What Are the Signs of Lupus?
Systemic lupus erythematosus, known as SLE or lupus, is an autoimmune disorder. This means that the immune system of someone with lupus mistakenly attacks the person’s own cells as if they were foreign objects. Scientists are uncertain what causes the disease, but it appears to have a genetic component that is activated by environmental factors including ultraviolet light, viral infections, and exposure to certain particulate matter in the air.
Lupus is notoriously hard to diagnose, in part because different individuals can exhibit different symptoms, and because the symptoms can abate during times of remission. The average lupus patient spends six years waiting for a definitive diagnosis. Doctors use a series of laboratory tests to confirm the condition, but there are 10 common Signs that give early clues to the disease’s presence.
1. Skin Rashes
The quintessential lupus symptom is a butterfly-shaped rash across the nose and both cheeks. Lupus means “wolf” in Latin, and the disease is named after the appearance of this symptom, which a doctor in the 1200s thought resembled either the bite of a wolf or perhaps the silhouette of a wolf’s face. The word erythematosus was added to the name in the 1800s, after the Greek word erythema which means “blush.”
Lupus-related rashes are not limited to the face, and distinctive round sores on the arms and legs also are common. When near the hairline or on the head, these lesions can damage hair follicles and cause hair to fall out or become brittle, giving the appearance of what is sometimes nicknamed “lupus hair.” These skin rashes often occur or worsen after sun exposure.

2. Discolored Extremities
Fingers and toes of people who suffer from lupus can periodically turn white, blue, or purple. This disturbing condition is known as Raynaud’s phenomenon and usually occurs in response to cold weather or emotional stress. It also can be triggered by certain decongestant medications, exposure to cigarette smoke, or by holding electronic devices that vibrate, such as electric drills or hand mixers.
Physiologically, the discoloration is caused by an inflammatory narrowing of small vessels that supply blood to the skin. There is often a numb or pins-and-needles sensation accompanying it, and some report the experience as being painful. Other extremities like the nose, ears, or chin also can be affected. When the skin is warmed or the external trigger removed, affected areas can turn red in response to restored blood flow and increased temperature.

3. Abnormal Urine
The urine of people with lupus can look red, pink, or brown and can have a frothy texture. The color change occurs due to blood in the urine, or hematuria, which can occur when inflammation causes the glomeruli, or vessels of the kidneys, to narrow. Immune cells can attack the glomeruli themselves and cause scarring, which further allows blood to enter the urine. Similarly, in a condition known as proteinuria, the vessels allow too much protein to be excreted and cause the urine to look foamy.
Other less obvious signs that the kidneys are under attack are high blood pressure and fluid retention around the ankles and waist. Sometimes people feel excessively thirsty or hungry or have to urinate frequently. Doctors can inspect urine under a microscope for the presence of cell casts, which are tiny pieces of blood or kidney cells, or macromolecules of protein and fat. Tests of glomerular filtration rate are sometimes performed, or in extreme cases, a piece of the kidney can be biopsied.

4. Muscle Pain
Unfortunately, people suffering from lupus must cope with chronic muscle pain. Generalized pain in the muscles, known as myalgia, is caused by inflammation in other parts of the body. This phenomenon is similar to the achy feeling that accompanies influenza and serves as an indicator that the body as a whole is under attack. It can give people a general feeling of malaise and fatigue.
Myalgia can be contrasted with myositis, which is inflammation of a specific muscle. All skeletal muscles are at risk, but muscle groups commonly affected are those of the shoulders and neck, thighs and pelvis, and upper arms. In extreme cases, patients are unable to perform simple tasks such as getting out of bed or raising their arms above their heads. Extreme pain and lack of mobility can cause loss of muscle mass, which further exacerbates the problem.

5. Joint and Tendon Pain
Joints and ligaments connect bone to bone, and tendons connect bone to muscle. Pain in any of these structures, especially pain that comes and goes, is a sign of lupus. Lupus arthritis causes inflammation in joints of the limbs, causing them to swell and become stiff, painful, and warm to the touch. Pain is generally more severe in the morning than at night and affects both sides of the body equally.
Pain in a tendon or its associated bursa (sacs of lubricating synovial fluid) is known as tendinitis or bursitis, respectively, and can be caused by damage to a joint. Carpal tunnel syndrome, also caused by inflammation, can be a side effect that results in numbness and tingling of the hands.
6. Brain Fog
Lack of concentration, headaches, and memory loss are experienced by lupus patients so commonly that they are collectively given the nickname of “lupus fog.” These symptoms can be so subtle that they go unnoticed for years or are mistakenly attributed to other causes such as stress, lack of sleep, or the aging process.
Some patients have more extreme forms of cognitive impairment, including seizures, extreme mood swings, or even psychotic episodes. These incidents are the brain’s response to inflammation attacking the central nervous system and can be chronic or appear and disappear periodically. They do not cause permanent brain damage but can be disruptive to a person’s life.

