10 RSD Symptoms (Reflex Sympathetic Dystrophy)
Reflex sympathetic dystrophy, or complex regional pain syndrome, is a condition that is sometimes known as the “suicide disease” because of the severe symptoms and lack of effective treatments. It most commonly affects a portion of the body, usually a limb.
One version of the McGill pain index (a scale that helps individuals describe the intensity and quality of pain) has ranked this condition highest, even above amputation, childbirth, and cancer. This condition may first affect one limb and gradually spread throughout the body. There are two subtypes with type 1 occurring after illness or injury without evidence of nerve damage in the affected limb while type 2 has distinct evidence of a nerve injury.
Reflex sympathetic dystrophy is an uncommon condition with an unclear cause. Treatment is best if started early as it improves prognosis. It often involves medications, occupational therapy, physical therapy, neuromodulation, and psychological treatments.

Symptom #1: Pain
Pain is a distressing feeling that is often caused by damaging stimuli. It can be defined as an unpleasant experience where there is potential tissue damage. Pain is a sensation that motivates the individual to withdraw from damaging stimuli or situations to protect the body and allow it to heal. It also helps learning and teaches the individual to avoid similar experiences in the future.
Pain is one of the first symptoms that limits function. In reflex sympathetic dystrophy, the pain is usually burning in nature and is severe. It is felt in the extremity and can last for many years. It may be worsened by emotional factors and loud noises.

Symptom #2: Swelling
Swelling refers to the temporary abnormal enlargement of the affected body part due to the accumulation of interstitial fluid. It can be localized or generalized. It is generally harmless and is a common reaction to a bruise or inflammation.
Swelling is also considered to be one of the five hallmarks of inflammation along with loss of function, heat, pain, and redness. Swelling can occur as a response to disease, injury, and infection. Swelling is one of the common physical findings for reflex sympathetic dystrophy. It is often more prominent with dependency in early stages of the disease.

Symptom #3: Redness and Warmth
Redness and warmth are cardinal signs of inflammation. Redness and warmth occur due to increased blood flow to the site of inflammation. The redness in reflex sympathetic dystrophy worsens with dependency. The redness usually gives way to cyanosis, pallor, and hyperhidrosis.
The redness is often most noticeable at the proximal interphalangeal joint and metacarpophalangeal joint flexion creases in the early stages of the disease. Inflammation may be reduced using nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen.

Symptom #4: Loss of Function
Loss of function is one of the hallmarks of inflammation. It may occur due to pain that inhibits the affected body part. This is believed to be a protective mechanism as loss of function leads to limited movement allowing the damaged part to heal.
In reflex sympathetic dystrophy, loss of function progresses due to fibrosis and pain in the joints due to chronic inflammation. The loss of function in reflex sympathetic dystrophy is often prominent and can cause negative impacts on the daily activities of the patient.

Symptom #5: Hyperhidrosis
Hyperhidrosis refers to the condition where there is abnormally excessive sweating than those needed for body temperature regulation. It can negatively impact the quality of life from a social, emotional, and psychological perspective. It can be localized or generalized.
Some of the most active regions of perspiration are the feet, hands, facial area, and groin due to the higher number of sweat glands. Localized sweating is known as primary hyperhidrosis while generalized sweating is also known as secondary hyperhidrosis. Hyperhidrosis may occur in reflex sympathetic dystrophy.

Symptom #6: Fainting
Fainting or syncope occurs when there is rapid and sudden loss of muscle strength and consciousness. it occurs as a result of decreased blood flow to the brain. Symptoms include nausea, vomiting, sweating, lightheadedness, loss of consciousness, and pallor. Causes of fainting include orthostatic hypotension, abnormal heart rhythm, pulmonary embolism, and dehydration.
Presyncope occurs when there is not a total loss of muscle strength or consciousness. Presyncope and syncope treatment is similar. Fainting spells may occur in reflex sympathetic dystrophy.

