What Is Myofascial Pain Syndrome?
 Article Sources
Article Sources
- 1. Myofascial Pain Syndrome [n.d.]. Retrieved from https://www.mayoclinic.org/diseases-conditions/myofascial-pain-syndrome/symptoms-causes/syc-203754442.
- 2. Mayo Clinic Q and A: Understanding Myofascial Pain Syndrome and Fibromyalgia [Dec. 1, 2017], https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-q-and-a-understanding-myofascial-pain-syndrome-and-fibromyalgia/
- 3. Myofascial Pain Syndrome [n.d.]. Retrieved from https://my.clevelandclinic.org/health/diseases/12054-myofascial-pain-syndrome/diagnosis-and-tests
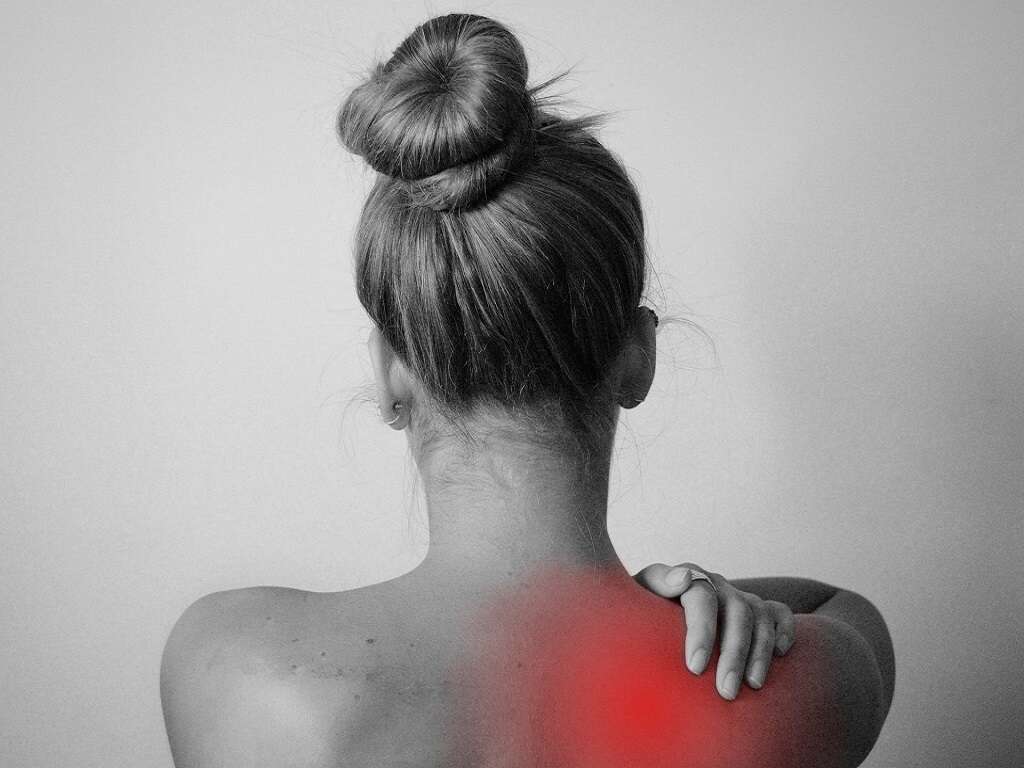
Everyone has muscle pain from time to time. Usually that pain goes away as your muscles heal from the injury or stress that caused the discomfort. Sometimes, however, your pain sticks around and becomes chronic. If you’re experiencing persistent muscle pain, you may be suffering from myofascial pain syndrome, or chronic, aching muscle pain that worsens with pressure to sensitive areas known as trigger points.1Myofascial Pain Syndrome [n.d.]. Retrieved from https://www.mayoclinic.org/diseases-conditions/myofascial-pain-syndrome/symptoms-causes/syc-203754442.
In many cases, uncertainty and anxiety can worsen your experience of chronic pain. If you’ve been diagnosed with myofascial pain syndrome, learning more about your condition can be a helpful tool in managing your symptoms and improving your understanding of what’s going on inside your body.

1. Causes
Myofascial pain syndrome is generally a result of injury or prolonged strain to a muscle. In most cases, your body responds to this type of stressor by repairing any damage to your muscle, allowing it to function effectively and painlessly, as it did before the injury.
In some cases, however, collections of sensitive, tight muscle fibers collect in the damaged muscle to form what is known as a trigger point, or a localized area of acute sensitivity. When pressure is applied to that trigger point, someone with myofascial pain syndrome will experience either localized muscle pain or referred pain in a remote part of the body.2Mayo Clinic Q and A: Understanding Myofascial Pain Syndrome and Fibromyalgia [Dec. 1, 2017], https://newsnetwork.mayoclinic.org/discussion/mayo-clinic-q-and-a-understanding-myofascial-pain-syndrome-and-fibromyalgia/

2. Risk Factors
Injury-related muscle strain and chronic stress and anxiety are the primary risk factors for myofascial pain syndrome. Either factor can cause damage to your muscles that leads to the condition.
Chronic stress can cause prolonged muscle tension, often in a sufferer’s neck, shoulders, or back. Just like in the case of injury, muscles can respond to persistent tension by developing sensitive trigger points and related myofascial pain syndrome.

