What Is Polymyositis?
Polymyositis is a rare condition that causes the patient to experience considerable loss of muscle strength, in addition to some other symptoms. It occurs when the immune system attacks the patient’s muscles, causing inflammation of the tissue.
With treatment, some patients can regain some degree of muscle strength. Furthermore, polymyositis can also increase the chances of the patient developing other conditions like cancer, pulmonary disease, or other autoimmune conditions.

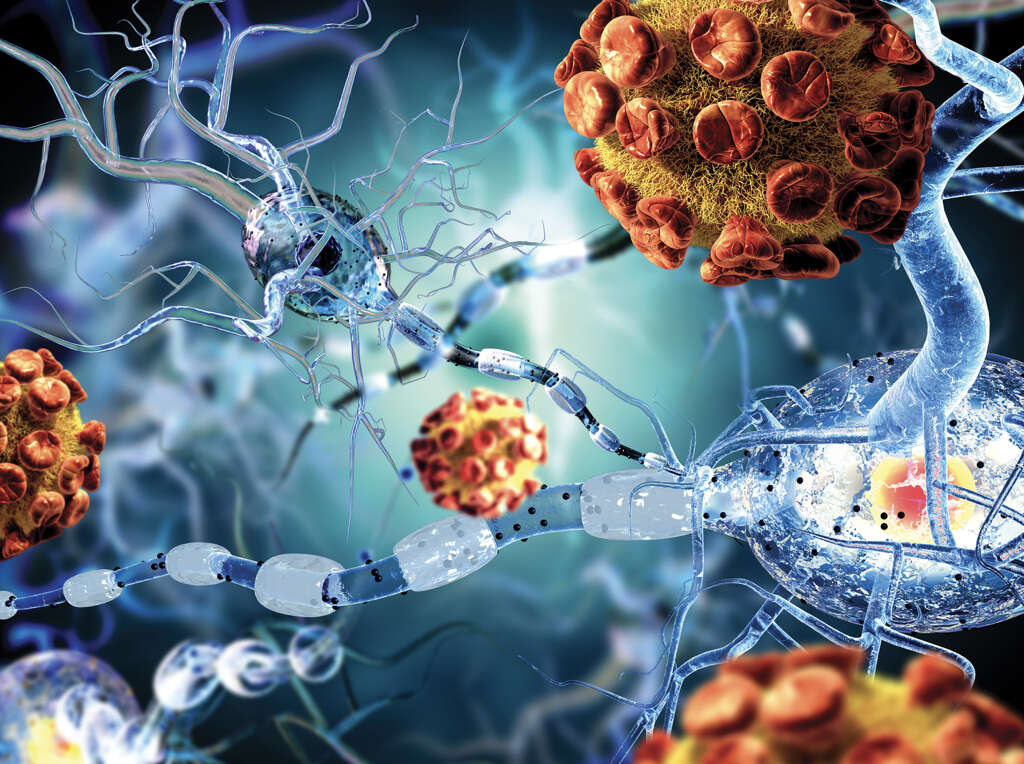
1. Cause
Exactly why polymyositis happens is not at all well understood; thus it is known as an idiopathic disease. However, we do know that it is an autoimmune condition partly mediated by T- lymphocytes, cells that are part of our immune system. Allegedly, T cells mistakenly target unknown molecules in the muscle, eventually surrounding, invading, and destroying healthy tissue. This leads to insidious onset of muscle weakness.
Polymyositis is frequently associated with other autoimmune conditions. As is typical for autoimmune conditions, there is no known cure for polymyositis. It can, however, be treated and some people go on to make a partial, if not full, recovery.
2. Risk Factors
Certain demographics can make somebody more likely to have the condition than others. For example, it is rare in children, affects women more than men, and usually affects people between 30 and 60 years old.
Another risk factor is the presence of other autoimmune disorders, particularly lupus, scleroderma, Sjögren syndrome, and rheumatoid arthritis. There is also a link with viral infections, malignancies, and connective-tissue diseases.
3. Muscle Weakness
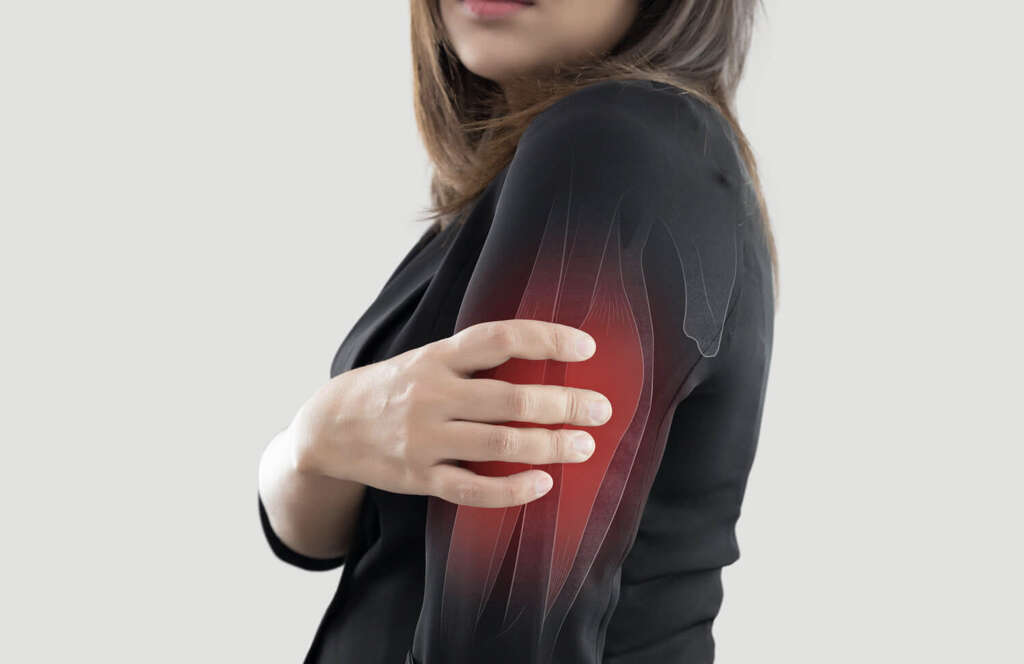
Perhaps the most characteristic symptom of polymyositis is that the patient will experience fluctuating weakness in their muscles. The weakness will start to develop slowly and will be found on both sides of the body (symmetrical).
The muscles most likely to be affected are those that are closest to the torso (proximal muscles). This means the hips, neck, shoulders, thighs, upper arms, and upper back. Patients with the condition will find it difficult to make movements like walking upstairs, standing from a seated position, and carrying objects. In a rare number of cases, the patient will also have difficulty swallowing (dysphagia).

