What Is Pericardial Effusion?
 Article Sources
Article Sources
- 1. Colombo, A. et al. Etiology and prognostic implications of a large pericardial effusion in men. Clinical Cardiology vol. 11,6 (1988):389-94. doi: 10.1002/clc.4960110606.
- 2. Sagristà-Sauleds, Jaume et al. Diagnosis and management of pericardial effusion. World Journal of Cardiology vol. 3,5 (2011): 135-43. doi: 10.4330/wjc.v3.i5.135.
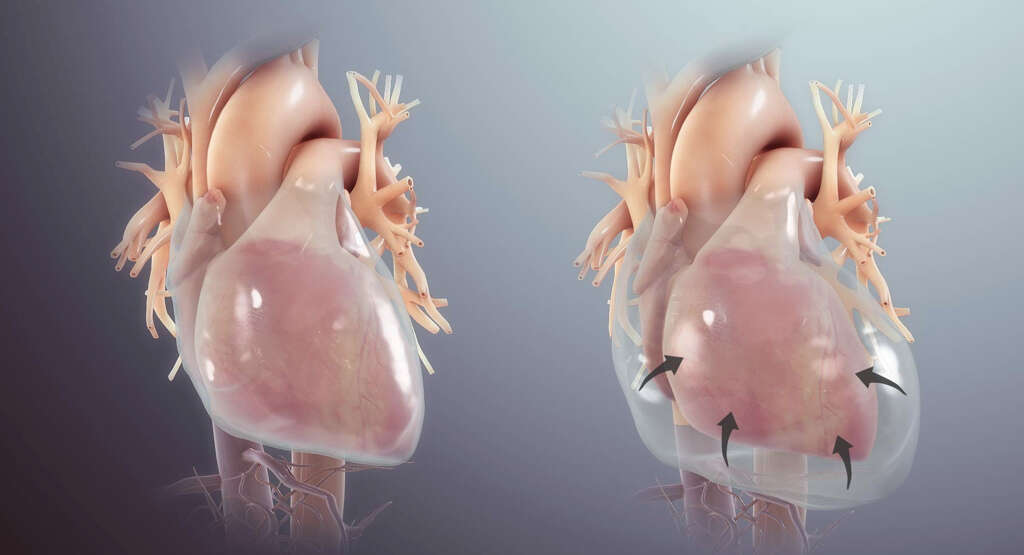
A normal heart is surrounded by a sac called the pericardium, which consists of two thin layers of tissue with a small amount of fluid between them. When the heart beats, this fluid helps to reduce the friction between the two layers of the pericardium.
Sometimes, a buildup of fluid occurs. This is referred to as a pericardial effusion. The excess fluid can inhibit normal heart functioning. The degree of severity can range from mild to acute. Severe cases can lead to heart failure or death when left untreated.

1. Causes
There are a number of potential causes for pericardial effusion. Cancer in the heart or metastasizing cancers from the lungs, breasts or blood can lead to the condition, as can cancer treatments. Autoimmune conditions are also potential factors that can cause a buildup of pericardium fluid, as are kidney failure and hyperthyroidism.
Inflammation, also known as pericarditis, in the pericardium due to an infection, heart attack or heart surgery is a common cause. Idiopathic pericarditis refers to inflammation with an unknown cause, though frequently it is presumed to be from an infection. Idiopathic pericarditis may be the most common cause of severe pericardial effusion in men.1Colombo, A. et al. Etiology and prognostic implications of a large pericardial effusion in men. Clinical Cardiology vol. 11,6 (1988):389-94. doi: 10.1002/clc.4960110606.
2. Risk Factors
Anyone can get pericardial effusion; however, men between the ages of 16-65 are at a higher risk. People who have cancer are more vulnerable to developing the condition due to the number of factors associated with cancer that potentially can cause pericardial effusion.
Those with underlying conditions that have the potential to cause fluid buildup in the pericardium, such as an autoimmune disorder, are more likely to develop this condition. There are also certain medications that increase the risk, including drugs that treat high blood pressure, seizures and tuberculosis.

3. Transmission
Pericardial effusion is not a contagious condition; thus, it cannot be passed from person to person. The underlying condition responsible for pericardial effusion may, however, be contagious. Infections are some of the most common causes.
If the infection is caused by a virus or bacteria, it is likely to be contagious, but contracting the illness from the pathogen does not necessarily lead to pericardial effusion in all people. Other types of infections that can cause the condition, such as those caused by fungi or parasites, are not contagious.
4. Diagnosis
The first step in diagnosing pericardial effusion is a physical exam, which includes listening to the heart for signs of the condition. If the doctor suspects the patient has the condition, imaging and blood tests are ordered to confirm the diagnosis and to determine potential causes. Often, however, the condition is discovered during an imaging test conducted for another reason.
A chest X-ray, echocardiogram and electrocardiogram are all tests that can help determine whether a patient has pericardial effusion and, if so, how severe it is. Blood tests are used to detect the presence of pathogens that cause infections and to look for potential autoimmune and metabolic system deficiencies.

