What Is Polymyalgia Rheumatica?
Muscle pain and stiffness are characteristic of the inflammatory condition known as polymyalgia rheumatica. People with this condition experience higher levels of discomfort in the morning and most often in the shoulders and hips. The symptoms of the disorder can arise quickly.
Another inflammatory disorder called giant cell arteritis is related to polymyalgia rheumatica. However, this condition impacts different parts of the body. An individual with one of these disorders can develop the other as well.
1. Symptoms of Polymyalgia Rheumatica
People who develop this disorder often experience a sudden onset of symptoms, which may, in the beginning, be mistaken for the flu. Symptoms usually begin in the neck and shoulders but can rapidly spread to the upper arms, hips, buttocks and thighs. It is also possible for the condition to impact the knees, wrists and elbows. Pain and stiffness occur on both sides of the body and are worse in the morning and after periods of inactivity.
Polymyalgia rheumatica can cause additional symptoms similar to those of the flu. An individual can have feelings of overall fatigue, depression and malaise. It is not uncommon to develop a mild fever. Some people also lose their appetite and begin to lose weight without intending to.

2. Complications of Polymyalgia Rheumatica
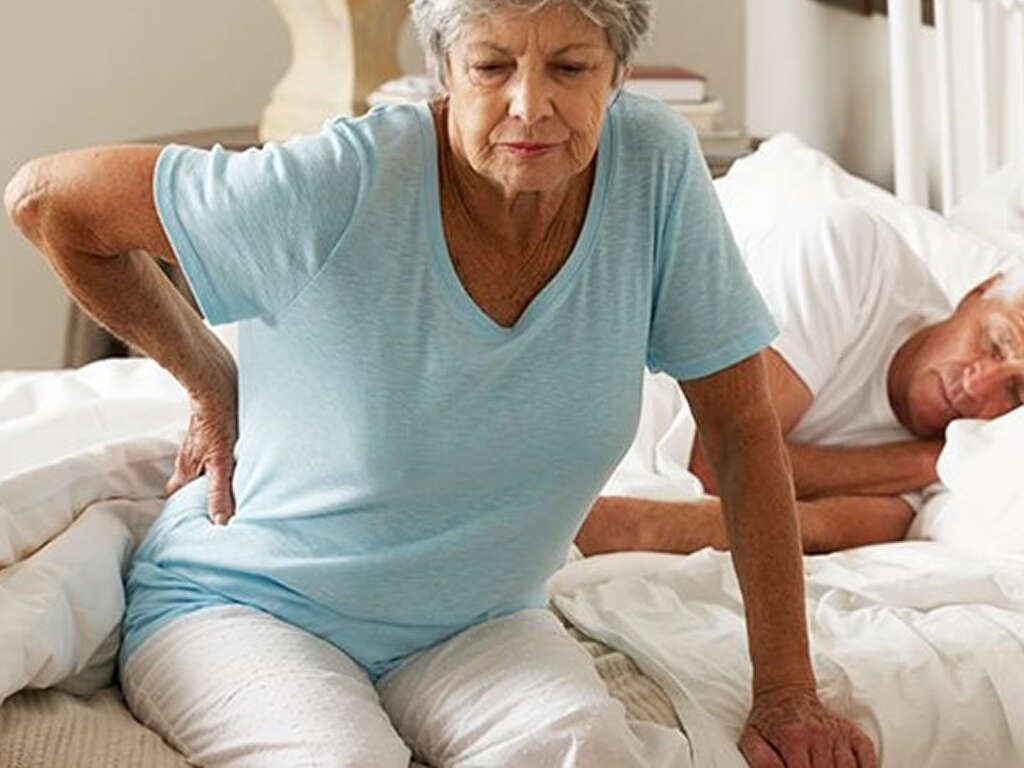
Polymyalgia rheumatica can cause significant disruptions in daily living. The severity of the pain and stiffness lead to difficulty performing tasks that would otherwise be completed with ease. Even getting out of bed or brushing teeth is challenging at times.
When the symptoms are severe, the effects of the disorder can spill over to impact every aspect of life. Maintaining the same level of activity as before the onset of the condition becomes difficult. As such, social engagements and physical activity diminish. Overall health, sleep quality and emotional wellbeing suffer as well.
3. Causes of Polymyalgia Rheumatica
It is not yet known precisely what causes polymyalgia rheumatica; however, there are two factors that seem to be at play: genetics and environment. The disorder is potentially linked to the aging process, and people’s genes may play a role in determining whether someone develops the condition.
Furthermore, there is an apparent connection to environmental influences, as new cases tend to be diagnosed in a cyclical pattern. This suggests the possibility that there is a seasonal exposure that triggers the onset, such as a virus. Whether this is actually the case has not yet been verified.
4. Risks Factors for Polymyalgia Rheumatica
Age is the predominant risk factor, as polymyalgia rheumatica almost exclusively affects those between the ages of 70 and 80. In addition, women are much more likely to develop the disorder than men by a factor of two to three.
This disorder is also seen more often in Caucasians than in any other race. More specifically, it is found in people who are of northern European or Scandinavian descent. This fact supports the idea that there is a genetic link for developing polymyalgia rheumatica.

