What Is Osteoporosis?
 Article Sources
Article Sources
- 1. Ganesan K, Jandu JS, Roane D. Osteoporosis (Secondary) [Updated 2020 Jun 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470166/
- 2. Pouresmaeili F, Kamalidehghan B, Kamarehei M, Goh YM. A comprehensive overview on osteoporosis and its risk factors. Ther Clin Risk Manag. 2018;14:2029-2049. Published 2018 Nov 6. doi:10.2147/TCRM.S138000
- 3. Varacallo M, Seaman TJ, Jandu JS, et al. Osteopenia. [Updated 2020 Apr 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499878/
Bones typically break from a high impact trauma. But what about when a bone breaks from a not so traumatic experience? A break that occurs because of an underlying condition is called a “pathological fracture” and often it is due to a bone disorder called osteoporosis.
Osteoporosis is a common disorder that causes bones to become brittle and to fracture more easily. About 20-25 million people are affected in the United States.1Ganesan K, Jandu JS, Roane D. Osteoporosis (Secondary) [Updated 2020 Jun 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470166/ It can be caused by a variety of ailments and, depending on the reason it is occurring, can be classified as primary or secondary. There is a spectrum to osteoporosis with osteopenia being the precursor. Once diagnosed, there are well-studied treatments to help build the bone density back up.

1. Primary and Secondary Osteoporosis
A diagnosis of osteoporosis can be categorized as primary or secondary. Primary osteoporosis is more common and is due to age-related changes of the body. For example, the hormonal changes that occur in postmenopausal women may cause a decrease in bone density. Another cause of primary osteoporosis is a deficit in the body’s ability to utilize the minerals to keep bones strong.
Secondary osteoporosis is due to some underlying disease or condition. These underlying causes include, but are not limited to, hormonal issues, problems with the digestive system, disorders having to do with blood, autoimmune disorders, a disease of the kidneys, or certain medications.1Ganesan K, Jandu JS, Roane D. Osteoporosis (Secondary) [Updated 2020 Jun 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470166/

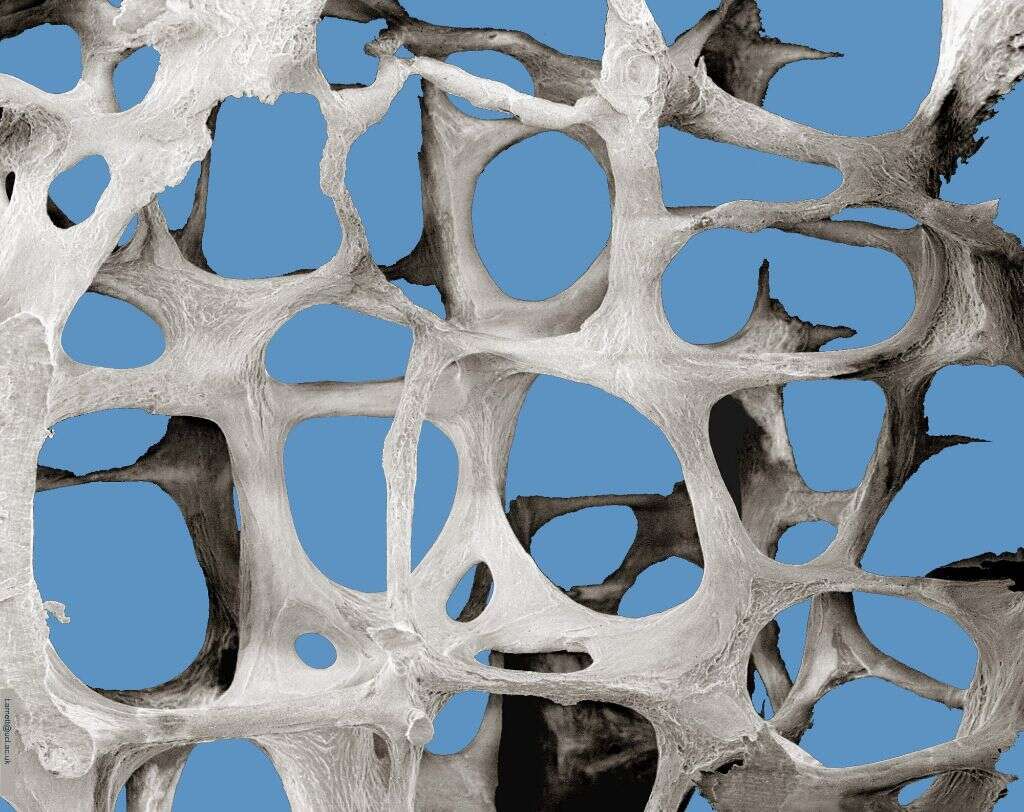
2. Normal Bone
Although bone is very strong, it is a living and ever-changing tissue within our bodies. It relies on the balance of a certain kind of cellular activity. This cellular activity works to break down bone (called resorption) and to build it back up (called formation). But why would the body want to break down bone? Bone is a natural storage place of minerals. When the body is in need of one of these minerals then the breaking down of bone to release the mineral occurs more. When the body has enough of a certain mineral then they will be stored back into the bone.
