What Is Empty Sella Syndrome?
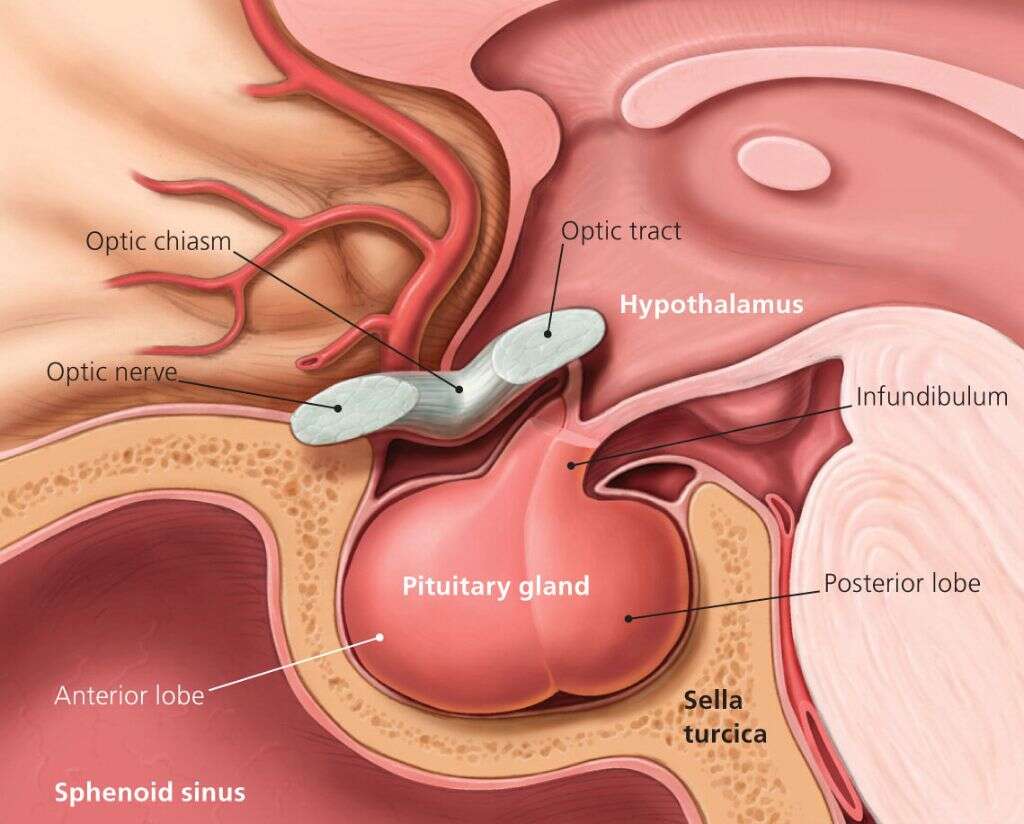
The pituitary gland sits in an area of the skull known as the sella turcica, a small indentation in the sphenoid bone at the base of a human skull. Empty sella syndrome refers to the visible absence or flattened appearance of the pituitary gland in MRI imaging. However, the sella turcica is not empty at all; it is entirely or partially filled with cerebrospinal fluid.
A diagnosis of any condition, or a concern over its potential development, is disheartening and worrisome. Most people do not have a common knowledge of diseases and medical disorders, especially rarely diagnosed conditions like empty sella syndrome. It is natural for potential and diagnosed patients to have many questions about treatments, causes and potential cures. The following 10 questions can answer the most pertinent questions about this disorder and hopefully put your mind at ease.
1. What Are the Signs and Symptoms of Empty Sella Syndrome?
Most people with empty sella syndrome are asymptomatic, meaning they show no symptoms of the condition. However, a few patients may suffer from chronic headaches, vision problems or spinal fluid leaking from the nose. The condition leads to increased cranial pressure, which is likely the reason for headaches. The disorder can also cause swelling of the optic nerve, leading to blurry vision. However, researchers explain that some of these symptoms, like headaches, may link to high blood pressure, which is common in empty sella patients.
While any physical symptoms are rare, there are at least two more associated problems that are even rarer. Some patients suffer from vertigo or dizziness, and, in the most unique cases and likely in combination with another diagnosis, empty sella patients may experience seizures. Again, the likelihood of having any of these symptoms is low as patients with this condition are typically asymptomatic.
2. What Causes This Condition?
Primary empty sella syndrome has no known causes. The current hypothesis is that it results from a congenital disability in the diaphragma sellae, the membrane covering the sella turcica. Researchers believe that some people are born with a tear in the membrane, allowing cerebrospinal fluid to leak into the sella turcica. However, there is no definitive causal link, meaning that a torn diaphragma sellae may only present a higher risk of developing the condition.
Unlike primary empty sella syndrome, doctors know that secondary empty sella syndrome results from another condition. For example, patients who experience head trauma, infection or pituitary tumors may develop this disorder. Multiple underlying brain or pituitary syndromes, like intracranial hypertension or hypophysitis, also present a higher risk for developing empty sella syndrome.
3. How Is Empty Sella Syndrome Diagnosed?
Most patients with empty sella syndrome go their entire lives without experiencing any symptoms, making the condition difficult to diagnose. If you are exhibiting a particular combination of symptoms, your doctor may suspect the condition. However, before giving a diagnosis, physicians will perform a physical exam. They will also do a thorough review of your medical history to rule out any other potential conditions.
After reviewing your history and completing a physical, your doctor may order MRI or CT scans to confirm the suspicion. Either of these scans can show a clear picture of the sella turcica and the pituitary gland. From the images, your physician can tell if there is cerebrospinal fluid present in the cavity and also see how much cerebrospinal fluid is in the sella turcica, providing you with a diagnosis of partial or total empty sella syndrome.
4. What Are the Standard Treatments and Therapies?
Treatment is likely unnecessary for primary empty sella syndrome, as long as there are no noticeable symptoms. For those who do experience symptoms, there are a couple of treatment options: surgery and medication. Doctors typically reserve surgery for patients suffering from cerebrospinal fluid leaking from their nose. Medications are typically just pain relievers for headaches.
A diagnosis of secondary empty sella syndrome is different. When the condition directly results from another ailment, your doctor may seek to treat the underlying cause. For example, a doctor can treat head trauma that caused the syndrome to develop. Sometimes, the treatment or therapy used for the underlying condition can limit the severity of the corresponding empty sella syndrome. However, sometimes the syndrome remains even after the correction of the primary issue.

