What Is Pyloric Stenosis?
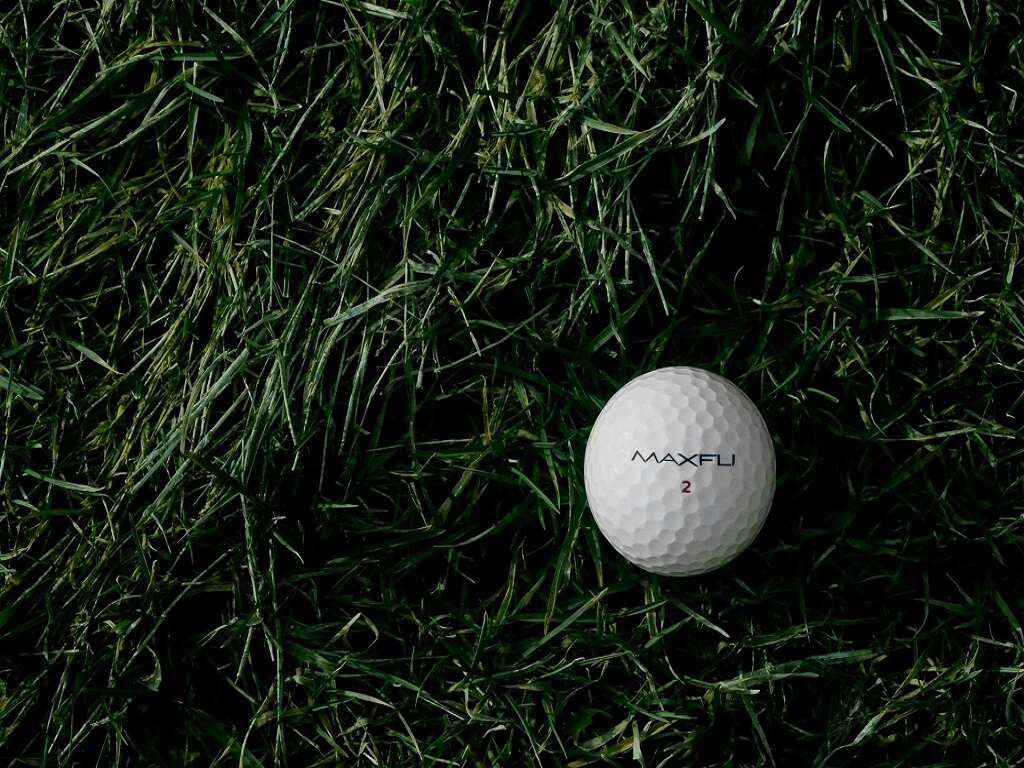
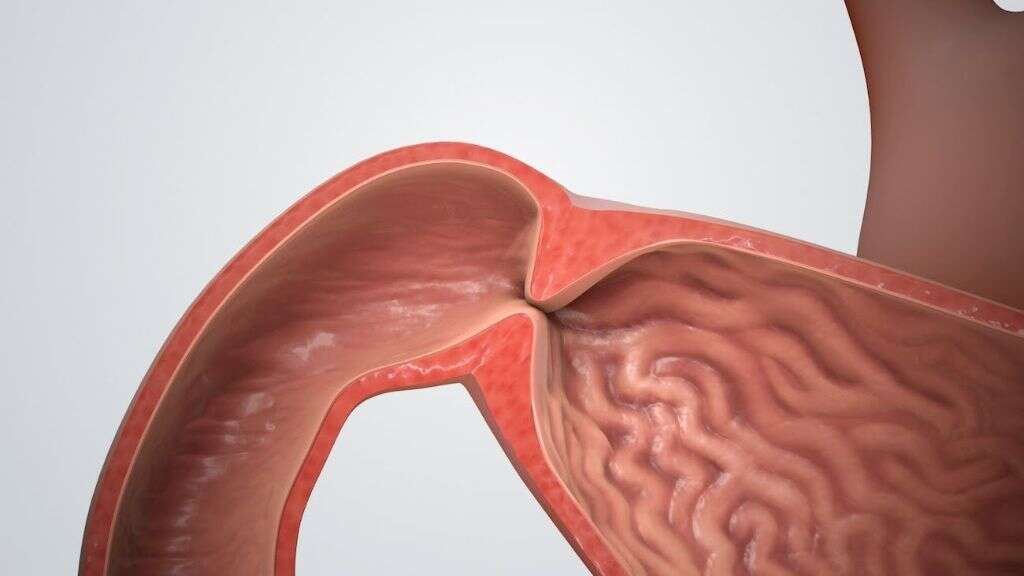
Pyloric stenosis is an issue affecting the lower portion of the stomach, the pylorus. This condition refers to a narrowing in the pylorus’s opening to the intestines, which prevents digestion and forces vomiting. Doctors have found the disorder affects newborn infants up to six months of age. If left untreated, it can become a grave concern.
Weight loss and dehydration are the primary worries with pyloric stenosis. Newborns, with their smaller proportions, cannot afford to lose vital nutrients. Because of their size, problems and deterioration can occur rapidly, which means diagnosis and treatment must be fast and accurate. If you have a child with this condition or find yourself concerned about witnessing common symptoms, this article is for you. The following 10 FAQs will provide a better understanding of the pyloric stenosis and its treatments.

