What Is Hypercapnia?
The term “hypercapnia” can be defined as abnormal elevation of carbon dioxide levels in the blood. “Hyper” translates to “too much” in Greek while “kapnos” means “smoke.” Hypercapnia can also be known as carbon dioxide retention or hypercarbia.
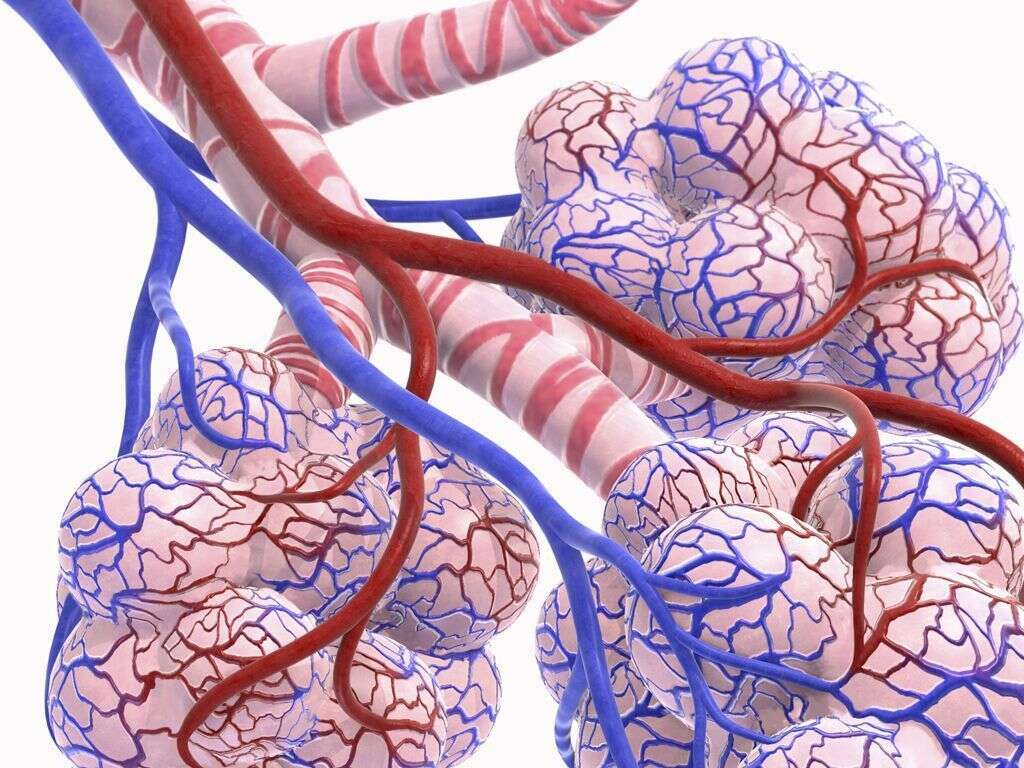
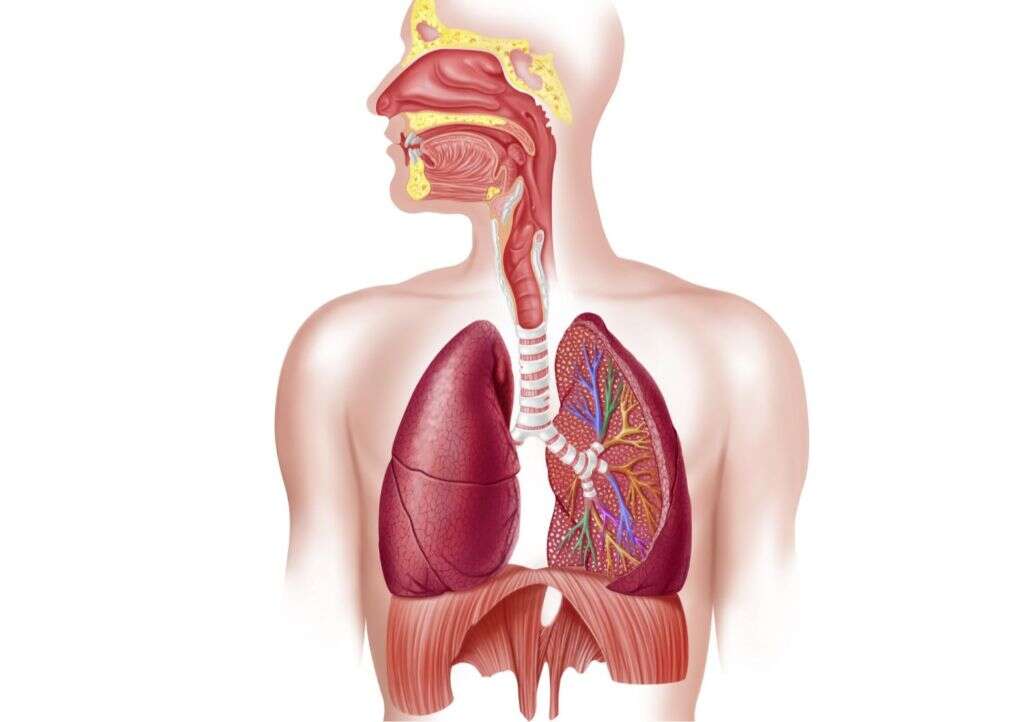
Due to the metabolism in the body, carbon dioxide is expelled through the lungs. In conditions where there is reduced clearance of air from the alveoli, carbon dioxide accumulation can occur. When this occurs, there can be respiratory acidosis causing the body the compensate for the increasing acidity.

