What Is Infantigo?
Focusing on your health can take many forms. Though the skin covers the human body and protects it from an array of threats, it is also susceptible to a number of conditions. Infantigo, more commonly known as impetigo, is a type of skin infection that is usually caused by bacteria. It often impacts the face, as well as the skin found along the arms and legs. Medical experts state that impetigo predominantly impacts children under the age of five, but adults of any age can still contract the infection.
Knowing the difference between a normal rash and a skin condition that requires medical attention can be tricky. Learn more about this condition to gain a better idea of how to spot infantigo.

1. What Are the Types of Infantigo?
In a number of impetigo cases, the exact kind of bacterial skin infection an afflicted individual develops determines the classification of infantigo and subsequent treatments. “Primary impetigo,” for example, infects skin cells that otherwise seem healthy. “Secondary infantigo,” on the other hand, is an infection that takes place around broken skin and wounds.
Distinguishing between primary and secondary infantigo is best determined by a dermatologist or skin care professional. They can provide a diagnosis and offer a number of treatment options based on the specifics of your case.

2. How Does Infantigo Develop?
Infantigo is a condition that has persisted for many centuries. The first recorded cases of modern impetigo date to somewhere in England in the 1300s. Since an understanding of bacterial infections would not develop for several hundred years, medical professionals of the time often classified infantigo as an “attack” upon the skin.
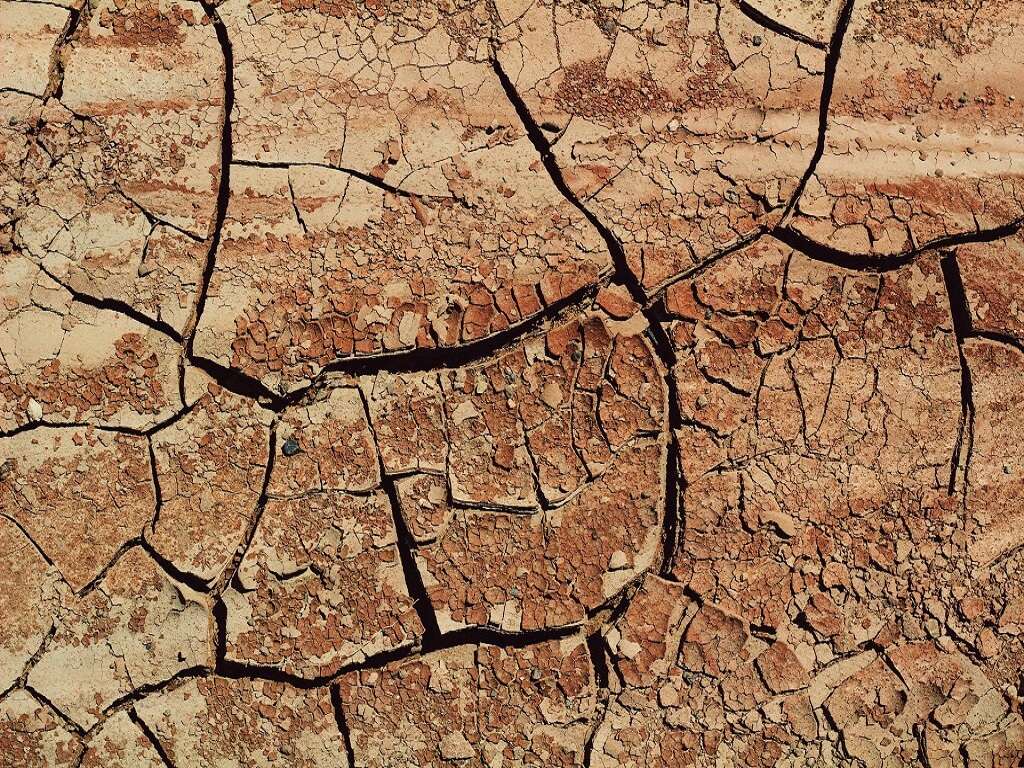
The spread of the infected skin occurred fast, especially in hot climates where the bacteria of the infection could thrive. Even now, warm environments are still the most common for encouraging the spread of bacterial infections like impetigo.

3. What Environmental Conditions Cause Infantigo?
The bacteria that causes impetigo is typically contracted due to a combination of environmental and circumstantial factors. Skin abrasion tends to increase the odds. Even minor scratches and insect bites can cause a person to develop an infection after the broken skin is exposed to an environment containing bacterial strains like staph or strep.
Towels and other common items can also act as breeding grounds for the bacteria and increase the odds of exposure and infection. Medical experts mention these bacteria is most likely to develop during the warmer months but can be a year-round threat in consistently hot climates.

