What Is Primary Biliary Cirrhosis?
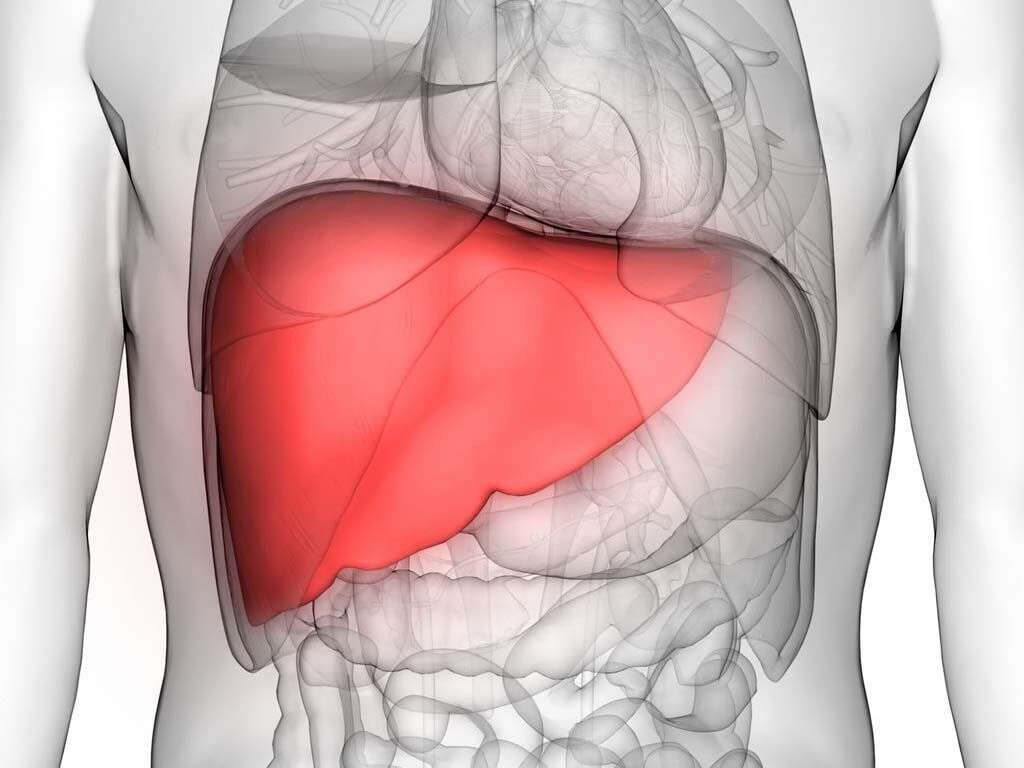
The liver is a very important organ for us. Not only does it help to filter out toxins, but it also produces various hormones and other compounds that play a very important role in the functioning of our bodies. One of these compounds is bile, and it helps us to digest foods.
The bile is transported through the biliary ducts from the liver to the gallbladder (hepatic and cystic ducts) and from the gallbladder to the small intestine (common bile duct). Primary biliary cirrhosis is a chronic, autoimmune condition that affects the bile ducts directly. In fact, nowadays it is known as primary biliary cholangitis, since cirrhosis only occurs in the late stage of the disease.
Bile is a substance that helps us to break down our food, especially fats. It is produced in the liver and is then passed on to the gallbladder, which is where it is stored until it is needed. When needed, it will then be released into the digestive system where it can help to break down our food. The bile duct helps to carry bile from the liver to the gallbladder, and also from the gallbladder to the duodenum in the small intestine. As with other parts of the body, the bile duct is not completely safe from developing problems, and this can result in a number of unwelcome symptoms.

1. Bile Duct
Bile is a substance that helps us to break down our food, especially fats. It is produced in the liver and is then passed on to the gallbladder, which is where it is stored until it is needed. When needed, it will then be released into the digestive system where it can help to break down our food. The bile duct helps to carry bile from the liver to the gallbladder, and also from the gallbladder to the duodenum in the small intestine. As with other parts of the body, the bile duct is not completely safe from developing problems, and this can result in a number of unwelcome symptoms.

2. Disease Process
Primary biliary cholangitis, is an autoimmune condition that results in progressive destruction of small to medium bile ducts in the liver, causing a chronic reduction or stoppage of bile flow known as cholestasis. Thus, bile and other toxins that are normally excreted, build up in the ducts within the liver and cause further damage. The resulting inflammation of the bile duct system that occurs in the early stage of the disease is known as cholangitis.
Finally, progressive damage to the tissue involved can lead to scarring, fibrosis, and eventually end-stage liver disease or cirrhosis in the late stages of the disease. In short, cirrhosis is a complication of many liver diseases characterized by the replacement of normal hepatic tissue by scar tissue. This can alter the normal functions of the organ and lead to liver failure.
3. Causes
There is a lot that we don’t know about primary biliary cholangitis, and exactly why it happens is still somewhat of a mystery. Evidence indicates that it is an autoimmune condition. Recall, that one of the functions of our immune system is to protect our body by responding to invading microorganisms by producing antibodies or sensitized lymphocytes (types of white blood cells). In some cases, however, immune cells mistakenly attack the very cells that they are meant to protect.
In primary biliary cholangitis, there are abnormalities in the production of antibodies (i.e. antibodies against host tissue) and impaired regulation of lymphocytes (B and T lymphocytes). In fact, activated lymphocytes (CD4 and CD8) are partly responsible for the chronic destruction of small and medium bile ducts. Finally, primary biliary cholangitis can be associated with many other autoimmune diseases (i.e. autoimmune thyroiditis, scleroderma).
4. Symptoms:Itchy Skin
Most patients are asymptomatic during the early stages of the disease and almost a quarter of them are incidentally diagnosed during a routine blood test. However, there are a few symptoms that patients can exhibit from the start.
Itchiness or pruritus is often the first symptom that a lot of people with primary biliary cirrhosis will experience. In fact, roughly ten percent of patients exhibit severe itchiness in the skin. Contrary to common beliefs, this symptom is not related to the deposition of bile acids in the skin. The cause is unknown; however, it appears to be related to the increased production and effects of opioid peptides. Normally, these substances act on opioid receptors throughout the central nervous system to cause different effects, including pain relief, reduced anxiety, and enhanced mood. In this case, the production of these substances causes severe pruritus and seems to be proportionally related to bilirubin levels.

