What Is Peyronie's Disease?
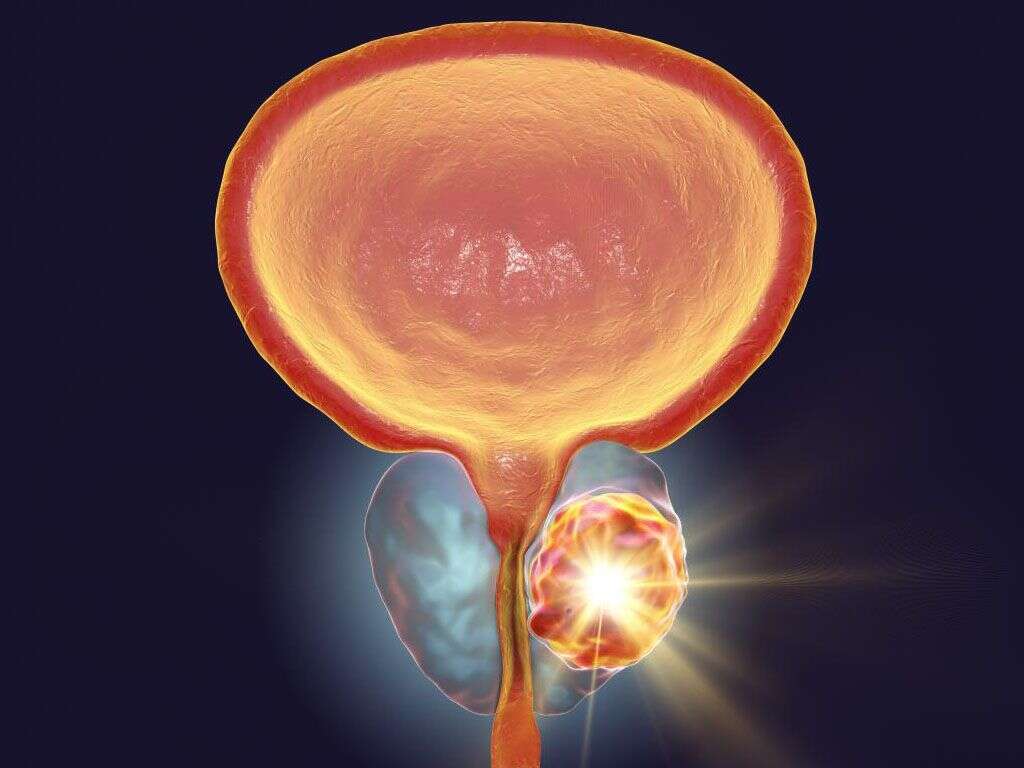
Peyronie’s disease is a condition named after Francois Gigot de la Peyronie, a French surgeon who first described this condition in 1743. This condition is characterized by a curvature in the penile shaft resulting in various issues. It is a connective tissue disorder where there is abnormal growth of fibrous plaques in the penile soft tissue.
Throughout the years, there have been various medications and surgical therapies used in the treatment of this condition. The number of methods proposed is a testament to how ineffective these treatments have been. This condition is due to the presence of scar tissue that affects the connective tissue in the penis. The curvature is usually obvious when there is erection but can be noticeable even when flaccid. The area of fibrosis known as the plaque can vary in firmness and become calcified.

1. Epidemiology
The rate of Peyronie’s disease has been estimated to be about 0.39% to 3%. However, this may be an underestimation as most men are embarrassed regarding this issue. There may also be underreporting due to mild or non-debilitating issues where medical attention is not required.
Although most commonly seen in men between the ages of 40 to 70 years old, there are also other authors that reported these cases among young individuals. In a study involving 4,432 study participants, it was reported that the estimated prevalence by age was 1.5% for those 30 to 39, 3% for men 40 to 49, 3% for men between the ages of 50 to 59, 4% for those 60 to 69, and 6.5% for men above the age of 70 years.

2. Etiology
The cause of Peyronie’s disease is still unclear. It has been associated with the elevation of serotonin levels, vitamin E deficiency, ingestion of beta-blocking agents, Dupuytren contractures, HLA-B7 (genes), vascular trauma, penile injury, and more.
An injury can trigger the release of cytokines activating the proliferation of fibroblasts and production of collagen. Based on an analysis on sociodemographic factors, it was identified that the potential risk factors also include diabetes mellitus, hypertension, systemic vascular diseases, hyperlipidemia, alcohol consumption, smoking, history of nongonococcal urethritis, and the use of propranolol. However, how these risk factors contribute to the condition is still unclear.

