What Is Horner's Syndrome?
Horner’s syndrome is a medical condition that impacts the face, specifically the area around the eyes. Though there are rare cases of a child being born with other types of this syndrome, the condition usually manifests in a person due to particular factors. It typically impacts one side of the face and is characterized by an eye that appears slightly sunken into the skull with a drooping eyelid and pupil that has decreased in size. The side of the face that has been impacted will also stop producing sweat.
Learning more about Horner’s syndrome can be invaluable in spotting the symptoms in yourself or someone you care about. By responding fast to the early signs, it is possible to explore treatment options and reduce the odds of the condition doing lasting damage.
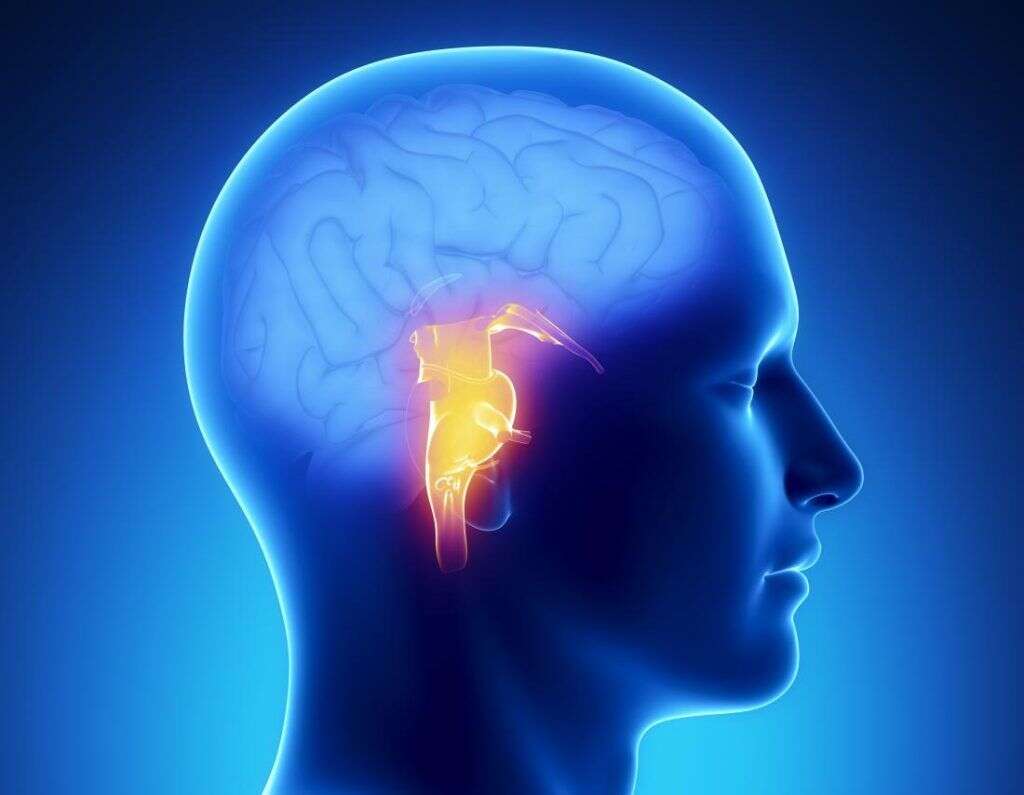
1. Nerve Pathways and Horner’s Syndrome
When the nerve pathways that run to and from the eyes become obstructed, it creates the conditions for Horner’s syndrome to develop. An obstruction like a tumor, lesion, or similar growth can interrupt the sympathetic nerve supply. This, in turn, decreases the overall function of the nerve and leads to the shifted position and decreased size of the eye. While the obstruction is what causes the disruption in nerve function, the underlying cause must be determined to find the most appropriate treatment for the condition.
Professionals believe there are a number of specific factors that can lead to the development of Horner’s syndrome. Unfortunately, research suggests that the condition can also come about for reasons that have not yet been adequately studied.

2. Causes of Horner’s Syndrome
Horner’s syndrome is usually the result or symptom of another issue in the body. More often than not, it occurs because a tumor or growth has formed within the chest, neck, or lungs. A Pancoast tumor is often to blame, which is a type of growth that develops in the upper part of the lungs. While the chest is one area where conditions can lead to Horner’s syndrome, the brain can also be the source. Any growth or lesion that develops along the stem of the brain or spinal cord could lead to it.
Some reports have pointed out that inflammation may lead to the development of Horner’s syndrome. When the lymph nodes become swollen due to overactivity, the inflammation can disrupt the pathways of the nervous system.
3. Horner’s Syndrome and Accidents
Though the development of a tumor in the lungs or brain stem can lead to the development of Horner’s syndrome, there are several other causes of which to stay mindful. A stroke can also be a leading factor, especially one that has a direct impact on the neural pathways connected to the eyes. A particularly bad car accident might also cause the condition. This is especially true of any accident that results in physical injury to the head, neck, spine, or chest. Surgery on any of these areas may also lead to the development of this syndrome.
There is no specific treatment for the syndrome itself. Instead, medical professionals must know what conditions led to the development of the neural obstruction.

