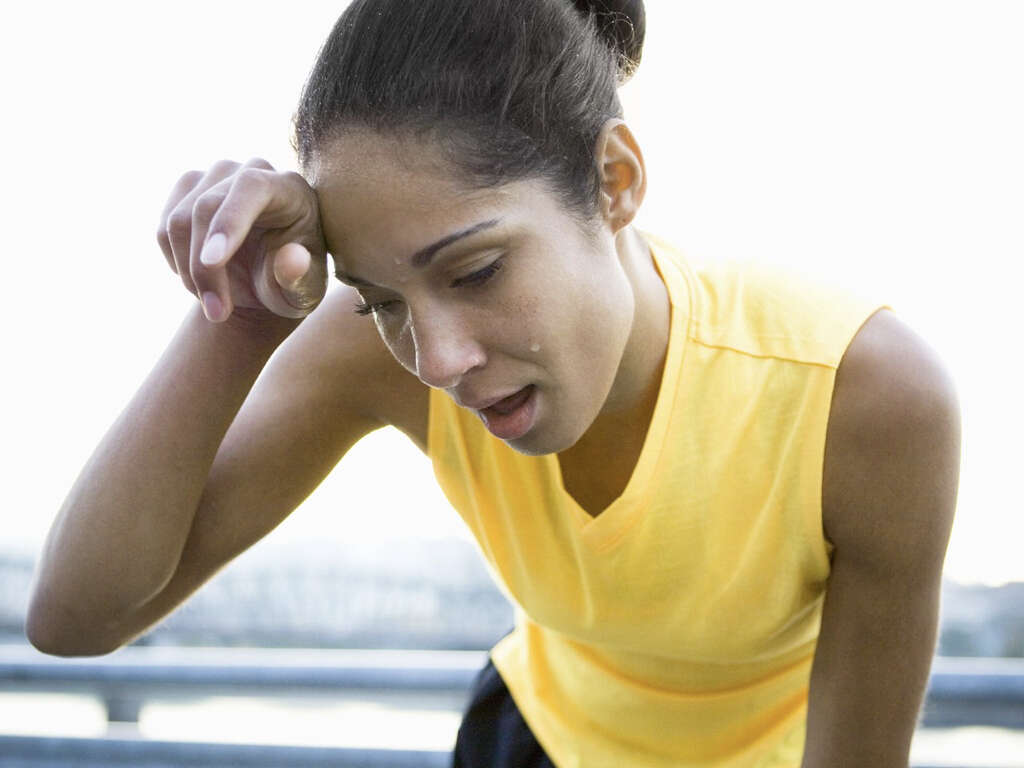
Some of the signs and symptoms of anhidrosis or hypohidrosis are flushing, feeling hot, dizziness, little to no perspiration, muscle cramps, and weakness. The lack of sweat can be generalized, in scattered patches, or only occurring in a single area. This causes some areas to perspire more as a compensation mechanism.
It is possible for the affected individual to sweat profusely at one part of the body while very little or none at all at another. Since anhidrosis or hypohidrosis that affects a large portion of the body prevents the body to cool itself, it is best to avoid hard physical labor, vigorous exercise, and hot weather as it can cause heat exhaustion, heat cramps, or heatstroke.

3. Seeking Medical Care
Individuals who notice that they barely sweat despite the proper stimulus, such as hot weather or strenuous physical activity, must inform their doctor as they are more likely to experience a heat stroke. When a heat stroke occurs, a neurologic dysfunction causes an elevation of the body temperature, reaching temperatures higher than 40°C (104°F).
This can lead to symptoms of an altered sensorium (i.e. dizziness, confusion, disorientation, agitation, inattention, etc.), headache, nausea, vomiting, difficulty breathing, weakness, redness of the skin, and more. It is important to recognize the signs and symptoms of a heat stroke as it can lead to severe complications such as kidney failure and neurological sequelae (i.e. dementia, cerebellar dysfunction).

4. Patterns of Anhidrosis or Hypohidrosis
In clinical practice, the patterns of hypohidrosis or anhidrosis are global anhidrosis where more than 80% of the body surface is affected. This is often seen in patients with primary autonomic failure, hypothalamic lesion, and chronic idiopathic anhidrosis. In hemianhidrosis, there is incomplete anhidrosis (usually ipsilateral or of the same side of the body) due to lesions of the descending sympathetic pathways (i.e. brainstem or spinal cord). In segmental anhidrosis, there is the involvement of large areas that are asymmetrical, contiguous, with sharply demarcated borders.
Moreover, in distal anhidrosis, there is sweat loss in the distal lower limbs that eventually progresses to affect the fingers and lower anterior abdomen. Finally, focal anhidrosis affects isolated dermatomes (areas of skin that are connected to a single spinal nerve) and small localized areas due to injury, radiation, or surgical incision.

5. Risk Factors
There are several risk factors for anhidrosis and hypohidrosis. These include older age and genetic mutations. Changes to genes can lead to anomalies that result in improper functioning of sweat glands. Many individuals of a family can suffer from hypohidrotic ectodermal dysplasia and are at a high risk of developing hyperthermia (abnormally high body temperature), especially in hot environments.
In diabetics, their disease can also cause sweat gland irregularities due to neurological damage. Certain skin conditions such as psoriasis can affect the sweat glands leading to anhidrosis. Patients with a history of burns and trauma to the skin can also develop anhidrosis or hypohidrosis due to improper healing of the sweat glands.