3. Transmission
Myofascial pain syndrome is not transmissible from one person to another. However, the risk factors for myofascial pain syndrome are relatively limited, and it’s possible that the conditions that increase one patient’s risk may be common throughout a group.
Work environments or athletic activities that require physically demanding activity may increase the risk of developing myofascial pain syndrome among many participants. Any activity that puts a participant at risk of physical injury or places repetitive strain on a muscle can result in myofascial pain syndrome. Small changes, such as improving ergonomics or providing information about self-care and recovery, can reduce the occurrence of myofascial pain syndrome within a group.

4. Diagnosis
When you visit your doctor for help with lingering pain, he or she can conduct a physical exam and probably apply gentle pressure to the painful area, looking for knots in your muscles and evaluating your body’s response.
Your doctor can also ask questions about the origin and duration of your symptoms, such as how long you have experienced the pain, what were the circumstances of its onset, what makes the pain better or worse, and what treatments you have already tried. Although there are no imaging or blood tests available to diagnose myofascial pain syndrome, your doctor may order such tests to rule out other causes.

5. Signs & Symptoms
Deep, lingering muscle pain, associated trigger point sensitivity, and acutely painful or tender knots within a muscle are the primary symptoms of myofascial pain syndrome. The pain typically persists despite standard home remedies for muscle aches, such as ice packs, warm compresses, or over-the-counter medications.
Many people with myofascial pain syndrome also experience fatigue and poor sleep. However, these are typically a result of sleep disruptions due to pain and not directly caused by myofascial pain syndrome.

6. Complications
Chronic pain, such as myofascial pain syndrome, can lead to mental health concerns or exacerbate pre-existing depression or anxiety. The general lack of obvious external signs can cause patients to question their own symptoms and may contribute to skepticism among family and friends. Additionally, chronic pain can interrupt a sufferer’s daily activities, which may also increase feelings of isolation.
Some researchers believe that myofascial pain syndrome, when left unresolved, can evolve into fibromyalgia, in which the patient experiences chronic pain throughout the body, instead of in a localized area. Fibromyalgia also generally presents with more trigger points than myofascial pain syndrome and frequently includes other non-pain symptoms, such as fatigue, digestive distress, or headaches.3Myofascial Pain Syndrome [n.d.]. Retrieved from https://my.clevelandclinic.org/health/diseases/12054-myofascial-pain-syndrome/diagnosis-and-tests

7. Treatment & Management
Most treatments for myofascial pain syndrome involve either medication or needle procedures. Myofascial pain sufferers have found relief through pain medications, such as over-the-counter treatments or stronger prescription drugs, and other types of medications, such as antidepressants or sedatives that encourage the release of muscle tension. A doctor may also recommend injections of pain medicine directly into an affected trigger point, acupuncture, or dry needling.
Additionally, physical therapy and exercise can help reduce the symptoms of myofascial pain syndrome. Activities that strengthen and stretch the body can help retrain muscles to move in ways that cause less strain. Other options for managing pain include activities that relieve stress and calm your mind and body, such as massage or meditation.

8. Prevention
The most effective way to prevent myofascial pain syndrome is to reduce your risk of initial injury by managing your stress levels and mitigating the effects of repetitive muscle strain. Actions like carrying your purse on the other shoulder, consulting an occupational therapist to improve your work environment, or avoiding unsupportive footwear can help prevent injuries that lead to muscle knots and trigger point pain.
Engaging in consistent and adequate exercise can also help reduce your risk of myofascial pain syndrome. By strengthening and stretching your muscles, you reduce your risk of injury. Exercise may also cause your body to release feel-good chemicals, called endorphins, that help reduce your overall stress levels.

9. Prognosis
Myofascial pain syndrome is a highly individualized condition. Each patient will have a different response to treatment and timeline for recovery.
In some cases, treating the root cause of muscle strain and tension may eliminate the pain, while for other patients it could linger long after the initial cause is addressed. Periodic pain flare-ups may also reoccur even after daily pain is relieved.

10. When to See A Doctor
You should see your doctor any time you experience pain that persists or worsens despite treatment. For some patients, the pain associated with myofascial pain syndrome may be severe. Other sufferers may not consider the pain bad enough to seek medical attention.
In either case, however, a doctor can help rule out other causes of your pain and offer treatment options that reduce your suffering and improve your quality of life. Treating your myofascial pain syndrome can also reduce your risk of developing complications, such as mental health issues or fibromyalgia.