What Is Osteoarthritis?
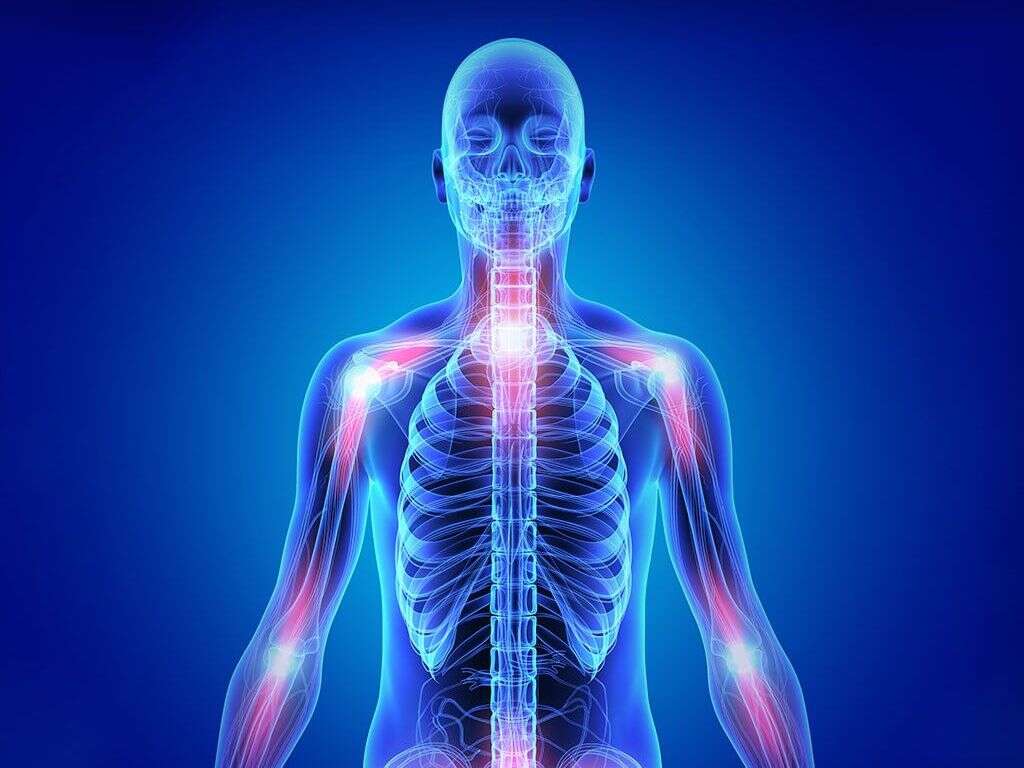
Osteoarthritis is the most common type of joint disease where it results in histopathologic and radiologic changes. It generally affects the weight-bearing joints such as the cervical spine, lumbosacral spine, hips, knees, and feet. Other joints that are commonly affected are the joints in the fingers.
Although once thought to be predominantly caused by excessive wear and tear, there is increasing literature and evidence pointing to the contributions of inflammation and abnormal mechanics. Generally, it can be divided into the primary and secondary forms. Since it is a common condition, it is costly due to visits, medications, therapy, and surgery. There is also indirect costs due to absence from work and decreased productivity.
1. Pathophysiology
In early stages of the disease, osteoarthritis can cause subtle biochemical changes. As the disease progresses, it can cause gross cartilage loss and damage to the joint tissues. In osteoarthritis, the collagen matrix is disorganized and the proteoglycan content in the cartilage decreases. As the collagen fibers break down, the water content increases. Without the proteoglycan’s protective effects, the collagen fibers are susceptible to degradation and results in degeneration.
Inflammation of the joint capsule and synovium can also occur as products from the breakdown are released into the synovial space. In the joint, the ligaments thicken and become fibrotic while the damaged menisci is damaged and worn. Bony growths known as osteophytes or spurs can also form on the joint margins causing more issues.
2. Causes
The daily wear and tear affects the joints (especially the weight bearing joints such as the hip, knee, and ankle). Most experts believe that the degeneration begins in the articular cartilage due to normal load (weight) on an abnormal or damaged joint or excessive load (weight) on a healthy joint.
Some of the risk factors for osteoarthritis include trauma (to the joint), age, obesity, muscle weakness, positive (and significant) family history, low levels of sex hormones, joint infection, repetitive use, previous episode of inflammatory arthritis, bone disorders, diabetes mellitus, history of surgical procedures, congenital joint conditions (such as congenital hip dislocation), and neuropathic disorders (such as tabes dorsalis and syringomyelia).

