What Is Osteomyelitis?
Under the right circumstances, an infection can occur in any area of your body. If pathogens reach very deep tissues, they can take hold and start multiplying themselves, which causes you to experience symptoms of infection.
Osteomyelitis is an infection that occurs in the bone. Though rare, it can cause potentially serious complications. If it is severe enough and other treatment options have not been successful, you may require an amputation. However, thanks to research into the condition, other treatment options are usually effective, especially if the infection is caught early on.

1. Prevalence
Osteomyelitis affects only about two out of every 10,000 people, making it extremely rare. It can occur at any age, although adults and children may experience it differently. In children, it is more likely to occur acutely and affect the long bones of the arms and/or legs. Adults are more likely to have osteomyelitis that develops over time and affects the vertebrae, hips, or feet.
Osteomyelitis can affect both males and females. There is no race or ethnicity that is more susceptible to it than others. However, other conditions, such as sickle-cell disease or diabetes, can put you at greater risk for osteomyelitis. People from certain races may be at greater risk for these conditions.
2. Symptoms
Systemic symptoms of osteomyelitis may include fever, chills, nausea, fatigue, and malaise, which is a general ill feeling of discomfort. Other symptoms may be localized to the area of the infection, which may be painful, red, or swollen. It may be warm to the touch. If there is an opening in the skin, pus may drain out.
The symptoms of osteomyelitis may depend on the specific bone that is affected. For example, if it affects a bone of your leg, it could cause you to limp. If it affects your hip, you may experience a decreased range of motion. If it affects the spine, you may have severe back pain.

3. Causes
A bacterial infection is often behind a case of osteomyelitis, with Staphylococcus aureus being the most common cause. However, osteomyelitis can also be caused by a fungal infection. Osteomyelitis either starts in the bone itself or results from an infection that spreads to the bone from elsewhere in the body.
Surgery on a bone or joint can cause an infection that results in osteomyelitis. A bone can also be exposed to bacteria due to a chronic wound in the skin, a puncture that extends down to the bone or adjacent tissues, or a fracture that pushes a fragment of the bone through the skin, exposing it to the air.
4. Risk Factors
Conditions that compromise the immune system, making it more difficult for your body to fight off infection, can put you at greater risk for osteomyelitis. HIV is one example; another is uncontrolled diabetes. The risk of osteomyelitis is greater in people with diabetes because it often causes ulcers in the skin of the feet through which bacteria can get in and infect the bones of the lower extremity.
You may be at greater risk for bacteria entering your body if you have a condition requiring frequent catheterization, such as kidney disease. You could also be at greater risk if you have recently had orthopedic surgery or use illicit drugs intravenously.
5. Complications
If there is an infection in a bone, it can sometimes spread to a nearby joint. This can cause septic arthritis, a serious and painful condition. When osteomyelitis occurs in children, it can impair normal growth. Osteomyelitis is sometimes associated with an open, draining sore in the skin. The tissue surrounding this area is more vulnerable to skin cancer of the squamous cells.
One of the most serious complications is osteonecrosis, or bone death. This can occur when the infection impedes circulation within the bone, cutting off the blood supply to a certain area. Once osteonecrosis has set in, the only treatment option available is to remove the area of dead bone tissue.

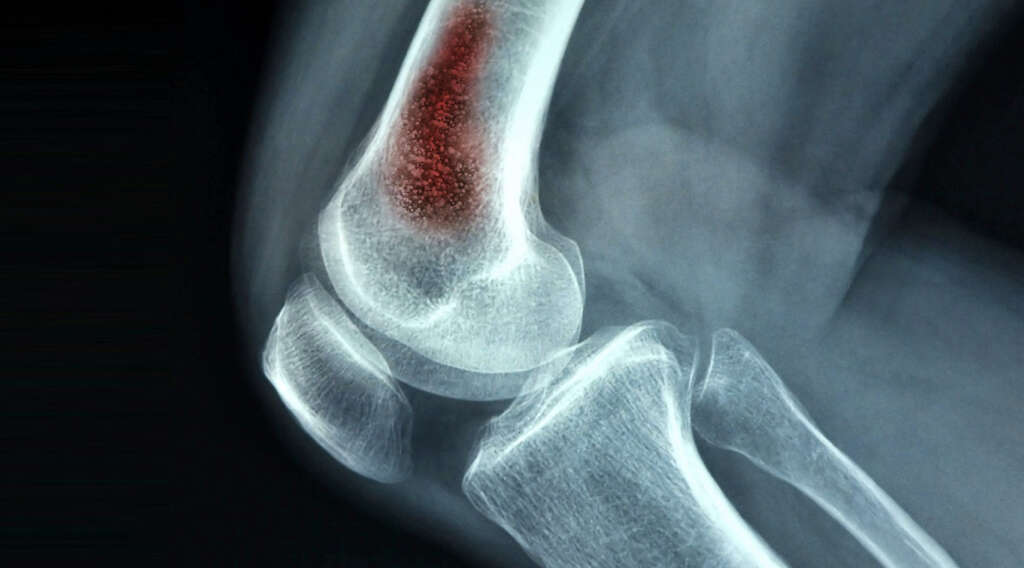
6. Diagnosis
Following a physical examination to assess the area of pain, diagnosis of osteomyelitis may begin with a blood test or blood culture. The former looks for signs of infection, such as an elevated level of disease-fighting white blood cells. The latter detects bacteria in the bloodstream and can determine the pathogen involved.
Imaging exams such as MRI or X-ray can identify damage to the bone due to osteomyelitis. Sometimes your doctor performs a procedure to take a sample of tissue from the infected bone. The sample is then sent to a lab and tested for the presence of foreign organisms. This test is called a biopsy.

7. Antibiotic Treatment
Through tests such as biopsy and blood culture, your doctor may identify the type of bacteria or fungus that is causing your osteomyelitis infection. This is important because it informs which type of antibiotics your doctor can use to fight the infection.
Antibiotic therapy is often the first line of treatment for osteomyelitis. Your doctor may perform a culture and sensibility test to see which medications are effective at killing the pathogens. Because the infection occurs deep in the body, you may have to receive the antibiotics intravenously at first. Later, your doctor may switch you to oral antibiotics.

8. Surgical Treatment
Surgical treatment of osteomyelitis becomes necessary if antibiotic treatment alone is not effective. The main goal of surgical treatment for osteomyelitis is to prevent it from spreading any further. Rarely, if the infection is severe enough and cannot be controlled any other way, the only option is to amputate the entire limb.
Fortunately, amputation is only necessary in the most severe cases of osteomyelitis. Usually, it is only necessary to remove the area of the bone damaged due to osteonecrosis. To ensure complete removal of infected bone, the surgeon also takes a small margin of healthy tissue. You may have a graft later to replace the tissue that was removed.

9. Prevention
You can protect yourself from osteomyelitis by taking steps to prevent open wounds, such as scratches, scrapes, or cuts. It may not be possible to avoid all such injuries, but if you do get a cut or scratch, you should cover it with a bandage after cleansing it carefully and thoroughly.
It is especially important to prevent osteomyelitis if you are at an increased risk of infection. Talk to your doctor about any more specific preventative measures you could be taking.

10. Outlook
Osteomyelitis was once considered incurable. Fortunately, research has expanded doctors’ understanding of both the condition and effective means of treating it. Therefore, it is possible to treat most cases of osteomyelitis successfully without resorting to amputation.
The chances of recovery from osteomyelitis are better the earlier it is caught. It is harder to treat the infection once it becomes acute. Therefore, you should discuss any systemic symptoms of infection or wounds that won’t heal with your doctor as soon as possible.