What Is Psoriatic Arthritis?
Psoriatic arthritis is a chronic and inflammatory condition that develops in about 5% of patients with psoriasis. Although a link between psoriasis and arthritis was made in the mid-19th century, it was not clinically distinguished from rheumatoid arthritis until the 1960s.
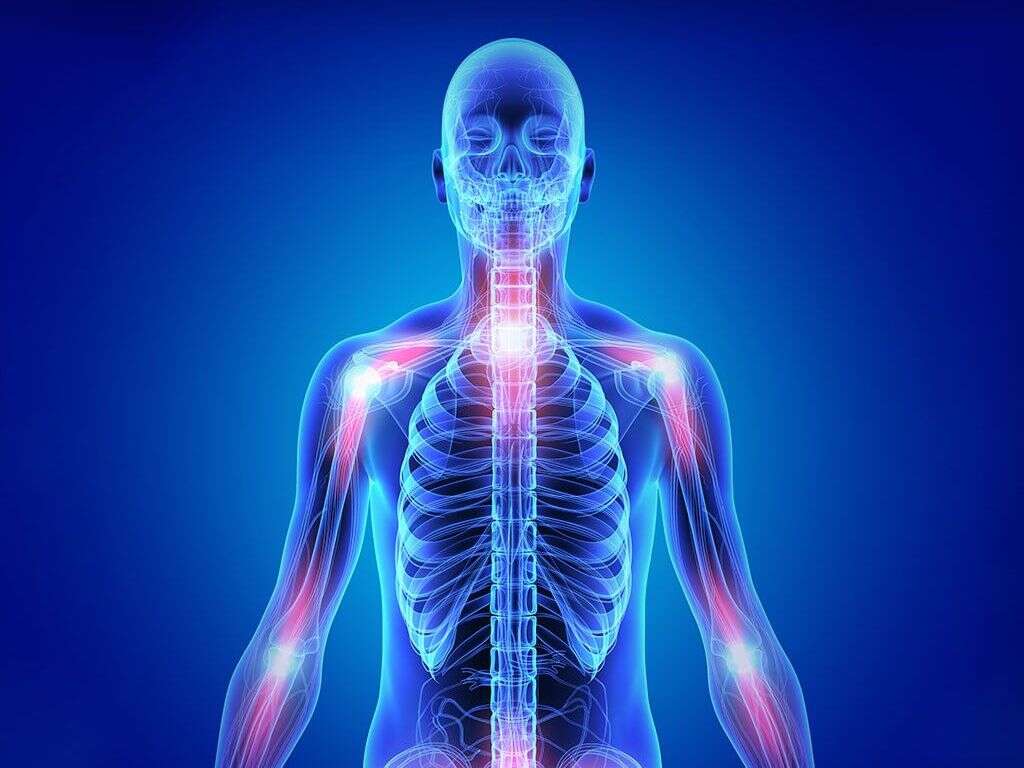
As the name suggests, psoriatic arthritis affects the joints and entheses (connective tissue between bone and ligament or tendon). Psoriatic arthritis may also affect the nails and skin with other associated features such as osteitis, uveitis, and dactylitis. Ninety-five percent of patients with psoriatic arthritis experience peripheral joint disease while axial spine involvement occurs in the other 5%.

1. Mechanism
Although the pathogenesis of psoriatic arthritis is not fully understood, environmental factors, genetics, and immune-mediated inflammation are believed to play a role. Since psoriatic arthritis and psoriasis are interrelated disorders, both disorders have commonalities in the pathogenesis. Genetic factors play an important role in the susceptibility of psoriatic arthritis and psoriasis with an estimated 40% of patients having a positive family history. The recurrence risk ratio has been estimated to be 8 to 10 for psoriasis and 30 to 55 in psoriatic arthritis. The inflammatory process also suggests the involvement of immunological mechanisms where there is an increased level of proinflammatory cytokines such as IL8 and IL6.

2. Statistics
The National Psoriasis Foundation has estimated that psoriatic arthritis affects about 30% of individuals with psoriasis, around 1 million individuals in the United States. However, various studies have reported varying prevalence rates. In a population-based study, there were less than 10% of individuals who had clinically recognized psoriatic arthritis throughout a 30-year duration.
A survey reported a 0.25% prevalence rate of psoriatic arthritis in the general population and 11% prevalence rate in patients with psoriasis. Globally, it is estimated that the average prevalence of psoriatic arthritis is 133 per 100,000 individuals. Among patients with psoriasis, about 1 in 4 patients have psoriatic arthritis. Psoriatic arthritis has been reported to be more common in Caucasians with equal ratio for both genders.

3. Signs and Symptoms
Psoriasis generally begins in 60% to 80% of patients before the onset of psoriatic arthritis. In the residual 15% to 20%, arthritis appears before psoriasis begins. This may occur especially among those with a positive family history of psoriasis. Although most have a gradual onset, about 33% of patients experience acute symptoms. Some of the factors that may increase the risk of psoriatic arthritis include extensive skin involvement and the presence of nail lesions.
Some of the symptoms patients may experience are pain and stiffness in the joints. One important finding in patients with psoriatic arthritis is dactylitis, also known as sausage fingers; however, it is not specific for this condition. It involves the inflammation of the small joints of fingers or toes, causing the swelling of the entire digit. Furthermore, many people with psoriatic arthritis report symptoms that involve the eyes, the skin (scaly and red lesions), the nails (i.e. splinter hemorrhages, detachment from the nail bed, etc.), and nonspecific symptoms (i.e. fatigue).