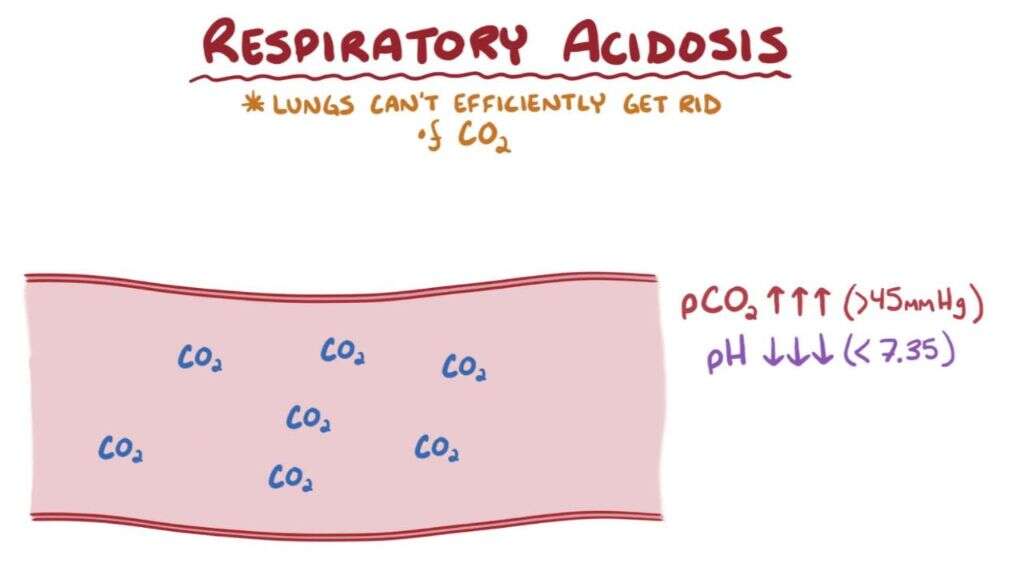
1. Respiratory Acidosis
Respiratory acidosis is a condition where there is decreased ventilation, resulting in the increased concentration of carbon dioxide in the blood. The accumulation of carbon dioxide in the blood decreases the pH of the blood, making it more acidic. Hence, it is known as acidosis. As respiration continues, carbon dioxide is produced and accumulates rapidly if the lungs are unable to expel it. Due to this, hypercapnia occurs. Respiratory acidosis can be divided into acute and chronic. Acute acidosis occurs when there is abrupt ventilation failure due to depression of the respiratory center (in the brain), or neuromuscular disease. Chronic acidosis can occur in various disorders such as COPD, obesity hypoventilation syndrome, neuromuscular diseases, and interstitial lung disease.
2. Signs and Symptoms
Hypercapnia usually occurs due to an underlying health condition. Some of the specific symptoms in early hypercapnia include breathlessness, confusion, lethargy, and headache. The patient may appear flushed, have rapid breathing, twitching muscles, have a bounding pulse, premature heart beats, and asterixis (hand flapping).
It is important to realize that the signs and symptoms may be confusing especially if there are underlying conditions. When severe hypercapnia occurs, patients can experience more severe symptoms such as panic, disorientation, convulsions, hyperventilation, loss of consciousness, and death. Severe hypercapnia generally occurs when the partial pressure of carbon dioxide is more than 75 mmHg.
