What Is Vasculitis?
We have blood vessels of different sizes in our body and this enables the whole body to be supplied with fresh oxygen, and other essential nutrients. The circulatory system is a vast network and, is with other networks, and issue in one area can result in problems elsewhere. This has the potential to causes some serious problems.
One potential cause of such problems is vasculitis. This is a condition that directly affects the walls of our blood vessels and it can impact our blood vessels to the extent that our circulation is affected. It cannot be cured, but the good news for most people is the condition can at least be treated to help reduce the severity of any symptoms it might cause.

1. Vasculitis
Vasculitis, which is also known as angiitis and arteritis, is a condition that causes the walls of our blood vessels to become inflamed. There are many different types, some of which are quite rare. Vasculitis can be short term or long term, and it can also affect several organs at once, or it might only affect one.
The inflammation of the walls of the blood vessels can cause problems. The walls can become scarred and thicker. They can also become weaker, and the blood vessels can also become narrower. This can affect the flow of blood through the blood vessels, and this can result in a number of unwelcome symptoms.

2. Causes
The causes of vasculitis are not at all well understood. However, we do know that it is sometimes caused by an autoimmune condition. This means that the patient’s immune system is attacking the cells of their blood vessel walls. It is not really known why this happens, but it does appear to be associated with certain triggers.
Potential triggers include some cancers of the blood, while it can also be triggered by existing autoimmune conditions. Vasculitis might also sometimes be triggered by certain types of infections, while some types of medication can also be a trigger. In other cases, vasculitis appears to be down to genetics rather than an autoimmune condition.
3. Symptoms
The symptoms of vasculitis will depend largely on which particular type of vasculitis the patient is suffering from. These symptoms can be quite specific to each type, but there are also some symptoms that are more general and are likely to be found across most varieties.
Some of these symptoms include a headache, and a fever. The patient is also likely to experience aches and pains in their muscles and joints. A rash is another potential symptom, and the patient may also experience night sweats. The patient may also develop problems with their nerves resulting in numbness, and they may also lose weight.

4. Infections
In addition to the symptoms mentioned, vasculitis is also associated with certain complications. One of these is infections, which can sometimes be rather severe. While infections are not necessarily a direct symptom of vasculitis, infections are often a trigger, meaning that the two conditions will often go hand in hand.
There are numerous different types of infection associated with vasculitis, one of which is pneumonia. This is a potentially serious lung infection that has the potential to cause respiratory failure. Sepsis is another potential complication, which is caused by a dangerously strong reaction to an infection by the immune system.
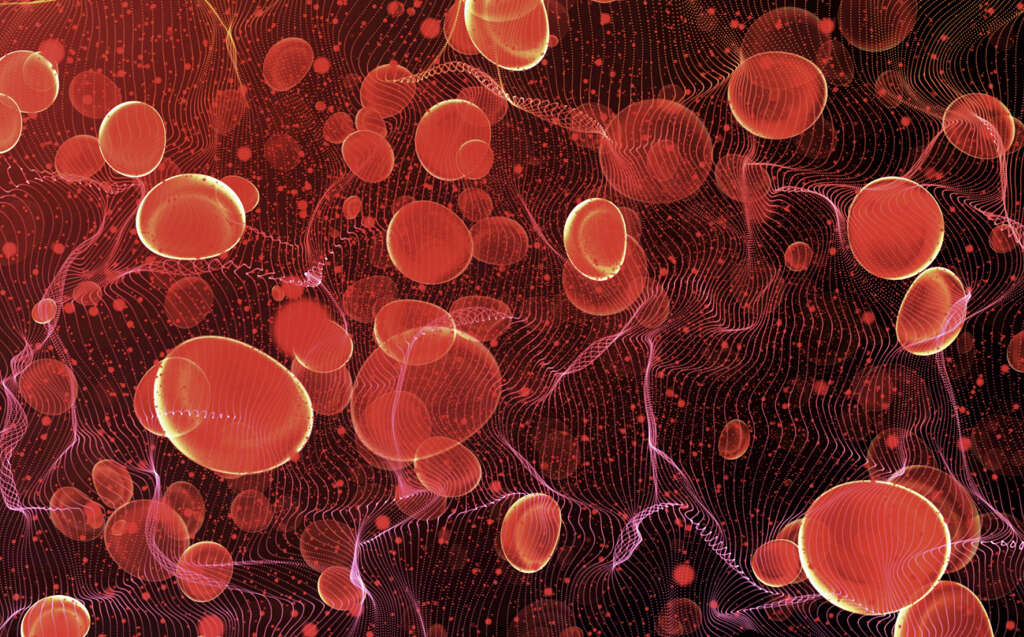
5. Blood Clots
Another potential complication of vasculitis is the formation of blood clots, and these can further obstruct the flow of blood. There is also the possibility of a blood clot becoming dislodged, and it may then travel through the circulatory system until it becomes stuck elsewhere.
A blood clot that gets stuck can result in an embolism, which is a very serious medical emergency. If the walls of the blood vessels are sufficiently weakened then the patient can suffer from an aneurysm, which is a condition where the wall of the blood vessel bulges outward. This can rupture, which will be fatal in some cases.