5. Giant Cell Arteritis and Polymyalgia Rheumatica
Polymyalgia rheumatica is closely related to another serious inflammatory condition called giant cell arteritis. The two are similar; however, giant cell arteritis involves an inflammation of the linings in the arteries. It most frequently affects those in the temples. It is common for people who have symptoms of one condition to also show signs of the other.
The symptoms for giant cell arteritis include scalp tenderness, tightness in the jaw, headaches and vision problems. Treatment is critical for this condition to avoid serious complications. Without treatment, permanent vision loss, including blindness, is possible. Furthermore, the risk of stroke also significantly increases.

6. Diagnosis of Polymyalgia Rheumatica
Diagnosis and continued evaluation of an individual’s condition is necessary. There are cases when someone receives an initial diagnosis of polymyalgia, but, upon reevaluation at a later stage, is re-diagnosed with rheumatoid arthritis. Initial evaluation involves a physical examination, along with imaging and blood tests.
Ultrasound and MRIs are increasingly being utilized to narrow down a correct diagnosis. Ultrasounds help differentiate polymyalgia rheumatica from other similar conditions, while MRIs can illuminate alternative causes for joint pain. Blood tests are used to identify inflammation indicators, though these tests are not always conclusive.

7. Diagnosis of Giant Cell Arteritis
If you are diagnosed with polymyalgia, your physician will likely want to monitor you for giant cell arteritis. If you begin to experience symptoms such as jaw pain, headaches that are persistent and new, scalp tenderness or blurred or double vision, it is important to see your doctor as soon as possible.
These signs are indications that you may be developing giant cell arteritis. If your doctor suspects that this is the case, a biopsy of one of your temple arteries will be ordered. The procedure is done under local anesthesia, and the sample is evaluated for signs of inflammation.
8. Treatment for Polymyalgia Rheumatica: Medical
Polymyalgia rheumatica treatment almost always involves the use of medications to help control and ease symptoms. People with the disorder are typically placed on a low dose of corticosteroids. Since long-term use of these drugs results in serious side effects, the dose is gradually reduced after the first few weeks of treatment, though ongoing adjustments may be required.
To offset the potential side effects of the corticosteroids, doctors generally prescribe vitamin D and calcium supplements. These nutrients help reduce bone loss associated with steroids. Methotrexate is another possible option that suppresses the immune system and may be beneficial to those who don’t respond to the corticosteroids.

9. Treatment for Polymyalgia Rheumatica: Physical Therapy
Muscle pain and stiffness are the primary debilitating symptoms of polymyalgia rheumatica. Generally, corticosteroid treatment allows individuals to return to their previous levels of activity. However, for some, more help is required to get them moving again without pain and stiffness.
Typically, people who have overall lower activity levels prior to the onset of this condition, as well as those who wait to start treatment, find it more difficult to resume daily activities. In these cases, physical therapy may be recommended to improve range of motion and muscle strength.

10. Treatment for Polymyalgia Rheumatica: Home Care
It is not recommended for people to take over-the-counter anti-inflammatory drugs, such as ibuprofen, to deal with this condition. However, there are other measures individuals can take to improve and manage their symptoms, as well as reduce the side effects from the corticosteroids.
A healthy diet that includes a wide range of vegetables and limits salt intake provides the body with vital nutrients that can help with systemic inflammation and provides a boost in bone-building nutrients. Regular exercise also improves bone strength, and getting sufficient sleep allows the body to recover and heal.