A healthy balance of these minerals in the body allows for ideal bone remodeling. The cells use vitamins and minerals such as calcium, vitamin D, phosphate, sodium, and magnesium to perform this function. This intricate process also relies on certain hormones that lets these specialized cells know if the body needs more or less of a mineral.
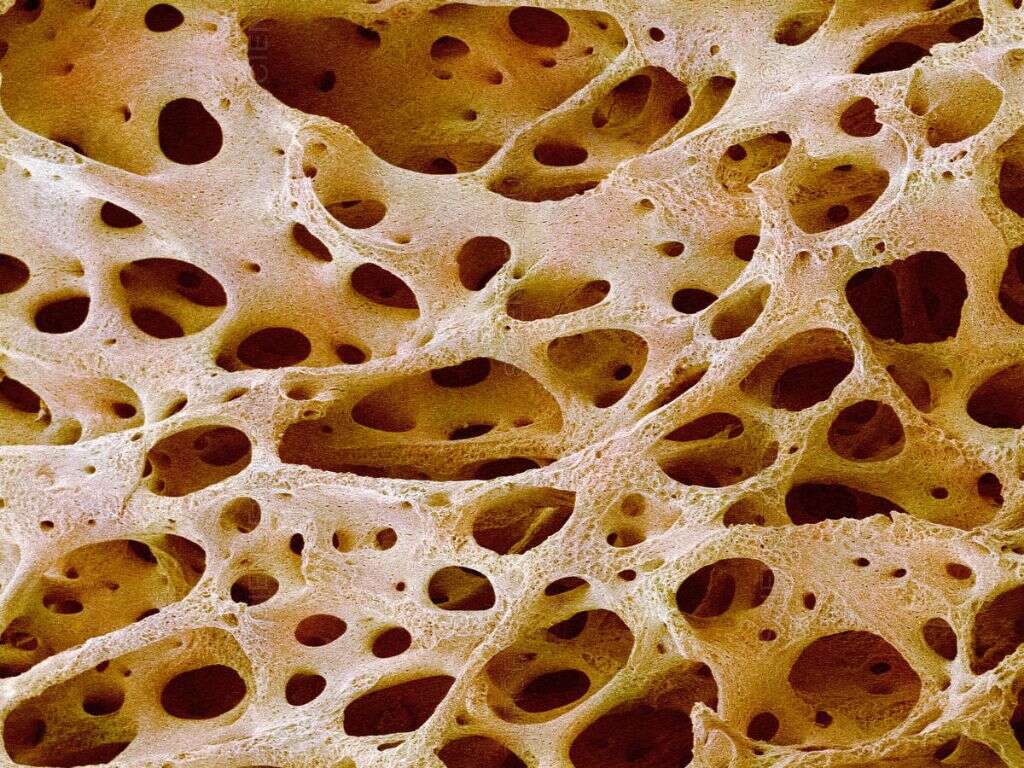
3. Osteoporotic Bone
In the case of osteoporotic bone, the balance of bone breakdown and build bone up is disrupted. Earlier in this article some causes of osteoporosis were mentioned. If a certain hormone is out of whack or if the right minerals are not being absorbed into the body, then bone breakdown will occur.