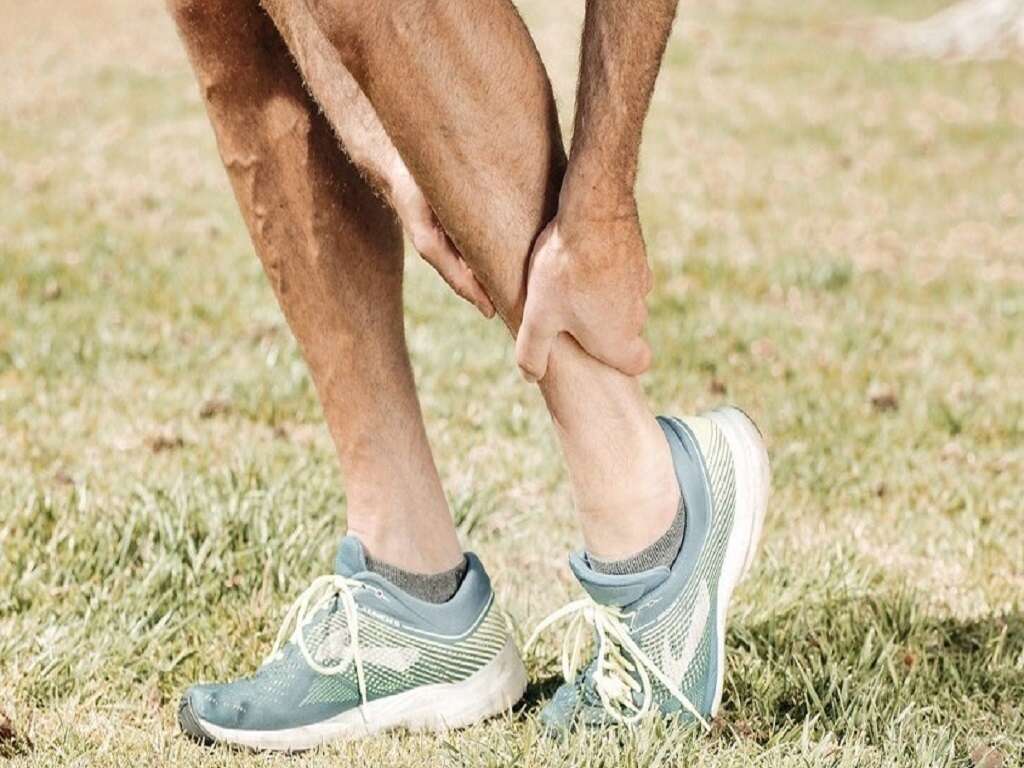
Symptom #7: Stiffness
Joint stiffness usually occurs when there is disease of the joint. It is most commonly seen with joint pain and limited movement. Joint stiffness may occur during different times. For example, in osteoarthritis, joint stiffness is most commonly felt in the morning upon waking up.
In reflex sympathetic dystrophy, joint stiffness is often prominent and can manifest as a claw hand or frozen shoulder. Stiffness is usually more severe than expected and can cause great distress to the affected individual.

Symptom #8: Skin Discoloration
Skin discoloration occurs when the skin changes color compared to normal. In reflex sympathetic dystrophy, discoloration of the skin may occur. The discoloration may differ depending on the different stages of the disease. The skin can appear cyanotic, pale, dusky, or red. It can also lead to skin hypopigmentation.
In the hand, skin discoloration usually starts to appear red over the proximal interphalangeal joint (PIP) or metacarpophalangeal joint (MCP) flexion creases in the early stages of the disease.

Symptom #9: Atrophy
Atrophy refers to the partial or complete wasting of the body. It can lead to diminished muscle size due to reduction in cell, organ, or tissue size. It may be caused by poor nourishment, mutations, poor circulation, excessive cell apoptosis, loss of nerve supply, loss of hormonal support, and lack of exercise.
In reflex sympathetic dystrophy, the subcutaneous tissues and skin begins to atrophy. Other potential causes for atrophy include Charcot-Marie-Tooth disease, Guillain-Barre syndrome, and poliomyelitis.

Symptom #10: Dupuytren’s Contracture
Dupuytren’s contracture refers to the condition where one or more fingers are permanently flexed due to fibrosis of the palmar fascia. It begins as small nodules under the skin of the palm and gradually worsens over time until the fingers can no longer be straightened. The most commonly affected fingers are the ring finger, middle finger, and little finger.
While it does not cause any pain, it can have a negative impact on daily life as it interferes with writing, food, and other activities. Risk factors include liver disease, alcoholism, positive family history, smoking, thyroid issues, epilepsy, and diabetes. Treatment includes steroid injections and physical therapy. Clostridial collagenase injections or surgery may also be beneficial.