1. What Are the Primary Signs of Pyloric Stenosis?
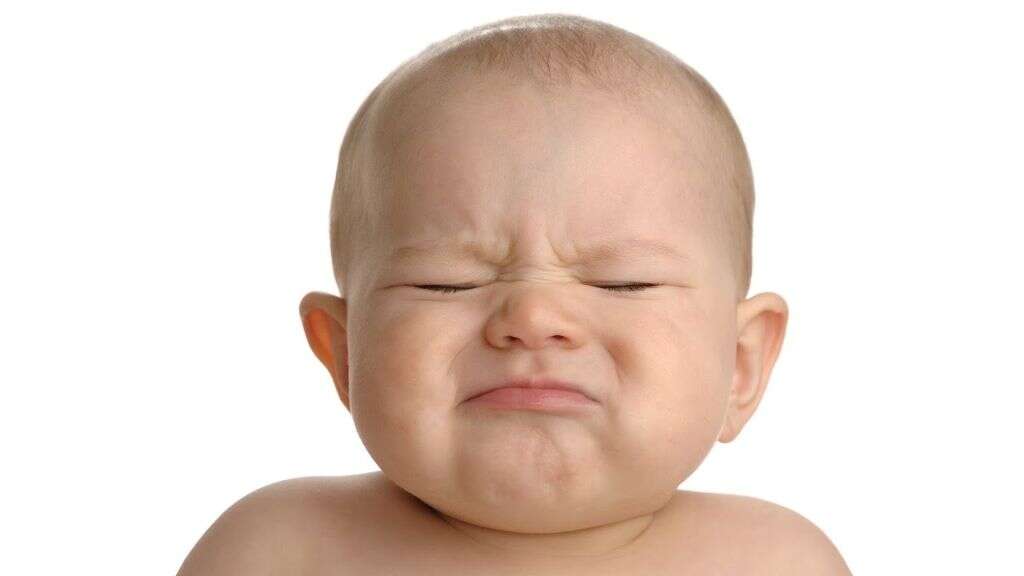
Any new parent should watch for at least three signs of pyloric stenosis: (1) vomiting, (2) weight loss and (3) hunger. While vomiting is a sign of this disorder, all newborns vomit from time to time. You need to be cautious of frequent and projectile vomiting. For example, if your baby is vomiting after most meals and the vomit spews out several feet, schedule a physical exam to discuss the issue with your doctor.
If vomiting couples with weight loss and unsatiated hunger, you may have a reason for concern. If your newborn is still hungry after vomiting and he or she is losing weight consistently, pyloric stenosis might be the problem. However, it is possible that something else is contributing to the issues your baby is having, which is why a doctor’s examination is necessary. With rapid weight loss, it is essential to have your baby examined as soon as possible.

2. Are There Any Additional Symptoms of Pyloric Stenosis?
Beyond routine vomiting, weight loss and ravenous hunger, be mindful of your newborn’s energy levels and bowel movements. If your infant is lethargic with limited bouts of energy, you may have cause for concern. Minimal energy can mean malnutrition. Your baby is not receiving the nutrients he or she needs, which corresponds with less energy and more sleep. The combination of weight loss, vomiting and lethargy are reliable indicators of a nutritional crisis.
Your infant’s bowel movements, or lack of, can also provide clues of pyloric stenosis. Routine constipation or frequent mucus stools suggests problems in the digestive tract. Even producing fewer bowel movements can point to trouble — most babies poop between three and 12 times per day. If your child is not pooping at least three times daily, he or she may have digestive problems, but seek medical advice for certainty.
3. What Causes Pyloric Stenosis?
Pyloric stenosis is a congenital disorder and a multifactorial trait, meaning both genetic and environmental factors contribute to its development. However, the actual causes of the condition are unknown. Doctors and researchers believe the enlargement of the pylorus muscles, which contributes to the narrowing of the pylorus, occurs after birth. Only in rare instances does the condition present at birth.
Gender and maturity also seem to play a role in the development of pyloric stenosis. The condition is more likely to develop in premature babies and appear four times more often in boys than girls. While gender and developmental maturity are strong indicators of likelihood, susceptibility is possible in any child, and the signs and symptoms are universal. Therefore, be cautious and mindful during the first several months of your child’s life.