5. Are There Any Life-Threatening Complications of Empty Sella Syndrome?
Empty sella syndrome is not life-threatening in itself. People with a primary diagnosis do not experience any reduction in life expectancy, and they will probably never show signs or symptoms. Yes, having a diagnosis of any medical condition can feel scary, but this illness is nothing to worry about, especially with a primary diagnosis. Live your best life, and don’t concern yourself with unnecessary stress.
A secondary empty sella syndrome diagnosis may be a little more concerning, depending on the primary condition responsible. It is impossible to list all possible conditions and the potential complications because of the spectrum and variety of traumas. However, people likely experience minimal problems or trauma from the syndrome itself. Any pain or suffering is likely the result of the underlying condition and not the empty sella syndrome.
6. Are There Any Genetic Markers or Hereditary Characteristics of This Condition?
Empty sella syndrome is not hereditary. The current research does not show any genetic links for the development of this condition. Most researchers believe the illness stems from a congenital disability in the membrane surrounding the sella turcica. However, there is no confirmation of this hypothesis, meaning the true cause and links to developmental issues is purely speculative and hypothetical.
The rarity of diagnoses for this condition means that definitive explanations are far off. The limited pool of patients equates to limited data. However, as this condition is not often diagnosed because of the absence of symptoms in many patients, it is difficult to even define the syndrome as rare.

7. What Percentage of the Population Has This Disorder?
Researchers estimate that up to 25% of the population may have empty sella syndrome. However, it is challenging to narrow this percentage down to a precise number. Not everyone with the condition gets tested or diagnosed and only 1% of people with it may experience symptoms, making it likely that the vast majority of people who have the syndrome do not even know it and will never find out.
Doctors and researchers base their numbers on available data, meaning experts base their opinions only on those patients that present with symptoms and receive a diagnosis. Therefore, while the rare illness classification stands for empty sella syndrome, it is impossible to know the exact number of affected individuals. While that news may seem troubling, unlike many other conditions, empty sella syndrome rarely inhibits or impacts the life of affected patients.
8. What Are the Risk Factors?
Women are four times more likely to develop empty sella syndrome than men. Most diagnosed women also present with underlying issues like obesity and high blood pressure, and the diagnosis or presentation of symptoms typically occurs in middle age. However, as the condition is rarely diagnosed and most patients do not present with symptoms, it is hard to say that gender, age, blood pressure and obesity are risk factors, especially for primary empty sella syndrome.
The consensus is that you may minimize the risks of empty sella syndrome, like any condition, through healthy lifestyle choices. Therefore, while obesity and high blood pressure may not contribute to the development of the illness, consuming a healthy diet is still enormously beneficial. While it is also not clear that habits like smoking affect the condition, tobacco use causes multiple health problems. Following fundamental health guidelines are always good ways to help ensure your physical fitness.

9. Can Empty Sella Syndrome Affect Growth and Development?
Empty sella syndrome affects the pituitary gland, which can lead to growth and developmental deficiencies. This condition may be correlated with developmental issues in children such as early onset of puberty, pituitary gland dysfunction, growth hormone deficiency or pituitary tumors. As the empty sella syndrome is likely secondary in these situations, a child may recover from any resulting deficiencies.
While there is a possibility of secondary empty sella syndrome leading to developmental issues with your child, if it is primary, the chances of such problems occurring are minor. Doctors stress that most patients are asymptomatic and enjoy a normal and healthy life.
10. Is There a Cure?
There is no cure for primary empty sella syndrome. The condition is often harmless and does not even require treatment. However, if you are presenting with symptoms, surgery may correct the problem. Patients suffering from secondary empty sella syndrome often experience relief of symptoms after receiving treatment for their underlying condition.
Empty sella syndrome is a rarely diagnosed condition, and it is not life-threatening. Most people who receive a diagnosis for the illness will never experience symptoms. However, for those who suffer from chronic headaches or nasal discharge, a doctor may suggest medications or surgery. If you believe you are showing signs of empty sella syndrome, speak with your physician and ask about a CT or MRI scan to confirm the diagnosis.
Related Articles
-
10 Symptoms of Pheochromocytoma
10FAQ
-
Nursing Degree: A Gateway To A Rewarding Career
10FAQ
-
Understanding LASIK Surgery for Improved Vision
10FAQ
-
Cheap Dental Implants: A Cost-Effective Solution For Your Dental Needs
10FAQ
-
Gallbladder Polyps Causes, Symptoms and More
10FAQ
-
10 Trigger Finger Symptoms
10FAQ