3. Presentation
The presentation of this condition can vary. It can progress over several years. Once the fibrosis has calcified, the angle of the curvature stabilizes. Since spontaneous resolution is unlikely, intervention is recommended. Symptoms of Peyronie’s disease include pain in the penis, which becomes more pronounced especially when there is an erection.
The penis can also appear to be angulated. This angulation may only be seen during an erection or in some cases in a flaccid penis. At the site of angulation, a plaque can also be palpable. In some patients, there can be an indentation in the shaft at the site of the plaque resulting in an hour glass deformity. Patients with this condition also have decreased erectile function due to penile buckling or loss of rigidity.

4. Psychosocial Aspects of Peyronie’s Disease
A study has found that about 77% of those with Peyronie’s disease experience psychological effects. In the study involving 245 men, 81% experienced emotional difficulties while 54% attribute their relationship difficulties to this condition.
Those able to have intercourse have less relationship issues. Another study found that 48% of their study participants were depressed. The 6 main themes through a 2008 study were concerns about their physical appearance, sexual self image, sexual function and performance, loss of sexual confidence and decreased feeling of attractiveness, social stigmatization and isolation, performance anxiety, and concern about not being able to sexually satisfy their partners.
5. Investigations
There is no specific blood test that is used for the diagnosis of Peyronie’s disease. Despite an association being made between HLA-B7 surface antigen and Peyronie’s disease, it is not a marker specific for this condition. Using this marker to diagnose Peyronie’s is impractical as the diagnosis can be made via the patient’s history and examination.
Imaging is used to identify calcification of the plaque as this means that the plaque has matured and there will be no longer any further angulation. Some of the imaging that may be used include a plain x-ray, ultrasound of the penis, magnetic resonance imaging (MRI), and a corpus cavernosography. MRI is used when the plaque is composed of fibrous tissue.

6. Further Procedures
If the Peyronie’s disease patient also has associated erectile dysfunction, a duplex ultrasonography with intracavernous injections of a vasoactive agent can be beneficial to help identify the underlying issue. This procedure is popular to assess the extent of the plaque, assess the deformity in the shaft, and penile angulation.
In a study involving 81 men with Peyronie’s disease, it was found that 54% overestimated the degree of curvature, 26% underestimated it, and 20% correctly estimated it to within 5?. This study emphasized that proper measurement of penile angulation is needed to accurately counsel patients and assess treatment outcome.

7. Medical Therapy
The best medical therapy for this condition has yet to be identified. Watchful observation without any intervention is acceptable for those with minimal symptoms and if it does not disrupt sexual function. A study involving 246 patients with Peyronie’s disease found that the condition improved in 12% of patients, unchanged in 40%, and worsened in 48%.
All who initially presented with penile pain have reported improvement with 89% noting complete resolution of pain without any treatment. In the evaluation of a specific therapy, placebo effect should be taken into consideration as some symptoms can spontaneously improve in many patients. Some medications and supplements that have been used are vitamin E supplements, interferon-alpha-2b, and collagenase clostridium histolyticum.

8. Surgery
Surgery is only considered if the patient meets all the required criteria. The type of surgery performed will also depend if the condition is associated with erectile dysfunction and characteristics of the plaque. A discussion with the patient will be required regarding the description of the procedure, goal, risks, percentages of success, and other treatment options.
The patient should be counseled that his penis will no longer appear as it exactly did and that there may be some residual angling. The penis may appear shorter and wider compared to before the surgery. This discussion is essential so the patient has realistic expectations. After the surgery, the catheter can be removed the following morning and the patient can return with oral antibiotics. Follow-up care is generally a week later.

9. Follow-Up, Complications, Prognosis
Follow-up for those on medical treatment is reasonable every 3 months. Those who had surgery should be monitored closely to ensure they heal well. Complications from medical therapy are rare while surgery carries the risk of bleeding, infection, scarring, return of curvature, penile foreshortening, and anesthesia complications. If an incision is necessary under the corpus spongiosum or dorsal neurovascular bundles, there is a change of damage to the structures resulting in permanent sensory loss and loss of erections.
Generally, the outcome of this condition can be judged based on satisfactory sexual functioning and the degree of improvement in plaque and penile curvature. Results are best obtained when the patient’s goal is identified in the early course of treatment.

10. Treatment Contraindications
The contradictions to the treatment of Peyronie’s disease are based on the signs and symptoms. If there is minimal curvature, little to no loss of penile rigidity, and no compromise of function, intervention is contraindicated. This is due to the fact that any intervention is unlikely to improve appearance or function while exposing patients to side effects and worsening of the symptoms. To those with hypersensitivity to a specific agent, oral and topical treatments are contraindicated.
Meanwhile, injectable agents are well tolerated and have little systemic effects as the amounts injected are small. Surgery is also contraindicated for those with minimal symptoms or unstable disease as surgery performed before fibrosis is complete will lead to more plaque and curvature.