3. Physiologic Compensation
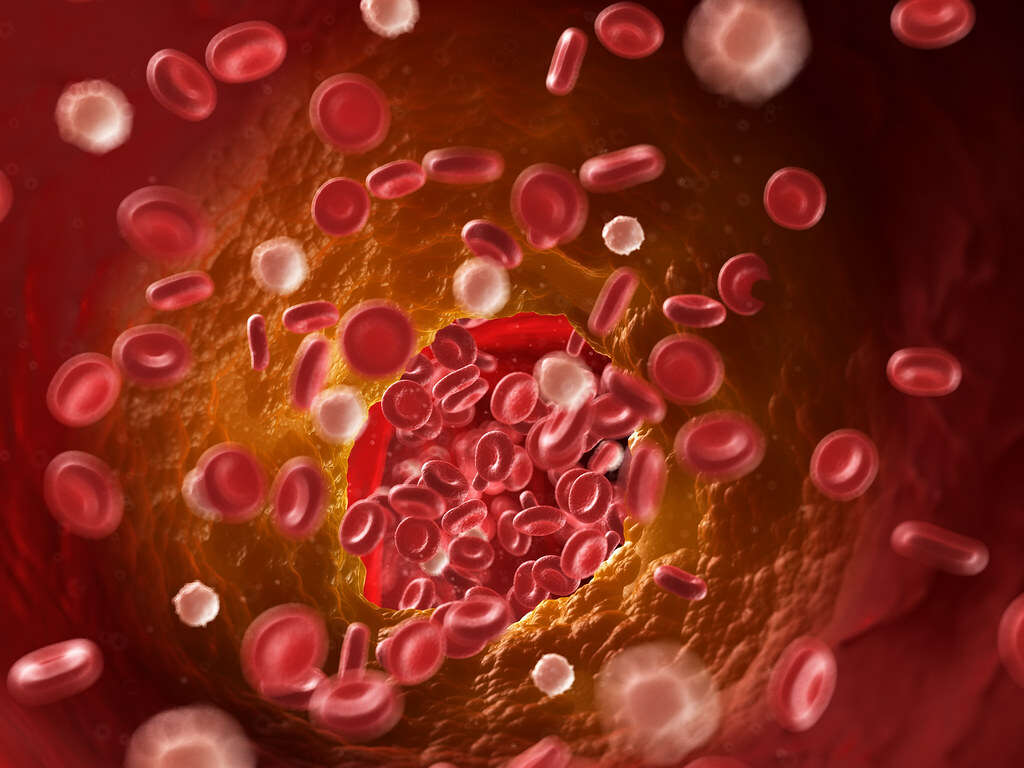
In normal cases, the metabolism of the carbohydrates and fats in the body results in a large amount of carbon dioxide. This then combines with water to become carbonic acid. This can be excreted via the lungs and accumulation does not usually occur. When hypercapnia occurs and is not corrected, it results in respiratory acidosis.
The body then tries to compensate in 2 steps. Cellular buffering first begins to increase plasma bicarbonate values. After 3 to 5 days, the kidneys compensate by excreting carbonic acid and increasing bicarbonate reabsorption. Respiratory acidosis does not usually greatly affect the serum electrolyte levels. However, small changes can be seen in potassium and calcium levels.
4. Causes
Hypercapnia can be caused by various conditions where there is decreased consciousness, hypoventilation, and lung disease. It may also occur when there is exposure to an environment where there is abnormally high levels of carbon dioxide.
This can occur when one rebreathes exhaled carbon dioxide or is caught in an area where there is geothermal or volcanic activity. Acute hypercapnic respiratory failure can occur when there is acute illness such as neuromuscular disease, chest wall deformity, and chronic obstructive pulmonary disease (COPD). It can also occur when the breathing muscles are weakened like in acute severe asthma, severe pneumonia, or depression of respiratory center due to drug abuse.
5. Chronic Obstructive Pulmonary Disease
Chronic obstructive pulmonary disease (COPD) is a term to describe a condition where there is difficulty breathing due to obstruction to respiratory outflow. COPD is most commonly caused by tobacco use or inhalation of harmful air due to pollution or occupational hazard.
With time, the irritants in the lungs cause scarring and fibrosis resulting in the loss of elasticity in the air sacs (alveoli) of the lungs. This means that the lungs are no longer as efficient. COPD also causes inflammation to the airways leading to the excessive production of mucus. This makes it even harder to breathe. As the scarring and inflammation prevents proper air flow, the body is unable to expel carbon dioxide leading to its accumulation. Although not all COPD patients will get hypercapnia, the progression of the disease makes it more likely to occur.
6. Risk Factors
Risk factors of hypercapnia, especially due to COPD, are individuals who smoke or use tobacco heavily, those with asthma (especially those who also smoke), individuals who live or work in environments where they breathe in fumes or chemicals (such as chemical plants, electrical plants, warehouses, and factories), and age (as hypercapnia generally only shows symptoms after the age of 40 years old).
Other risk factors include those who are obese, have sleep apnea, pulmonary embolus, nerve and muscular issues (such as muscular dystrophies or Guillain-Barre syndrome), positive family history, and those with genetic causes such as those with alpha-1 antitrypsin deficiency syndrome.