The breakdown of bone tissues causes a decrease in the density of the bone causing it to be more fragile and more at risk to fractures. Fractures of osteoporotic bone will tend to occur in the spine, hips, or the forearm.1Ganesan K, Jandu JS, Roane D. Osteoporosis (Secondary) [Updated 2020 Jun 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470166/
4. Risk Factors, Signs, and Symptoms
The tricky thing about osteoporosis is that there are really not any obvious symptoms until a fracture occurs. Knowing the risk factors of osteoporosis, screening, and prompt treatment are the best ways to catch osteoporosis early. Ideally, it would be best to catch osteoporosis in its precursor stage, called osteopenia, or to avoid osteopenia/osteoporosis all together if possible.
Some risk factors of osteoporosis include poor nutritional absorption in the digestive tract, sedentary lifestyle, being underweight, smoking, alcohol, pollution, and stress. Other factors include age, frequent falling, gender, being of White race, family history, and certain underlying medical conditions as mentioned above.2Pouresmaeili F, Kamalidehghan B, Kamarehei M, Goh YM. A comprehensive overview on osteoporosis and its risk factors. Ther Clin Risk Manag. 2018;14:2029-2049. Published 2018 Nov 6. doi:10.2147/TCRM.S138000
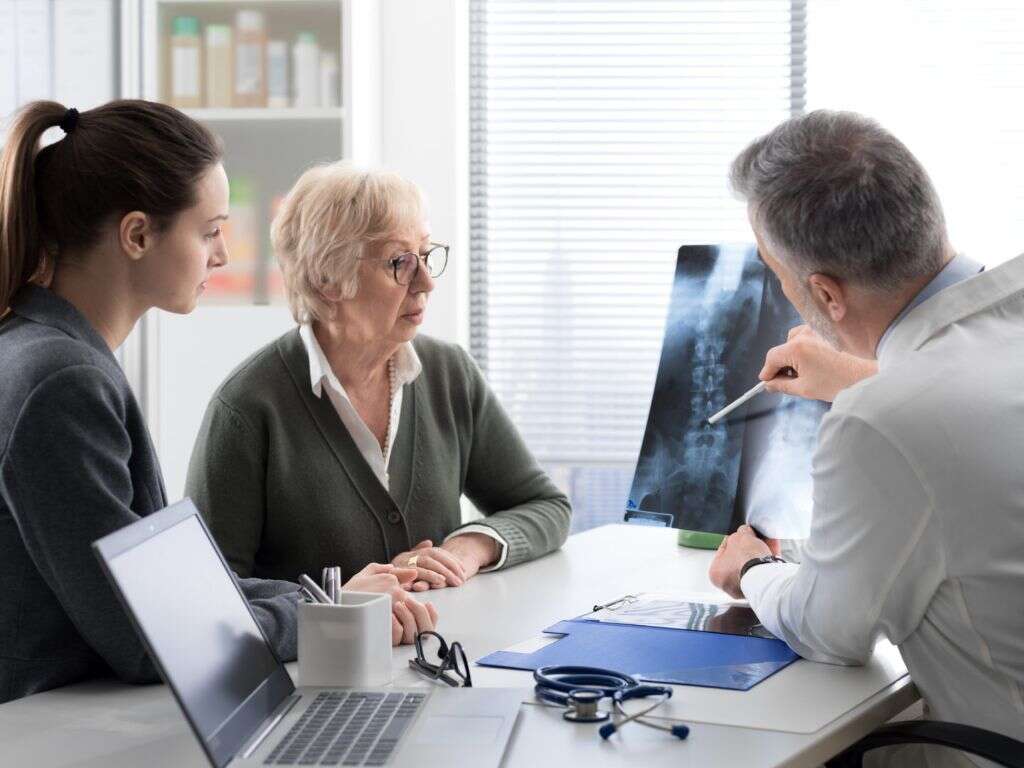
5. Evaluation and Diagnosis
The presence of osteoporosis will be evaluated by a doctor and the key is to diagnose it early before a bone fracture occurs. The underlying cause of their suspicion for osteoporosis will guide exactly what they will be looking for. They could do tests on blood, hormones, minerals, certain markers for bone resorption and formation, etc. If a fracture is suspected the doctor will order an x-ray.1Ganesan K, Jandu JS, Roane D. Osteoporosis (Secondary) [Updated 2020 Jun 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470166/
The diagnosis of osteoporosis is made by using a dual energy x-ray absorptiometry (DXA) bone scan. This scan measures the ‘T-score’. If this score comes back less than or equal to -2.5 with the presence of a fracture due to minimal trauma, then a diagnosis of osteoporosis is made.1Ganesan K, Jandu JS, Roane D. Osteoporosis (Secondary) [Updated 2020 Jun 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470166/

6. Differential Diagnosis
‘Differential diagnosis’ is a term used to describe other diagnoses that could be possible besides the diagnosis that seems to be the most likely. What diagnoses make the list depend largely on the patient’s history, signs, and symptoms. When making a diagnosis, doctors consider this list so that they may order the correct tests to come to the correct diagnosis.