7. Mouth Ulcers
Lupus-related mouth ulcers differ from canker or cold sores. They resemble canker sores in that they are red in the middle and white around the perimeter but also have white streaks that radiate out from the center. Lupus mouth sores are occasionally on the bottom lip but most often occur on the roof of the mouth or in the nose. A major difference from cold sores is that the sores are usually painless. Another type of mouth lesions are white patches of rough, keratinized skin on the inside of the cheek.
Sometimes people develop sores in the corners of the mouth (angular cheilitis) due to a condition associated with lupus called Sjögren’s syndrome, or xerostomia, that causes the body to produce less saliva than normal. Other complications associated with lack of saliva are discomfort in swallowing and talking, reduced sense of taste, recurrent oral yeast infections, dental cavities, and a cracked and bumpy tongue. Sjögren’s syndrome also affects tear-producing glands, resulting in dry eyes.

8. Trouble Breathing
Another sign of lupus is a stabbing pain in the chest when you laugh, sneeze, or sometimes simply breathe. This condition is called pleurisy and is caused by inflammation of the outer lining (pleura) of the lungs. Sometimes a liquid can build up between the pleura and the lungs, causing what is known as a pleural effusion, which also causes chest pain and shortness of breath. When symptoms include fever and excessive coughing, it can be a sign that tissues inside the lungs may be infected by microorganisms.
Over the long term, breathing problems can lead to scar tissue forming in the lungs, which can further reduce their ability to function. This situation leaves many patients with what is known as chronic diffuse interstitial lung disease, the symptoms of which are coughing, experiencing chest pain, and feeling short of breath after physical activity. Lung disease puts them at risk for pulmonary embolism, a life-threatening situation in which a blood clot forms in the lungs.
9. Gastrointestinal Distress
Nausea, vomiting, constipation, and diarrhea can be signs of lupus-related irritable bowel syndrome. In a related condition called ascites, the lining of the abdominal cavity, the peritoneum, can become inflamed, causing fluid to accumulate there. Symptoms of ascites are fever, pain, and tenderness in the abdomen, and the inability to have a bowel movement.
Lupus also causes inflammation in the lining of the esophagus, resulting in chronic acid re-flux, heartburn, and sometimes difficulty swallowing. Blood in the stool can be a sign of lupus-related ulcerative colitis, which is the presence of sores in the lining of the stomach and rectum. Other digestive organs potentially affected by lupus include the gallbladder, pancreas, and liver.

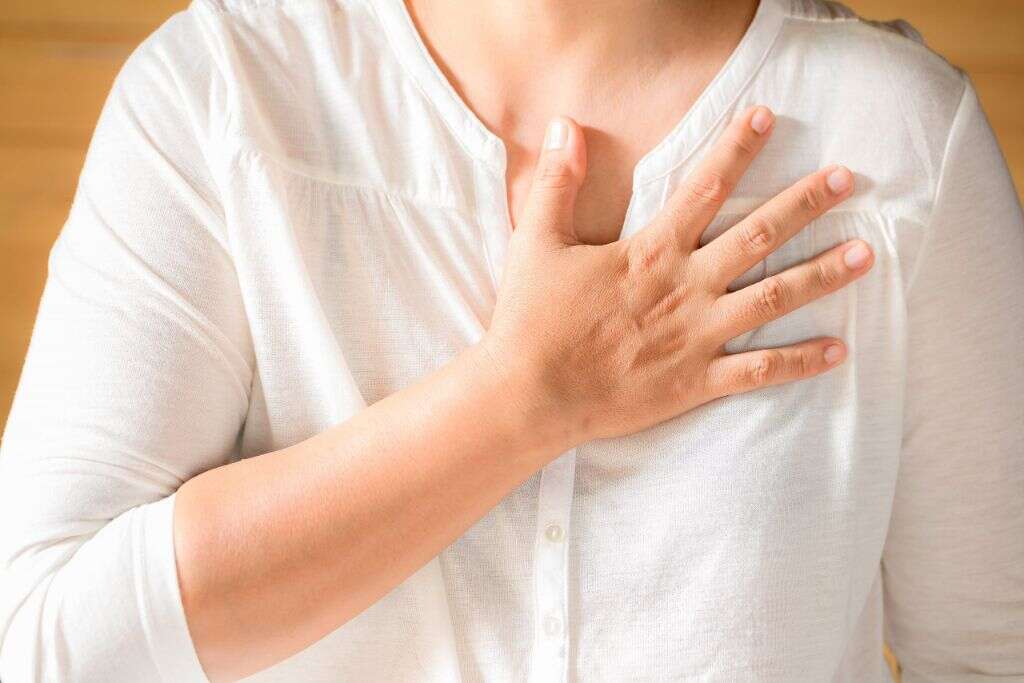
10. Heart Problems
While lupus has no significant effect on life expectancy, heart disease is the leading cause of death in lupus patients, and most will experience some type of problem with the heart during the course of the disease. The outer lining of the heart, the pericardium, can become inflamed and cause pain and shortness of breath. The endocardium, the lining of the inside of the heart, also can be affected, making heart valves thicken or develop growths. The heart muscle itself, the myocardium, can suffer as well, causing rapid heartbeat and pain.
Other cardiovascular conditions caused or worsened by lupus include anemia, thrombosis, atherosclerosis, vasculitis, and angina. Anyone experiencing these signs may want to schedule an appointment with a health care provider. Finding a course of treatment can help improve quality of life and help patients deal with living with lupus.