7. Diving and Hypercapnia
In diving, normal respiration results in inadequate elimination of carbon dioxide, resulting in hypercapnia. This is due to the variety of reasons where the carbon dioxide is not expelled completely during exhalation. For example, the diver exhales into a vessel where the carbon dioxide does not escape to the environment resulting in reinhalation.
Another reason is over-exercising leading to increased carbon dioxide because of elevated metabolic activity. The carbon dioxide scrubber may also not be sufficient to remove carbon dioxide. Because the density of the breathing gas becomes higher as the diver dives deeper, there is more effort to inhale and exhale, causing breathing to become more difficult. Divers may also be “skip breathing” in an effort to conserve breathing gas. All these reasons contribute to the possibility of hypercapnia in divers.

8. Diagnosis
As in any condition, patient history and physical examination plays a crucial role in the diagnosis of a disease. In acute illness, blood gas tests can be performed through a blood sample collected from the radial artery. This test helps to measure the carbon dioxide and oxygen levels in the blood. Chemistry panels such as electrolytes and bicarbonate levels may also be useful. A complete blood count can also be performed.
Other potentially beneficial tests include thyroid function tests, toxicology screens, creatine phosphokinase test, and medical imaging to ensure there are no physical issues with the lungs, brain, and spinal cord.

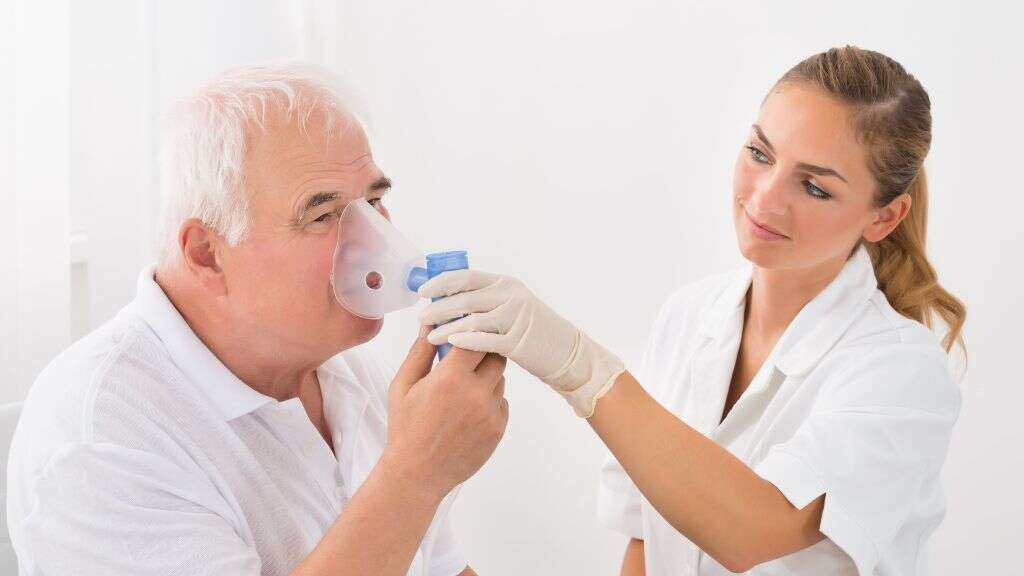
9. Treatment and Management
The treatment and management of a patient with hypercapnia depends on the underlying issue. In acute illness, stabilization of the patient is the most important. It may involve mechanical respiratory support and medications. Non-invasive ventilation (face mask or nasal mask) is generally preferred over invasive mechanical ventilation (endotracheal tube or tracheostomy tube).
In very severe cases where there is respiratory failure due to hypercapnia, extracorporeal membrane oxygenation (ECMO) where carbon dioxide is removed and oxygen added to the blood may be done. Another technique known as the extracorporeal carbon dioxide removal where carbon dioxide is removed may be indicated. This technique requires less blood flow volume compared to the ECMO technique.

10. Patient Education
Prevention of hypercapnia includes increasing patient compliance for the management of existing medical conditions such as COPD. This means taking medicine and following guidelines such as using supplemental oxygen as directed. It is best to decrease the use of sedatives and narcotics and use only as directed. Any side effects should be reported.
Those who are on supplemental oxygen at home may find it beneficial to have a fingertip pulse oximeter to monitor their oxygen levels. They may also ask to consult with a physical, occupational, or respiratory therapist on breathing techniques to help clear carbon dioxide more efficiently. Always seek medical attention when there are symptoms such as breathlessness, lethargy, and confusion. Maintaining a healthy lifestyle by having a good diet, regular exercise, no smoking, and having regular follow-ups with the doctor is also recommended.