4. What Are Common Symptoms of Infantigo?
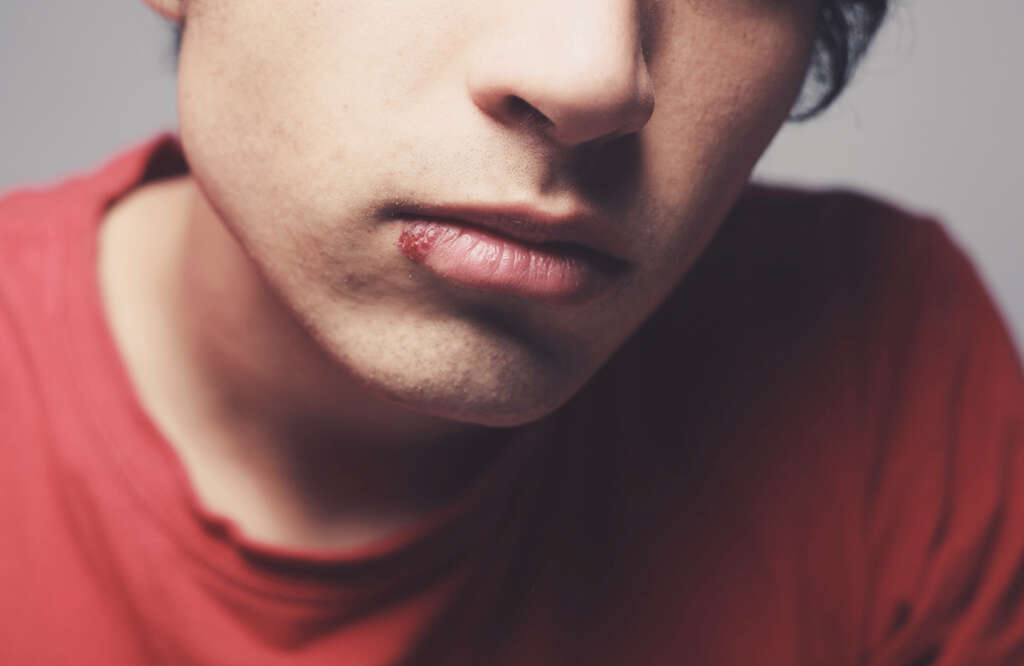
Since impetigo is a skin condition, a number of the symptoms indicating this infection are easy to notice. One of the earliest warning signs of infantigo is discoloration of the skin. Specifically, it manifests as red sores localized around the lips and nose.
As these sores grow, they become blisters that may ooze or break and can be quite painful. They are persistently itchy and scratching at them makes the symptoms worse. The arms and legs can also develop these sores in addition to or instead of on the face.
5. How Does Infantigo Impact Adults?
As is the case with many conditions, adults who contract an infection like Infantino are likely to experience different symptoms than children. Adults are more likely to spread the infection at a faster pace if they play sports, work in small offices, or live in a residence with many other people.
An adult with infantigo has a higher risk of developing complications such as sepsis and cellulitis. The faster the infection is seen by a dermatologist or medical expert, the easier it is to control the spread and reduce the odds of exacerbating other ailments.

6. How Does Infantigo Impact Children?
Infantigo is most common among children between the ages of two and five. Unlike adults, who are most likely to show indications of the infection around the lips and face, children first show symptoms around the legs. Specifically, these bacteria are likely to invade around the diaper area.
Since it can look like common diaper rash at a glance, you’ll want to pay close attention when changing a child and noticing discoloration or redness around the legs and trunk. Children often spread the bacteria around their own bodies at a fast pace by scratching at infected sites.

7. What Are the Different Forms of Infantigo?
There are several different types of infantigo, classified by the specific strain of bacteria and the infection’s progress. The three main forms are non-bullous impetigo, bullous impetigo, and ecthyma.
Unlike bullous and non-bullous forms, which are diagnosed according to the bacterial strain, ecthyma is what occurs when infected sites are not treated. At this stage, sores have blistered beyond the point of discomfort and will ooze blood and pus when dried, crusted skin breaks from the pressure. Since most people see a healthcare professional during the non-bullous or bullous stages, cases of ecthyma are rare.

8. Can the Spread of Infantigo Be Prevented?
Infantigo is highly contagious. When a person reaches the stage of the infection where sores have blistered and opened, it is at its most contagious point. Children and adults who have been diagnosed with this infection need to remain at home and avoid all physical contact with others until the wounds have healed.
Once the infection clears from treatment and time, a normal routine can be resumed. Additional steps may be required depending on the severity of the infection, but isolation is always the best way to limit the spread of this infection.

9. Do Good Hygiene Habits Prevent Infantigo?
Though it can be unavoidable in a number of cases, health experts believe that the odds contracting these bacteria can be reduced by following proper hygiene habits. Regularly washing your hands with soap throughout the day helps to keep any possible open sores on your hands clean and can cut down on the presence of skin bacteria.
Cover any cuts or open sores on your hands and exposed areas with adhesive strips until fully healed, and avoid scratching at any dry or itchy spots. Good hygiene is an invaluable preventative step for an array of common health conditions, including infantigo.

10. How Is Infantigo Treated?
Upon being diagnosed with infantigo, antibiotics are usually prescribed. What you are administered depends largely on the type of infection and the stage that it is currently at. Skin creams and other topical options may also be offered to help handle the symptoms of the condition like pain and itchiness.
On average, infantigo that has been treated will heal somewhere within 10 days. This period can be elongated in cases where other health conditions delay or impact the rate at which the body responds to the antibiotics. Your doctor can provide a detailed explanation of what to expect.