5. Signs & Symptoms
This condition ranges from mild to severe. A small pericardial effusion is indicative of a mild case, while a large one is severe. A majority of those who have pericardial effusion do not have any symptoms, including those with large, chronic pericardial effusion.2Sagristà-Sauleds, Jaume et al. Diagnosis and management of pericardial effusion. World Journal of Cardiology vol. 3,5 (2011): 135-43. doi: 10.4330/wjc.v3.i5.135. This is particularly true when the condition develops slowly, with fluid buildup occurring over time.
If symptoms do occur, it is usually after a significant amount of fluid has accumulated in the pericardium. At this time, the individual may experience chest pain or pressure, generally on the left side. Shortness of breath and difficulty breathing may also occur. Some people notice a feeling of fullness in the chest. There is the potential for swelling to occur in the legs and abdomen.

6. Complications
When there is a significant amount of excess fluid in the pericardium, it can lead to a condition called cardiac tamponade. This is a serious condition that causes pressure on the heart and is a frequent cause of death in people with pericardial effusion. People who have chronic pericardial effusion can be stable for a number of years and then suddenly develop cardiac tamponade.2Sagristà-Sauleds, Jaume et al. Diagnosis and management of pericardial effusion. World Journal of Cardiology vol. 3,5 (2011): 135-43. doi: 10.4330/wjc.v3.i5.135.
Cardiac tamponade prevents the heart from working as it should because it inhibits full expansion of the ventricles during the heartbeat. This reduces blood flow to the rest of the body. It can lead to heart failure, pulmonary edema, shock and death. The condition develops rapidly and requires fast treatment to remove the excess fluid.
7. Treatment & Management
Treatment measures vary according to the severity of the condition as well as the underlying causes. In some cases, if the underlying cause can be treated, then the pericardial effusion is corrected as well. If the individual is not at risk of cardiac tamponade, then medications are often prescribed to reduce inflammation.
When medications are ineffective, or if the individual has or is at risk of cardiac tamponade, other measures are necessary. The most common action taken is to drain the fluid using a catheter. Open-heart surgery may be required when there is bleeding into the pericardium, which can happen as a result of heart surgery.

8. Prevention
In most cases, there is no way to prevent pericardial effusion. However, steps can be taken to reduce the risk for some of the conditions that cause it. Those who lead a heart-healthy lifestyle by eating a nutritious and balanced diet, exercising regularly and limiting alcohol intake are less likely to develop a number of the conditions that contribute to pericardial effusion.
If a person has already had an acute episode, it is possible to reduce the likelihood of another one or of developing a chronic condition. Doing so requires diligent adherence to the prescribed treatment plan and following the cardiologist’s recommendations for medical care.

9. Prognosis
The prognosis for pericardial effusion depends largely on the underlying cause and the severity of the condition.2Sagristà-Sauleds, Jaume et al. Diagnosis and management of pericardial effusion. World Journal of Cardiology vol. 3,5 (2011): 135-43. doi: 10.4330/wjc.v3.i5.135. Individuals who have lung cancer or malignant cells within the pericardium have a poor prognosis.2Sagristà-Sauleds, Jaume et al. Diagnosis and management of pericardial effusion. World Journal of Cardiology vol. 3,5 (2011): 135-43. doi: 10.4330/wjc.v3.i5.135. Those who develop cardiac tamponade are at high risk for a poor outcome.
People who have a small effusion generally do not experience any complications. The prognosis for those who have idiopathic pericarditis and chronic pericardial effusion is good, though there is a risk of cardiac tamponade with a chronic condition.2Sagristà-Sauleds, Jaume et al. Diagnosis and management of pericardial effusion. World Journal of Cardiology vol. 3,5 (2011): 135-43. doi: 10.4330/wjc.v3.i5.135. Getting treatment for underlying conditions, such as infections, results in positive outcomes.

10. When to See a Doctor
If you experience chest pain that does not subside within a few minutes, call 911 immediately. Shortness of breath, increased heart rate, chest pain or discomfort, fainting and enlarged veins in the neck are all signs that you may have a severe case of pericardial effusion.
If you develop any of the signs of pericardial effusion, it is important to make an appointment with your doctor. Once the symptoms develop, treatment becomes necessary. Without addressing the condition, you put yourself at risk of a life-threatening emergency.