5. Symptoms: Fatigue
Most people can find themselves temporarily overtired from time to time, but usually, there is an identifiable cause within their routine or habits. However, the medical definition of fatigue involves an unrelenting sensation of exhaustion that lasts longer, is more profound, and isn't relieved by rest.
People with fatigue can have reduced energy, motivation, and concentration. Many diseases can cause fatigue; thus it is not exclusive of primary biliary cholangitis. However, it is one of the first symptoms reported by patients with this condition. Its etiology is uncertain, and it does not correlate with the stage of liver disease or the levels of hepatic enzymes.

6. Symptoms: Abdominal discomfort
One of the symptoms of primary biliary cholangitis is pain or discomfort in the abdomen. This sensation tends to be located in the upper right quadrant of the abdomen because it is here where the liver is located. This can occur in roughly eight to seventeen percent of patients; although it is most common in the late stages of the disease.
Pain and tenderness in the upper right area of the abdomen can also indicate hepatomegaly or the inflammation of the liver. Hepatomegaly is a finding on physical examination on approximately 25% of patients with primary biliary cholangitis. The condition can also cause inflammation of the spleen or splenomegaly.

7. Skin changes
Primary biliary cholangitis can cause hyperpigmentation or darkening of the skin that is not related to sun exposure. This phenomenon is given by the excessive synthesis of melanin, a skin pigment produced by melanocytes to protect our skin cells from the harmful radiation that we receive from sun exposure. The enzyme responsible for the initial reaction of melanin synthesis is known as tyrosinase, and it requires copper to function properly. Importantly, the liver is the organ responsible for copper metabolism in the body, and almost 80% of it is excreted in the bile and eliminated in the feces. Thus, when the liver is compromised in these patients, copper is accumulated in the body. In short, in patients with primary biliary cholangitis, the activity of tyrosinase and the synthesis of melatonin are increased, inducing hyperpigmentation.
The liver is the organ responsible for the elimination of almost all excess cholesterol from the body, through direct secretion into bile and via conversion to bile salts. In patients with diseases (such as PBC) that cause a reduction of bile flow (cholestasis), cholesterol levels in the blood are elevated because it’s excretion is decreased. Importantly, hypercholesterolemia, or cholesterol values above 200 mg/Dl, affects roughly 75% of patients with primary biliary cholangitis at presentation. Prolonged elevations in cholesterol levels in the blood may give rise to xanthelasmas. These are sharply demarcated yellowish plaques of cholesterol underneath the skin that usually occur on or around the eyelids.

8. Advanced Liver Disease
In late-stage primary biliary cholangitis, cirrhosis ensues. Signs of end-stage liver disease include ascites and peripheral edema. Ascites is the accumulation of fluid in the abdomen. It is given by many complex factors, but ultimately it is a result of liver dysfunction.
Furthermore, peripheral edema manifests as swollen feet and ankles. However, peripheral edema can be the result of a variety of conditions.

9. Diagnosis
As mentioned above, some patients with primary biliary cholangitis are incidentally diagnosed during routine blood work. Physicians can be alerted by significant elevations of enzymes in liver function tests that signal liver disease and bile duct injury. Thus, aminotransferases (ALT and AST), alkaline phosphatase (ALP), and ᵧ-glutamyl transpeptidase (GGTP)can be high. Furthermore, as mentioned above patients with PBC can present with hypercholesterolemia. Thus, physicians should also measure lipid and cholesterol levels in the blood. Also, antibody tests for signs of autoimmune disease can be useful for diagnosis. Anti-mitochondrial antibodies (AMAs) can be found in almost 95% of patients with primary biliary disease. These antibodies seldom occur in people without the condition. Thus, a positive anti-mitochondrial antibody test is a reliable sign of the disease. Nevertheless, a small number of patients with the condition don't exhibit AMAs.
Imaging studies can be useful to exclude obstruction of the biliary tract (CT or MRI), to diagnose portal hypertension (a consequence of cirrhosis) and its consequences, and to evaluate liver tissue.

10. Risk Factors
The etiology of primary biliary cholangitis is unknown. However, some factors may increase your risk of primary biliary cholangitis. For instance, sex is an important factor because approximately 75% to 90% of patients with primary biliary cholangitis are women. Age is also important because it's most likely to occur in people 30 to 65 years old. Also, genetic factors play an important role because you're more likely to develop the condition if you have a relative who has or had it (570- to 1000-fold with a first-degree family member). Finally, PBC is most common in northern Europe and North America.
Additionally, certain environmental factors can interact with genetic factors in order to trigger the onset of primary biliary cholangitis. These factors include infections (i.e. bacteria of the Enterobacteriaceae), smoking, and toxic chemicals.