4. Types of Psoriatic Arthritis
In asymmetrical oligoarticular arthritis, different joints on each side of the body are affected. Moreover, the toes and fingers are usually affected first, possibly resulting in dactylitis. Large joints such as the knee can also be involved.
Another pattern of joint involvement is symmetrical polyarthritis, which is thought to be the most common type of psoriatic arthritis. It develops on both sides of the body, meaning that it will usually involve the contralateral joint, and it may involve many joints at a time. Generally, wrists, hands, feet, and ankles are affected. On the other hand, distal interphalangeal arthropathy is estimated to only occur in 5% to 10% of patients, mostly men. It involves a tiny joint that is located at the tip of the finger, just before the start of the nail. Finally, arthritis mutilans is a rare form of psoriatic arthritis and can be as severe as rheumatoid arthritis. In arthritis mutilans, there is bone loss, and the joint breaks down, resulting in deformities. In about 5% of patients with psoriatic arthritis, there is the involvement of the spine.

5. Juvenile Psoriatic Arthritis
As the name suggests, juvenile psoriatic arthritis (JPA) is seen in 8% to 20% of childhood arthritis. The incidence and prevalence of juvenile psoriatic arthritis are unknown and vary greatly according to the criteria for diagnosis used to obtain the data. The onset of JPA is before 16 years of age and the duration of symptoms is of at least six weeks. Furthermore, to establish a definitive diagnosis, it must be associated with psoriasis in the patient or in a first-degree relative (i.e. parents or siblings), or it can be associated with two of the following findings: dactylitis or specific nail abnormalities. As you might have guessed, the diagnosis of this condition is not easy, especially because the signs and symptoms of JPA can be subtle or atypical in children.
Children that exhibit JPA before five years of age are usually female and present with the involvement of wrists, and joints of the hands and feet (i.e. dactylitis). On the contrary, the presentation in children above this age more closely resembles adult psoriatic arthritis, and it presents in both genders almost equally. Additionally, it will involve the axial skeleton (i.e. inflammation of the sacroiliac joint in the pelvis) and the entheses (the insertions of tendons, ligaments, fascia, or joint capsules into bones).

6. Diagnosis
There are no specific tests to diagnose psoriatic arthritis. Instead, it is based on a combination of clinical and radiological (medical imaging) criteria. Some of the tests that can be helpful to diagnose psoriatic arthritis include erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) levels as they increase when there is inflammation.
Rheumatoid factor and antinuclear antibodies may help to rule out other types of arthritic conditions. Other useful tests include levels of immunoglobulin A (IgA) in the blood and testing of intra-articular fluid (synovial fluid). Furthermore, imaging helps provide radiological features that can distinguish psoriatic arthritis from other forms of arthritis. Generally, X-rays, a computed tomography (CT) scan, a magnetic resonance imaging (MRI) scan, and ultrasonography can be performed.

7. Radiographic Findings
Radiological features generally show mild erosive disease. In psoriatic arthritis, changes in the joints are usually asymmetrical and they are mostly located in the small joints of the feet and hands. Unfortunately, erosive disease may result in the deformation of the joint. In the case of arthritis mutilans, a classic finding on X-ray is the “pencil-in-cup deformity”. Usually, a tiny bone of the finger is eroded into a pencil shape, which turns causes the adjoining bone to acquire a cup shape. Additionally, narrowing of the joint spaces of the finger joints can also be observed.
CT and MRI scans can be useful in detecting early changes in the joints. An MRI may show inflammation in the ligaments and soft tissues around the affected joint. Ultrasonography is used by some to diagnose, predict disease progression, predict prognosis, and monitoring of the disease.

8. Treatment and Management
Treatment of psoriatic arthritis aims to control the inflammation. Some experts have recommended starting disease-modifying antirheumatic drugs (DMARDs) early to delay the progression of disease and deformities. Also, a tailored regimen of physical therapy should begin early in the disease. For those with severe pain or significant deformities, surgery such as a joint replacement may be beneficial.
However, treatment should focus on the relief of symptoms and improving function. For pain relief, nonsteroidal anti-inflammatory drugs (NSAIDs) and glucocorticoids (steroids) may help. Additionally, the injection of glucocorticoids into the joints can help reduce inflammation.

9. Prognosis
Psoriatic arthritis was originally thought to be relatively mild. However, about 40% of cases were found to develop deforming and erosive arthritis. A Canadian study has reported a higher risk of obesity, hypertension, type 2 diabetes, hyperlipidemia, and heart issues in individuals with psoriatic arthritis compared to patients with only psoriasis.
A study in Norway reported that the severity of psoriatic arthritis decreased during pregnancy and increased within 6 months after delivery.

10. Patient Education
Patient education is crucial in psoriatic arthritis as it helps patients to better manage their condition, symptoms, and learn self-treatment strategies. They can also be referred to physical therapists to help them develop an exercise program and educate them regarding the benefits of a tailored program, as overexertion can cause harm to psoriatic arthritis patients. Joint protection is required as part of their therapy.
They should take adequate breaks and pace themselves from activity. Other joint protection methods include using splints on affected joints, learning proper lifting techniques, making use of body mechanics, and incorporating assistive devices into daily routines. Patients and their family members can also be made aware of when to seek medical treatment such as redness, swelling, and pain of the joint.