What Is Hypoventilation?
There are few things as naturally pleasurable and reassuring as being able to take a deep breath of fresh air and fill your lungs with clean oxygen. This sensation is even more heightened when it comes after some exertion like running or hiking. With all the endorphins kicking in and a positive sense of well-being, it feels good to be alive.
However, this feeling is not always achievable when your respiratory system is not operating optimally. Hypoventilation is a condition whereby there is a decreased level of oxygen and elevated level of carbon dioxide in the blood. This is brought on by limited amounts of air entering into the alveoli in the lungs. Let us look at some key facts that will help explain how and why this happens.
1. Ventilation
Enjoying a deep drag of air is actually partaking of a biological activity that is facilitated by the inner workings of your lungs. As you breathe in, you pull oxygen-rich air into your lungs. At the same time, blood that has circulated around the body is delivering carbon-dioxide rich blood to the same lungs. At the pulmonary capillary bed, an exchange takes place. Carbon dioxide is expelled and oxygen absorbed. When hypoventilation occurs, there is low absorption of oxygen that causes carbon dioxide to buildup in the blood. This is technically described as an elevated arterial carbon dioxide tension (PaCO2).
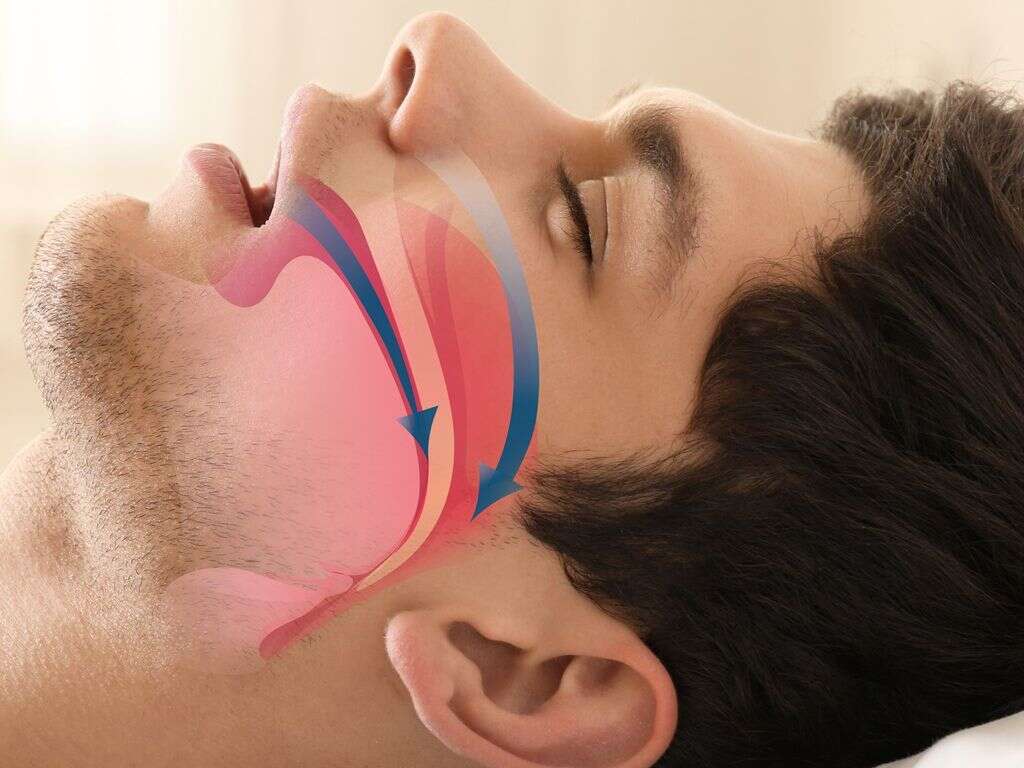
2. Hypopnea
Narrowing of passages that deliver oxygen to the lungs is a possible reason for hypoventilation. For those that suffer hypopnea, their airways become restricted during sleep, leading to a condition known as obstructive sleep apnea-hypopnea syndrome. This happens because muscles at the back of the throat relax too much and collapse in on themselves.
This narrows the airway and reduces oxygen flow to the lungs. Sleep studies have shown that those who suffer this condition will often experience disruption to their breathing for as much as 30 seconds. The lack of oxygen then triggers the brain to waken the person so they can adjust and breathe again.

3. Central Sleep Apnea
Though similar sounding to the above, this condition is somewhat different. Here, it is the brain that is at fault. It fails to send appropriate signals to the muscles that control breathing. There are several reasons why this might occur. Some medications have side effects that may affect the speed and regularity of breathing.
Those that suffer cardiac problems like stroke and congestive heart failure may also endure similar irregularities in breathing. This is particularly dangerous as an extended period of low oxygen levels in the blood can worsen heart cardiac conditions. Exposure to high altitudes where the air is thinner can also trigger this sleep apnea.