4. Muscle Pain
In addition to weakness, the patient will sometimes experience considerable pain and tenderness. This pain can occur in the muscles themselves and it can also happen in the patient’s joints (arthritis).
These symptoms will often develop very gradually and, in some instances, it may be weeks or months before the patient even notices that something is wrong. Patients with polymyositis will often also find that their muscles begin to waste away (atrophy). This will have the effect of making them smaller than they used to be. These are symptoms that should encourage the patient to speak with a medical professional.

5. Weight Loss
Patients with polymyositis can experience constitutional symptoms, including fever, fatigue, anorexia, and unintentional weight loss. Additionally, the patient’s muscles will begin to waste away, and this will contribute to weight loss.
Also, other symptoms (i.e. difficulty to swallow) may mean they are less likely to want to eat and this can also contribute to weight loss. Note that rapid and unintentional weight loss is never healthy, even if you are overweight.

6. Respiratory manifestations
Patients with polymyositis may experience breathing difficulties (i.e. shortness of breath or respiratory failure) if the chest wall muscles are compromised by the disease. As a result of the dysphagia (difficulty swallowing) caused by the disease, patients can develop a respiratory infection (pneumonia) as a result of accidentally breathing in food or liquids.
Finally, patients with polymyositis can develop interstitial lung disease. This is a chronic condition that causes scarring or fibrosis of the lung tissue, making it stiff and no longer elastic.

7. Diagnosis
Diagnosis of the condition is not easy and it will often be some time before doctors can be confident enough to conclude. One of the first things that doctors are likely to do is to ask you about your medical history, and whether there is a history of related medical conditions in the family.
A muscle biopsy is often performed to evaluate the muscle tissue on the microscope, and an MRI scan is also useful to assess muscle involvement, guide biopsy, and to identify extra muscular disease. Also, electromyography (EMG) is often performed to measure the electrical activity occurring in the muscles. Also, blood tests will be used to assess muscle enzyme levels (i.e. serum creatinine kinase), and to verify the presence of abnormal autoantibodies in the blood.

8. Physical Therapy
While there may be no cure for polymyositis, treatment is available that can at least help to limit the severity of the symptoms. One treatment often used is physical therapy. This involves getting the patient to exercise their muscles to help make them stronger, while also working on coordination and other aspects.
Physical therapy can be hard work. It can be very frustrating at times and even painful, but the patient must persevere because the therapy can be effective at helping people regain strength. The results generally mean that the patient will find it easier to move around and give them the strength to go about their day-to-day activities.

9. Medication
Most patients with the condition will be given medication that will help to suppress the immune system, reducing the harm it can do to the body. However, this has the downside of making the patient more susceptible to other diseases. In addition, patients are usually given corticosteroids.
One of the most useful aspects of steroids is that they are very effective in controlling polymyositis symptoms. They can help to relieve pain and decrease the levels of inflammation in the body. Steroids can also have unwanted side effects, however, so they will need to be used with caution.

10. Complications
While the condition is not usually dangerous when treated, it is possible that some serious complications can occur. One of these is aspiration pneumonia, which is when food and liquid are inhaled into the lungs instead of going to the stomach, causing an infection.
Loss of muscle strength in the throat area can also make it difficult for the patient to eat. If the chest muscles are significantly weakened, then it can mean the patient struggles to breathe. In severe cases, this can lead to a fatality as the patient’s respiratory system fails. Thankfully, extreme cases are rare and the prognosis is generally good overall. However, it is not uncommon for the patient to never fully regain their strength.