3. Statistics
In the United States, osteoarthritis affects more than 20 million people. If osteoarthritis is based on the radiographic criteria, more than 50% of those above the age of 65 are affected. Globally, osteoarthritis is the commonest joint disease and its frequency varies in different populations.
Symptoms of osteoarthritis do not generally become significant until the individual is above the age of 50. The prevalence of osteoarthritis increases dramatically among those above the age of 50. This is probably due to the collagen alterations and decrease of proteoglycans due to age. Osteoarthritis is observed to be more common among women compared to men. Female patients are more susceptible to osteoarthritis in the fingers and knee joints. Osteoarthritis has been observed to be more common in Native Americans, African Americans (especially women), and the Chinese.
4. Signs and Symptoms
The main symptoms in osteoarthritis include pain, stiffness, and loss of ability to move. The pain in osteoarthritis is often worsened by long durations of activity and relieved when at rest; however, too much rest can cause pain as well. In the mornings after waking up, stiffness is often worst but gradually resolves after beginning activities.
Movement of the affected joint may also produce a crackling sound known as crepitus. Patients may also complain of joint instability and joint locking. Some patients may experience aggravation of symptoms with high humidity, cold temperature, or drop in barometric pressure. Although it can affect any joint, it most commonly affects weight bearing joints, hands, feet, and spine. Osteoarthritis in smaller joints may result in hard bony enlargements known as Bouchard’s nodes or Heberden’s nodes.

5. Disease Progression
The progression of osteoarthritis can be divided into three stages. At stage 1, the cartilage matrix goes through proteolytic breakdown. Stage 2 involves the erosion and fibrillation of the cartilage surface. This causes the release of collagen fragments and proteoglycan into the synovial fluid.
By stage 3, cartilage breakdown products cause a chronic inflammatory response which then causes further cartilage breakdown. Although there are several systems that are used to grade focal cartilage change, simple descriptions (such as surface, partial or full thickness, subchondral bone change) are usually sufficient and help prevent confusion. Erosive osteoarthritis has been found to have the worst prognosis and causes the most disability with time.
6. Diagnosis
The diagnosis of osteoarthritis can be achieved via a combination of clinical and radiographic evidence. Patients with osteoarthritis do not usually have any specific laboratory abnormalities. Erythrocyte sedimentation rate (ESR) levels and white blood cell (WBC) counts are generally not elevated.
Some cases of erosive inflammatory arthritis may cause slight elevation in these tests. Plain radiographs are the investigation of choice for osteoarthritis as they are cost-effective and easily accessible. Plain radiographs usually show joint-space loss, cyst formation, and subchondral bony sclerosis. A magnetic resonance imaging (MRI) scan can show the characteristics that can be seen on plain x-rays but is generally unnecessary unless there are additional pathology that can be resolved through surgery. Bone scans and arthrocentesis are investigations that can be beneficial for diagnosis.

7. Nonpharmacologic Treatment
Treatment goals are improvement of function and alleviation of pain. Ideally, patients should receive a combination of pharmacologic and nonpharmacologic treatment. Nonpharmacologic interventions are crucial in the treatment of osteoarthritis.
They include patient education, physical therapy, occupational therapy, heat and cold therapy, weight loss, regular exercise routines, and more. A physical therapist and nutritionist can help the patient with developing exercise and dietary routines to help improve function and for weight loss, among other things. Exercise programs such as tai chi have been shown to benefit patients with osteoarthritis. Other nonpharmacological treatments that may help are transcutaneous electrical nerve stimulation, pulsed electromagnetic field therapy, whole body vibration, glucosamine, and chondroitin.
8. Pharmacologic Treatment
Acetaminophen can be used for mild to moderate osteoarthritic pain. For those that do not respond, a nonsteroidal anti-inflammatory drug (NSAID) such as ibuprofen or naproxen sodium can be used. The lowest dose should be given. Patients with highly resistant pain may be given tramadol.
Other medications used for pain include celecoxib and hydroxychloroquine. Duloxetine is a selective serotonin reuptake inhibitor (SSRI) that has been found to be effective for the treatment of osteoarthritic pain. Intraarticular injections using a corticosteroid, biologic agent, or sodium hyaluronate have also been found to have an anti-inflammatory effect and provide pain relief. Additional pharmacologic agents used include muscle relaxants, glucosamine, and chondroitin.

9. Surgery
Arthroscopy is a procedure that is minimally invasive and can be used to remove loose bodies and meniscal tears. Osteotomy is a procedure for patients with a misaligned knee or hip who intend to continue with some physical activity.
Arthroplasty is a procedure where there is removal of the joint surface and a metal or plastic prosthesis is inserted. This prosthesis is then held in place by bone ingrowth or cement. Ten to 15 years of viability can be expected from the prosthesis provided that there are no complications. One of the main concerns of arthroplasty is infection. However, this is now quite rare due to the use of perioperative antibiotics. Fusion can also be performed to relieve pain. This is a procedure where there is union of the bones on either side of the joint. However, it prevents motion and causes more stress for the surrounding joints.
10. Prognosis
The prognosis of patients with osteoarthritis depends on the number of joints involved, which joints are involved, and the severity of the condition. The treatment for osteoarthritis is directed at symptomatic relief. Based on a systematic review, there are several factors that are associated with rapid progression of osteoarthritis of the knee.
The factors involved are higher body mass index, older age, multiple involved joints, and varus deformity of the knee. Those who undergo joint replacement have good prognosis with success rates for knee and hip replacement exceeding 90%. However, these prostheses will need to be replaced 10 to 15 years after replacement depending on the activity level of the patient.