4. Horner’s Syndrome and Genetics
While there are a number of factors that can lead to the development of Horner’s syndrome, many researchers also believe it can come down to genetics in some individuals. Several studies suggest that certain people are more susceptible to obstructions in the neural pathways connected to the eyes because of abnormal genes inherited from a parent. A person who experiences this condition at some point is about 50% likely to pass that gene on to offspring. Still, genetics are only one factor. This syndrome can also develop idiopathically without a clear reason.
Visiting with a doctor as soon as symptoms begin to develop is the best way to determine whether you’re dealing with Horner’s syndrome and how best to discover the cause. Your physician may also suggest certain treatments to help you handle symptoms or pain.
5. Children and Horner’s Syndrome
Though it is considered rare, there are cases where children are born with Horner’s syndrome. It is often apparent right from birth or begins to show within the first weeks or months of development. Most of these cases are due to complications during the delivery where the baby’s neck or shoulders are injured. A genetic defect on the aorta that some babies are born with can also lead to an obstruction in the neural pathways of the eye. In very rare cases, a tumor in a child’s nervous system may be the cause.
While a doctor should be aware of the condition if a child shows symptoms right away, not all children exhibit Horner’s syndrome immediately. Contact your pediatrician as soon as you notice any signs or symptoms.

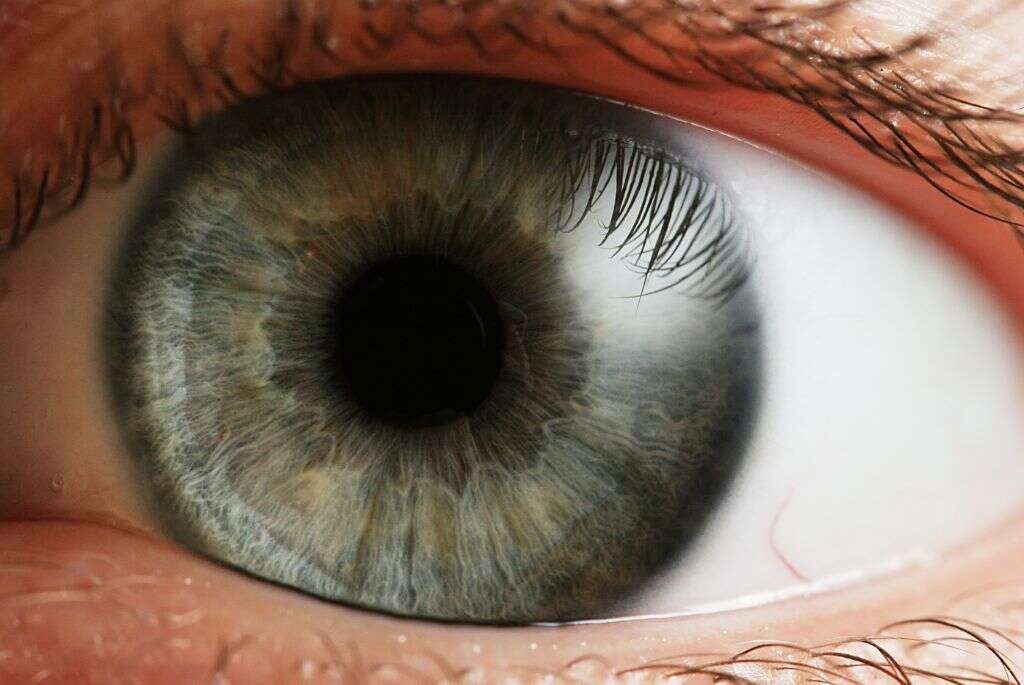
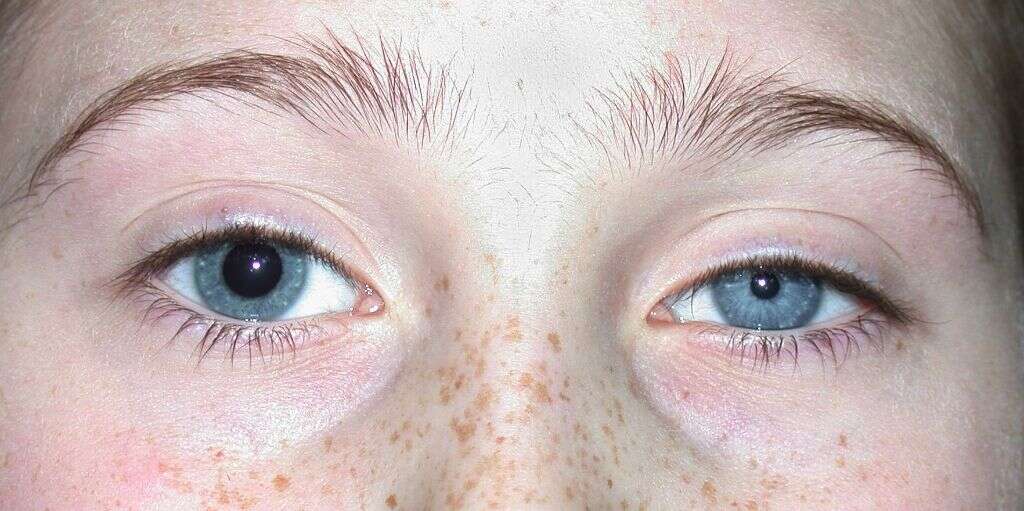
6. Common Symptoms of Horner’s Syndrome
Horner’s syndrome manifests around the eye on one side of the face in several specific ways. The size of the pupil shrinks and remains small, which can be apparent when compared to the size of the other eye’s pupil. The pupil may also have delayed responses with dilation or not change at all when light conditions shift. The eyelid of the impacted eye also droops significantly, which obstructs vision and is noticeable to others. The lower eyelid may seem somewhat elevated and make the eye appear slightly more closed than usual.
A person with Horner’s syndrome is likely to experience all of these symptoms around the eye. In addition, the side of the face that has been impacted no longer produces sweat. This dryness can be easy for a person to notice, especially in humid climates or during tense situations.
7. Severe Symptoms of Horner’s Syndrome
While most of the initial signs of Horner’s syndrome are subtle, the overall impact grows as the condition worsens. Since some of the early warning indicators are hard to notice, you may not even realize there is a specific problem to address. Unfortunately, there are further telltale signs that can help you understand what you’re dealing with.
If the condition gets worse, you may start to experience significantly impaired vision and a general sense of dizziness as your eyes struggle to adjust to the impairment. People who develop Horner’s syndrome also mention experiencing cluster headaches, migraines, and neck pain. A lack of muscle control or a feeling of weakness in muscle groups can also be an indication. If you or someone you love is experiencing any of these symptoms, consult with an emergency specialist as soon as possible.