A differential diagnosis list for osteoporosis may include: osteomalacia, lymphoma, mastocytosis, sickle cell anemia, multiple myeloma, Paget disease, osteonecrosis, infection, homocystinuria, scurvy, homocysteinemia, and metastatic bone disease.1Ganesan K, Jandu JS, Roane D. Osteoporosis (Secondary) [Updated 2020 Jun 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470166/
7. Medical Treatment
Treatment will depend on the underlying cause. Once the cause is established, corrective measures can be taken to avoid further progression of osteoporosis. Measures may include medication, diet, lifestyle modifications, among others.
While underlying causes are being treated, bone density itself will also be treated. Medications that promote bone formation and slow the breakdown of bone may be prescribed by a doctor. Calcium and other supplements may also be prescribed.2Pouresmaeili F, Kamalidehghan B, Kamarehei M, Goh YM. A comprehensive overview on osteoporosis and its risk factors. Ther Clin Risk Manag. 2018;14:2029-2049. Published 2018 Nov 6. doi:10.2147/TCRM.S138000 Medical treatment is not the only way to address or prevent osteoporosis. Living a certain lifestyle is important and described more in the next section.

8. Other Treatment and Management
Exercise is a great way to not only strengthen osteoporotic bone but to also prevent osteoporosis in the first place. Exercise should include weight bearing and resistance exercises. Examples of weight bearing exercises include walking and step aerobics while resistance exercises include weight lifting and theraband activities. Pilates and water aerobics have also been found to be beneficial.
These types of exercises put stress on the bone which will promote the cells to strengthen the bone. The key is finding the right dosage - enough stress but not too much to cause fracture. A Physical Therapist is an excellent healthcare provider to help a person with osteoporosis to find the most fitting exercise for the individual patient.

9. Prognosis
The term ‘prognosis’ used to describe the likely outcome of a diagnosis. When diagnosed and treated correctly in the early stages, the prognosis of osteoporosis is quite good. If osteoporosis progresses to a point of extreme fragility, the prognosis becomes poorer. The underlying cause of osteoporosis will also affect the prognosis. The prognosis is better for an easily treatable cause vs. a cause that is not easily treatable.
Collaborating with a healthcare team will help to improve the outcome of being diagnosed with osteoporosis. It is important for the individual to understand how their own choices will affect their prognosis.

10. Osteopenia
Osteopenia has been mentioned a few times in this article. It is the precursor (or less intense version) to osteoporosis and is diagnosed with the same scan as osteoporosis: a dual-energy x-ray absorptiometry (DXA) bone scan. This scan measures what is termed the “T-score”. If this score is between -1 to -2.5 then the diagnosis of osteopenia is made.3Varacallo M, Seaman TJ, Jandu JS, et al. Osteopenia. [Updated 2020 Apr 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2020 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499878/
There are no signs or symptoms of osteopenia and so early detection with the knowledge of risk factors is important. Treatment is usually pretty conservative but follows the same idea as osteoporosis: weight bearing and resistance exercises, maybe supplementation, and perhaps medication. It will be up to a doctor guided by the most recent evidence as to how to best treat both osteoporosis and osteopenia for the individual person.