4. How Is the Condition Diagnosed?
If your infant presents with the signs and symptoms of pyloric stenosis, then a doctor’s appointment is necessary to confirm the diagnosis. The examination may include a physical exam and additional testing. Most times, a doctor may feel an olive-shaped lump in your child’s abdomen. This lump is the enlarged pyloric muscles. During an exam, your child’s doctor may notice reverse peristaltic waves, which is another indicator of pyloric stenosis.
If a lump and reverse peristaltic waves are present, the doctor may order additional tests. An ultrasound will provide a view of the pylorus to confirm a diagnosis. However, if the ultrasound is unclear, the doctor may request X-rays of the digestive system. Blood tests are also used to check for electrolyte imbalance and dehydration, which are potential consequences of the condition.

5. What Are the Standard Treatments for Pyloric Stenosis?
The only suitable treatment for pyloric stenosis is surgery. While the prospect of surgery is uncomfortable for most parents, the narrowing of the pylorus region is life-threatening. Most often, the diagnosis and the surgery occur on the same day. If your baby’s blood work suggests there is an electrolyte imbalance or dehydration, he or she will receive fluids before the surgery to reduce any complications.
The surgery to correct pyloric stenosis is a pyloromyotomy. It is a minimally invasive surgery performed laparoscopically to ensure a fast recovery. The doctor creates an incision near the baby’s navel and inserts a small viewing instrument. With a good field of view, the surgeon cuts the outer layer of the pylorus muscle, which allows the inner lining to bulge out, opening the pylorus channel to the small intestine.

6. Do Patients Recover with Treatment?
The outlook for infants post-surgery is excellent regarding pyloric stenosis. Some vomiting may continue for a few days after surgery but then dissipate. To help your baby through the first few hours after surgery, the doctor and nurses may give intravenous fluids. However, parents can expect to feed their babies within the first 12 to 24 hours. Know that your infant may want more feedings than usual in the days following the surgery.
Parents must also be watchful of potential bleeding and infection during recovery. While these complications are not common, they can occur, and your baby will need medical intervention if they do. However, do not stress about these possibilities, as most babies recover with minimal to no complications.

7. Are There Dangerous Complications from Pyloric Stenosis?
Pyloric stenosis is a dangerous condition if left untreated. The enlarging of the pyloric muscles restricts the digestive system severely, forcing the baby to projectile vomit. Aside from injuries that can occur from violent episodes of vomiting, the condition can lead to choking and asphyxiation.
However, the main concerns of pyloric stenosis are malnutrition and dehydration. The size of an infant means that weight and fluid loss occurs much faster than with adults. A baby may experience severe dehydration in a matter of hours. If you notice a dry diaper after two to three hours, do not wait to contact the doctor, especially if you suspect this condition.
8. Who Does Pyloric Stenosis Affect?
Pyloric stenosis can affect any gender and ethnicity, but it is more prominent in Caucasian males, specifically those of northern European ancestry. The defect is also more common in premature babies than those carried to term.
Beyond heritage and development, a few other circumstances may contribute to pyloric stenosis development: smoking, antibiotics and bottle-feeding. You should never smoke during pregnancy, and studies suggest this behavior doubles the likelihood of pyloric stenosis. Some medicines may also increase the risk of developing the condition. For example, erythromycin, a standard whooping cough treatment, increases the odds. Also, in the great breastfeeding versus bottle-feeding debate, breastfeeding may have another leg up on the bottle. However, the studies might have skewed datasets, so more research is necessary.

9. Can You Give Your Baby Pyloric Stenosis?
Pyloric stenosis is a multifactorial trait, meaning genetics may play a role in its development. However, the environment also contributes to the condition. Therefore, it is not necessarily something you give to your child or transmit to him or her. Some studies point to a familial tie, but the numbers refer to only a 10% to 20% increased risk, meaning that other factors may play a more significant role in this specific congenital disorder’s development.
Whether lineage or genetics contribute to pyloric stenosis development, take the blame away from the diagnosis. You would not intentionally hurt your child. While this condition is frightening and dangerous, it is correctable. Blaming yourself, or saying you gave your child a condition, does not help anyone, and only stands to hurt your relationship with your child.

10. What Is the Recurrence Rate, If Any?
After the pyloromyotomy, the outlook for pyloric stenosis patients is excellent. Most infants will not experience further complications. However, in rare circumstances, the condition can return in later adolescence and adulthood. Ulcers or adhesions may cause the return of the defect, but the recurrence rate is minimal and not statistically valid. Most patients will recover from pyloric stenosis surgery with no further complications or concerns for the rest of their lives.
Pyloric stenosis is a dangerous congenital disorder that restricts the passageway from the stomach to the small intestine. Without surgical intervention, affected infants, age zero to six months, may suffer significant complications, from dehydration to malnutrition. If your baby is projectile vomiting and exhibiting signs of this condition, then contact your baby’s doctor to schedule an appointment. Be sure to specify your concerns over the phone to get the earliest appointment possible.