4. Bradypnea
While the previous conditions do occur while sleeping, bradypnea can occur when the person is awake. It is defined as having an abnormally slow breathing rate. Ideally, an adult should be able to carry out 12-20 breaths per minute while at rest. A below-normal rate may be caused by opioid use and sedatives.
Some drugs disrupt signals that are relayed between the brain, nerves, and muscles. A hormonal imbalance brought on by thyroid problems can also slow down certain body functions including breathing. Bradypnea has also been linked to incidents of head injuries, lung diseases, and some nerve conditions like ALS.

5. Dyspnea
Shortness of breath or labored breathing is something most are familiar with. For some, it may be due to some underlying medical condition, while for others it could be after a particularly strenuous workout session. In the latter case, recovery should be quick. For those that suffer from this chronically, it can give the feeling that they are suffocating.
Some conditions that can lead to the prolonging of this problem include obesity, heart disease, and lung disease. Other short-term situations that can trigger temporary dyspnea include stress, low blood pressure, heart failure, and carbon monoxide poisoning. It can also occur due to an injury that leads to rapid blood loss.

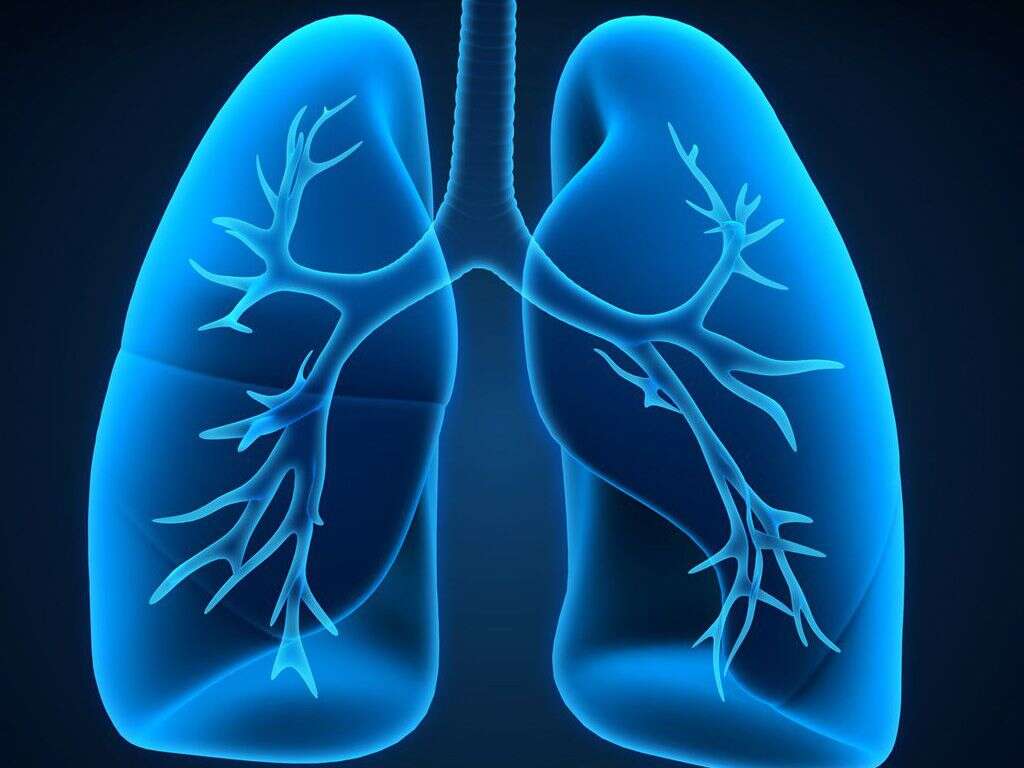
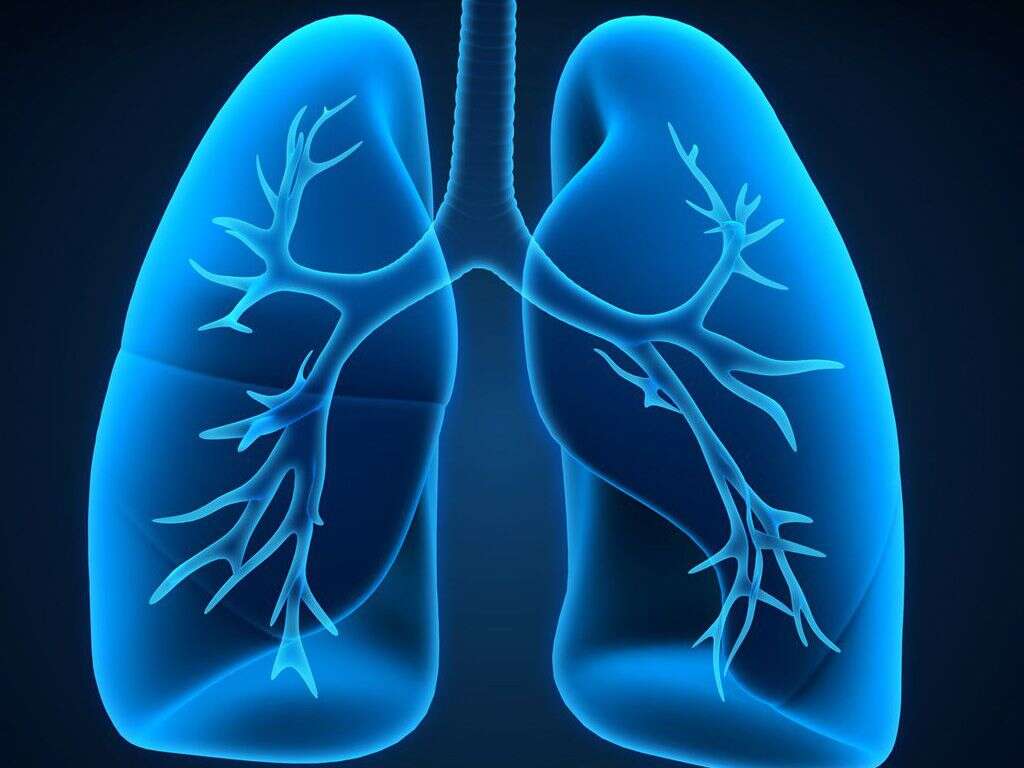
6. Chronic Obstructive Pulmonary Disease (COPD)
The lungs are the meeting point for oxygen, carbon dioxide, and blood. When this pair of organs is ill, it can certainly affect breathing and oxygen absorption. COPD covers a variety of progressive lung diseases the compromise the body’s ability to ventilate properly.
Tobacco use and prolonged exposure to chemicals are leading contributors to the development of these conditions. Emphysema is one of the most common COPD conditions. It damages air sacs in the lungs, making it difficult to exhale. Bronchitis is another common COPD that inflames bronchial tubes causing mucus to buildup. These conditions typically have no cure, merely management of the symptoms.
7. Congenital Central Hypoventilation Syndrome (CCHS)
This disorder affects people who hypoventilate due to an impairment in their nervous system. It is believed to be brought on by gene mutations that affect the autonomic nervous system. This system is responsible for controlling several bodily functions including breathing and regulating heartbeat. This syndrome can disrupt breathing both day and night, or just at night.
Many patients are diagnosed early in life. Parents of children with the condition will have observed a bluish tinge to their baby’s lips brought on by the lack of sufficient oxygen during sleep. This problem is often accompanied by other symptoms such as irregular heartbeat, low blood pressure, and low body temperature.