6. Blindness
Giant cell arteritis, which is also known as temporal arteritis, is a condition that can cause the thickening of the temporal artery. This is an artery that helps to supply blood to the head and brain, including the eyes. If the blood flow is impeded enough then it can result in the patient losing some, or all, of their vision.
The patient will often only experience blindness in one eye to begin with, and they are unlikely to experience pain. However, blindness can also follow in the other in just a few days afterwards. This symptom is usually only found in older people and those over the age of 50 are most at risk.

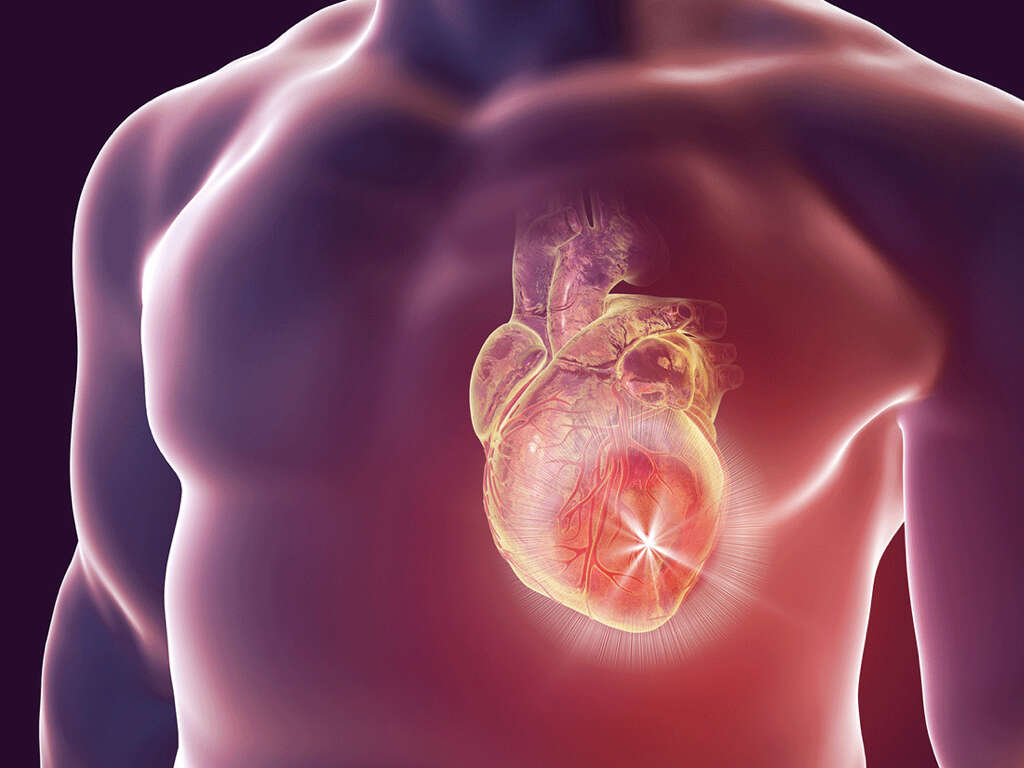
7. Organ damage
Vasculitis can affect the flow of blood to our organs, and a lack of blood can mean that the organ’s cells begin to suffer. Gradually, as the cells die, the organs become damaged and become gradually less effective at their job. Vasculitis can also affect the organs in other ways, however.
Vasculitis will also sometimes affect the blood vessels inside the organs themselves. One example of this is glomerulonephritis, which is also known as renal vasculitis, and it affects blood vessels in the kidneys that help them to filter impurities. This can affect the organ’s ability to keep our blood clean, and this can result in various unwelcome symptoms for the patient.

8. Who’s At Risk
Vasculitis can occur in anybody, and some people are even born with certain varieties of vasculitis. However, some people are more prone to developing the condition than others are. These include people who smoke regularly and, if you do smoke, it is a good idea to quite for a myriad of reasons in addition to avoiding vasculitis.
Also in a higher risk category are people who already have other types of autoimmune condition. This includes conditions like lupus, rheumatoid arthritis, and scleroderma. People who have certain chronic infections like hepatitis B or C are also are a higher risk of developing vasculitis.
9. Diagnosis
Your doctor will need to know about your medical history and about your symptoms. They might also ask about any medical conditions that run in your family. A number of tests may be needed to help confirm the diagnosis. These will often involve taking urine and blood samples for closer examination.
These samples will help experts to look for signs of inflammation that can help reveal vasculitis. X-rays and other imaging tests may also be used to help reveal signs of vasculitis. In some cases, a biopsy may be performed, which involves removing a small sample of the tissue so it can be examined.

10. Treatment
There is no cure for vasculitis and the treatment cannot be cured. However, medication is available that will help to manage the condition. This will typically involve anti-inflammatory medication to help reduce inflammation, and to help prevent it from flaring up again.
Other medications used can include those that will help to manage blood pressure. Medications that will help to prevent blood clots may also be used in some cases. There may also be a need to treat the symptoms of organ failure and other complications. Surgery will also sometimes be deemed necessary, including surgery to help treat an aneurysm.