8. Diagnosing Horner’s Syndrome
If you are exhibiting the symptoms associated with Horner’s syndrome, you are likely curious about how a doctor can diagnose you. If you’ve noticed earlier signs, then visit your optometrist. He or she can more accurately identify the condition and refer you to an ophthalmologist for more involved tests. These specialized eye doctors look at your ocular nerves and try to find any damage. If damage is found, the ophthalmologist needs to run tests to discover the root of the issue. This can involve an MRI, blood tests, and X-rays.
If you have any useful information that may be related to the condition, such as recently being in an accident or suffering a stroke, remember to share it during the appointment. This provides invaluable data to your doctor and informs the decisions he or she makes.
9. Treatment of Horner’s Syndrome
Unfortunately, there is no direct treatment to address Horner’s syndrome. This is largely due to the fact that it is most often a symptom of a more pressing medical issue. Once you have received a diagnosis from a medical professional, you will be introduced to the most appropriate treatment options. If the condition is the result of a tumor, for example, the doctor may suggest treatment to shrink it with radiation or remove it through surgery. For those who develop Horner’s syndrome as the result of family history, genetic therapy could prove to be a viable treatment.
In most cases, the symptoms related to Horner’s syndrome begin to decrease once the cause is addressed and treated. The specifics vary depending on your condition, so your doctor can provide more information on your individual timeline should you require one.

10. Horner’s Syndrome Outlook
Horner’s syndrome is a condition that can develop in very subtle ways and be a symptom of a much more threatening health risk. Though it may not be possible to get treatment for Horner’s syndrome itself, discovering the root of the issue can provide a person with a number of options for therapy. The most important thing to do is take note of the symptoms as they develop, even if those symptoms seem quite mild. If you’ve been in an accident or suffered a stroke, stay extra mindful of your eyes and pay close attention to the size of your pupils.
As soon as symptoms develop or persist, visit with a doctor. For mild symptoms, see an optometrist and learn if Horner’s syndrome is what you’re dealing with. Anyone experiencing severe symptoms should seek more immediate medical attention right away.