6. Diagnosis
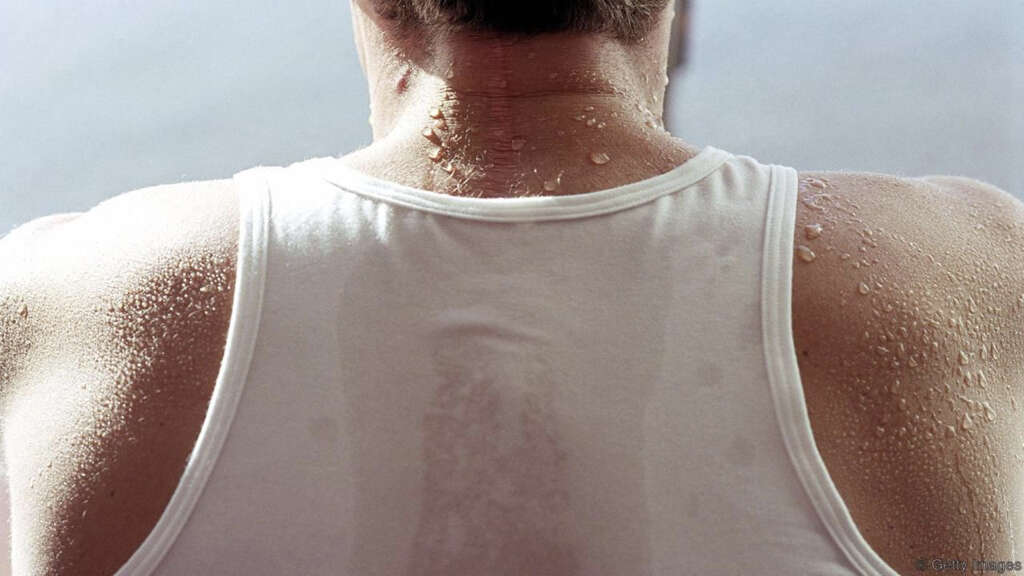
Sweat can be readily visualized by topical indicators such as sodium alizarin sulphate or iodinated starch (minor test). These tests allow a dramatic color change when sweat is present. To evaluate the body’s response to a thermal stimulus, a thermoregulatory sweat test can be performed by inducing sweating using a thermal blanket, exercise, or a hot box.
When there is no change in the color of the substance during testing, there is anhidrosis or hypohidrosis. Further testing may be required to localize the lesions. When the lesion causing the disorder is suspected to be located in the central nervous system, a magnetic resonance imaging (MRI) scan can be used. Skin biopsies can also be useful when hypohidrosis or anhidrosis occur due to a dermatological disorder as it can help reveal the destruction of sweat glands.
7. Management
The options for treatment of anhidrosis and hypohidrosis are limited. Those with this condition should avoid medications that can aggravate the condition, limit activities that raise the core body temperature, and exercise in well-ventilated and sheltered environments. When the primary cause of hypohidrosis or anhidrosis is known, specific treatment can be targeted at the primary pathology.
In autoimmune diseases such as systemic sclerosis and Sjogren syndrome, treatment using immunosuppressants may lead to improvement of the condition. However, treatment for neurological diseases is often irreversible. In these cases, prevention of further damage such as ensuring good glycemic control in diabetics is crucial. Many cases have also been reported to respond to corticosteroids.

8. Complications
The most important complications of hypohidrosis or anhidrosis is due to heat-related issues as the body is unable to cool itself off via sweating. This is especially true among children as their core temperature increases faster compared to adults. Their bodies are also less efficient in releasing heat. Some of the complications include heat cramps where the affected person experiences muscle spasms or pain.
Heat exhaustion can lead to tachycardia, nausea, and weakness. It is a medical emergency. As previously mentioned, another complication that can occur is heatstroke where the body temperature increases leading to loss of consciousness. In all these complications, the affected individual should be moved to the shade, supplemental oxygen provided, and intravenous fluids administered.
9. Patient Education
To prevent complications of hypohidrosis or anhidrosis, patients can try to stay indoors especially on hotter days. On warm days, it can make a significant difference by wearing light and loose clothing. Since sweating may not be an option for some, a spray bottle containing water to replace the sweating mechanism can help to prevent symptoms. Also, learning the signs and symptoms of complications and to seek help when necessary is crucial.
Friends and family members should also be educated on the signs and symptoms of heat cramps, exhaustion, and heat stroke so they know when to call emergency services.

10. What to expect from your doctor
Remember to prepare for certain questions your physician might ask about your symptoms. This will allow you to make the most of your time in the appointment. The doctor will probably inquire about the first time you noticed that you were not sweating, the specific parts of your body that don’t perspire, and if there are others in your family with similar symptoms.
Furthermore, the doctor might also ask if you have any accompanying symptoms if anything seems to improve them or make them worse. Before an appointment, it is helpful to write down any possible questions for your physician and make a list of all the medications and supplements you are taking.