8. Restrictive Thoracic Disorders
These conditions are caused by reduced lung capacity. The ability of a person’s lungs to expand when inhaling is limited, which means a limited amount of oxygen can be drawn into the lungs, leading to hypoventilation. This can be as a result of a disease affecting the chest wall or other parts of the thoracic cavity.
The majority of these diseases tend to be progressive, meaning they can be expected to get worse with time. Some common restrictive disorders include lung cancers, tuberculosis, and pneumonia. It can also be influenced by conditions outside the lungs like scoliosis, obesity, and pleural effusions.
9. Obesity
Obesity has been mentioned under several conditions above because it not only increases the development of related illnesses but also is itself a danger. Obesity hypoventilation syndrome occurs when there is an excessive buildup of fat around the neck and abdomen area. This can affect airflow and make for labored breathing.
Being obese can also disrupt hormonal levels that in turn affect breathing function. Besides sleep apnea, patients may also experience daytime drowsiness, fatigue, and headaches. Weight loss is often effective in resolving this problem. Other interventions can include the use of a CPAP machine to aid in continuous breathing when sleeping.

10. Sudden Infant Death Syndrome (SIDS)
The sudden unexplainable death of an infant can make the parents question every action they have ever undertaken and wonder if that is what caused the tragedy. SIDS is a condition that is plagued by numerous myths and false assumptions. One such assumption has been that CCHS may be responsible. In reality, some cases of SIDS may simply be undiagnosed cases of CCHS.
The gene mutation that causes CCHS was not found to be present in many cases of SIDS, disqualifying it as a cause. Sadly, the cause of SIDS has yet to be definitively identified. The safest preventative approach remains to follow best practices like creating a safe sleeping environment, getting vaccinated, and room sharing with the baby.